Introduction
In 75-85% of cases of acute hepatitis C infection, the disease becomes chronic and carries a risk of developing liver failure and hepatocellular cancer (1). In its global hepatitis report published in 2017, the World Health Organization (WHO) reported that 71.1 (95% uncertainty interval [UI]: 62.1-79.0 million) million people were chronically infected with the hepatitis C virus (HCV) (2). On World Hepatitis Day 2022, this number was updated to 58 million; approximately 1.5 million new hepatitis C cases are reported every year (3). In studies conducted in Türkiye, anti-HCV positivity was found to be 0.5-1%, with the dominant genotype being genotype 1b (4-6). In recent years, there has been an increase in the rate of non-genotype 1 genotypes in Türkiye, as it is a country that has received intense immigration from neighboring countries where non-genotype 1 genotypes are common (7).
The sustained virologic response (SVR) rate achieved as a result of pegylated interferon and ribavirin combination treatment in cases infected with genotype 1, which is common in our country, remained at 40-50%. The addition of the first developed protease inhibitors, such as telaprevir and boceprevir, to the treatment could only increase the SVR to ~ 70% (8, 9). The introduction of direct-acting oral antivirals (DAAs), which have been used since 2015, has led to a significant increase in end-of-treatment and SVR rates across all genotypes, and treatment duration has been reduced to 8-16 weeks (10). While the first DAAs developed were effective against specific genotypes, pan-genotypic DAAs that are effective against all genotypes have been developed in recent years. One of these is a fixed-dose combination of the HCV NS3/4A protease inhibitor glecaprevir and NS5A inhibitor pibrentasvir.
Glecaprevir/pibrentasvir (G/P) is approved for use in all patients with HCV 1, 2, 3, 4, 5 or 6, without cirrhosis or with compensated cirrhosis (Child-Pugh class A). SVR rates of 91-100% were reported in the literature following treatment with G/P (11). The safety of G/P was evaluated in phase II and III clinical trials and real-world studies. Headache and fatigue were the most commonly reported adverse events. The proportion of people treated with G/P who permanently discontinued treatment due to adverse reactions was 0.1% (12-15). The COVID-19 pandemic, which started towards the end of 2019, created a major obstacle in the diagnosis and treatment of hepatitis C, as with many other diseases, both by increasing the burden on healthcare systems and by reducing hospital admissions of non-COVID-19 patients. In an online question survey conducted in the United States of America (USA) of respondents treating patients for HCV or hepatitis B virus (HBV) infection, 88% (59/67) and 80% (49/61) reported some level of disruption, and 39% (26/67) and 21% (13/61) reported a >50% decline in treatment volumes, respectively (16).
This study aimed to determine the efficacy and adverse events of G/P in chronic hepatitis C patients as real-life data and to investigate the negative role of the COVID-19 pandemic in patient follow-up.
Materials and Methods
The Viral Hepatitis Working Group planned the study under the umbrella of the Turkish Society of Clinical Microbiology and Infectious Diseases (KLİMİK). Researchers from universities or training and research hospitals took part in this retrospective study, with patients treated between October 2019 and October 2021. Patients with chronic hepatitis C who were over 18 years of age, treatment-naïve or treatment-experienced, had detectable HCV RNA and were receiving G/P treatment were included in the study. Patients with Child-Pugh class B and C cirrhosis or hepatocellular carcinoma, liver transplant patients, patients with medication use that interfered with treatment, and pregnant or breastfeeding women were excluded. Patients co-infected with HBV were not excluded. Since liver biopsy is not included in the reimbursement conditions of the Social Security Institution and patients generally do not want to undergo biopsy, a biopsy was not an inclusion criterion. Universal health insurance in Türkiye provides people with HCV full access to DAAs.
The aspartate aminotransferase (AST) to platelet ratio index (APRI) score was used to assess liver status and cirrhosis. The standard formula (APRI = (AST [U/L] / upper limit of normal AST [U/L]) × 100 / platelet count [109 /L]) was used to determine the APRI score. The APRI score was calculated by the center where the study was conducted, taking into account the last AST and platelet count before treatment. APRI score of ≤0.3 was classified as no cirrhosis or fibrosis, >0.3 and ≤0.5 as no cirrhosis and fibrosis possible, >0.5 and ≤1.5 as cirrhosis and fibrosis possible, >1.5 and ≤2 as cirrhosis possible and fibrosis, and >2 probable cirrhosis (17, 18).
The study was conducted in accordance with the tenets of the Declaration of Helsinki. Informed consent was obtained from patients, and the Health Sciences University Dışkapı Training and Research Hospital Clinical Research Ethics Committee approved the study on December 13, 2021, with decision number 126/21.
G/P was given at a dose of 300 mg / 120 mg/day (three 100 mg / 40 mg tablets) (Maviret; AbbVie Inc., Türkiye) for eight weeks in naïve patients and 12-16 weeks in treatment-experienced patients. Interactions between G/P and the patient’s concomitant medications were assessed, and recommended precautions were taken. HCV RNA levels were tested by polymerase chain reaction (PCR) at each center with a lower limit of quantification of ≤ 25 IU/mL. Patient demographics, HCV RNA level, genotype determination, presence of HBV co-infection, body mass index (BMI), previous treatment experience, basal AST, alanine aminotransferase (ALT), gamma-glutamyl transferase (GGT), albumin, total protein, total and direct bilirubin, hemoglobin, platelet levels, coagulation parameters (prothrombin time, international normalized ratio [INR]), and alpha-fetoprotein (AFP) levels were recorded. The results of the monitored parameters at baseline, at weeks 2, 4, 8 and 12 of treatment and at 12 weeks after the end of treatment were collected in Excel forms that were prepared and shared with the centers.
Undetectable HCV RNA at week four of treatment was defined as early virological response, undetectable HCV RNA at the end of treatment was defined as end-of-treatment response, and no HCV RNA was detected at 12 weeks after the end of treatment was defined as sustained virological response (SVR 12).
Statistical Analysis
The baseline data of the patients were calculated as mean±SD or median. Categorical data variables were presented as numbers, and ratios were expressed as frequencies and percentages. The baseline data relationships were analyzed by using the Student’s t-test and Mann-Whitney U-test or chi-square test. The statistical significance was set as p<0.05. The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 15.0 (IBM Corp., Armonk, NY, USA).
Results
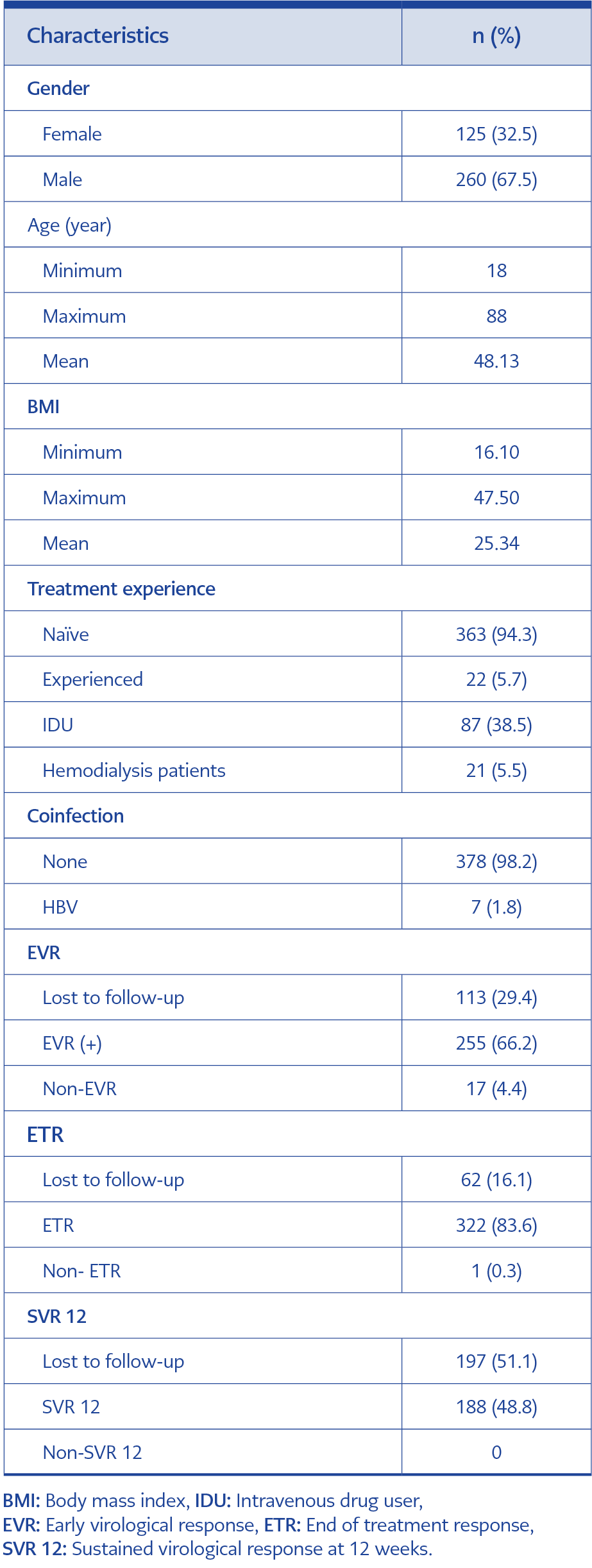
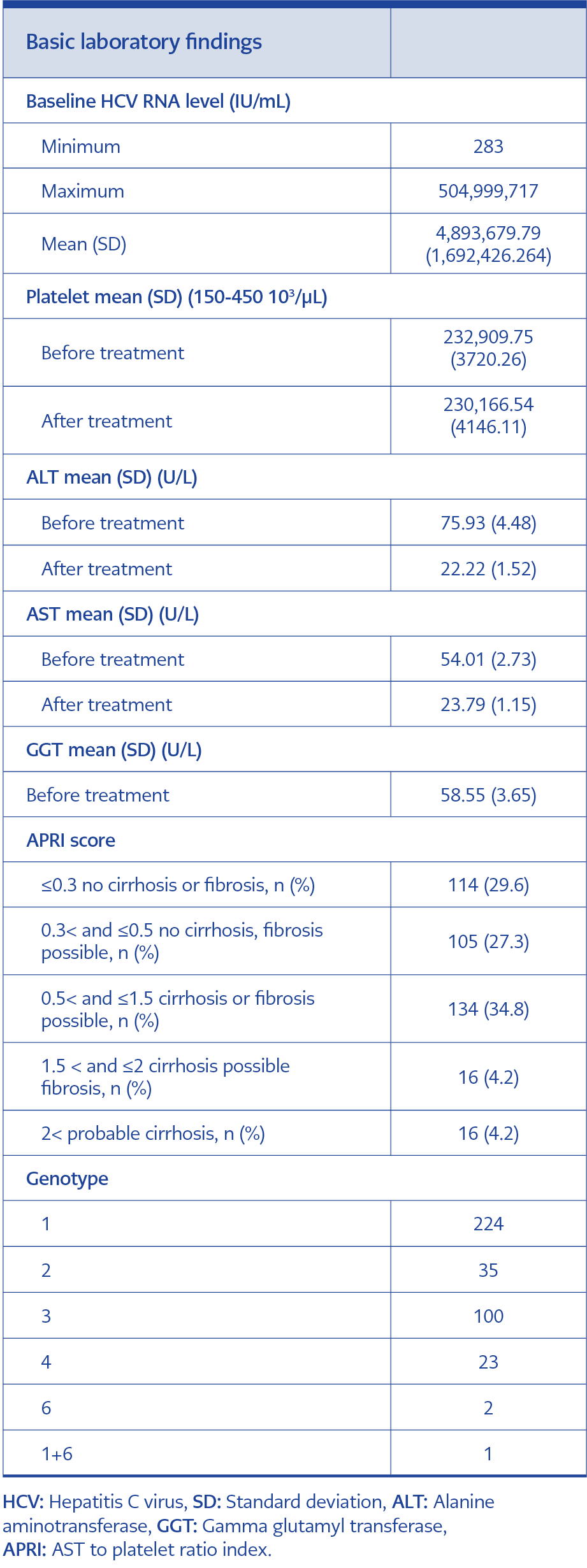
This study included 385 patients, of whom 262 were male (Table 1). Seven patients had HBV co-infection, but there was no human immunodeficiency virus (HIV) co-infection. While genotype 1 was the most common, genotype 3 was the second most common genotype (Table 2).
Eighty-seven patients (22.6%, 87/385) were intravenous (IV) drug users. Genotype distribution among IV drug users was as follows: 32 patients had genotype 1, eight had genotype 2, 39 had genotype 3, six had genotype 4, and two had genotype 6. Genotype 3 was significantly more common in IV drug users than in the general population (p=0.001). Twenty-one patients were on chronic hemodialysis. All patients’ liver disease severity was assessed using the APRI score (Table 2).
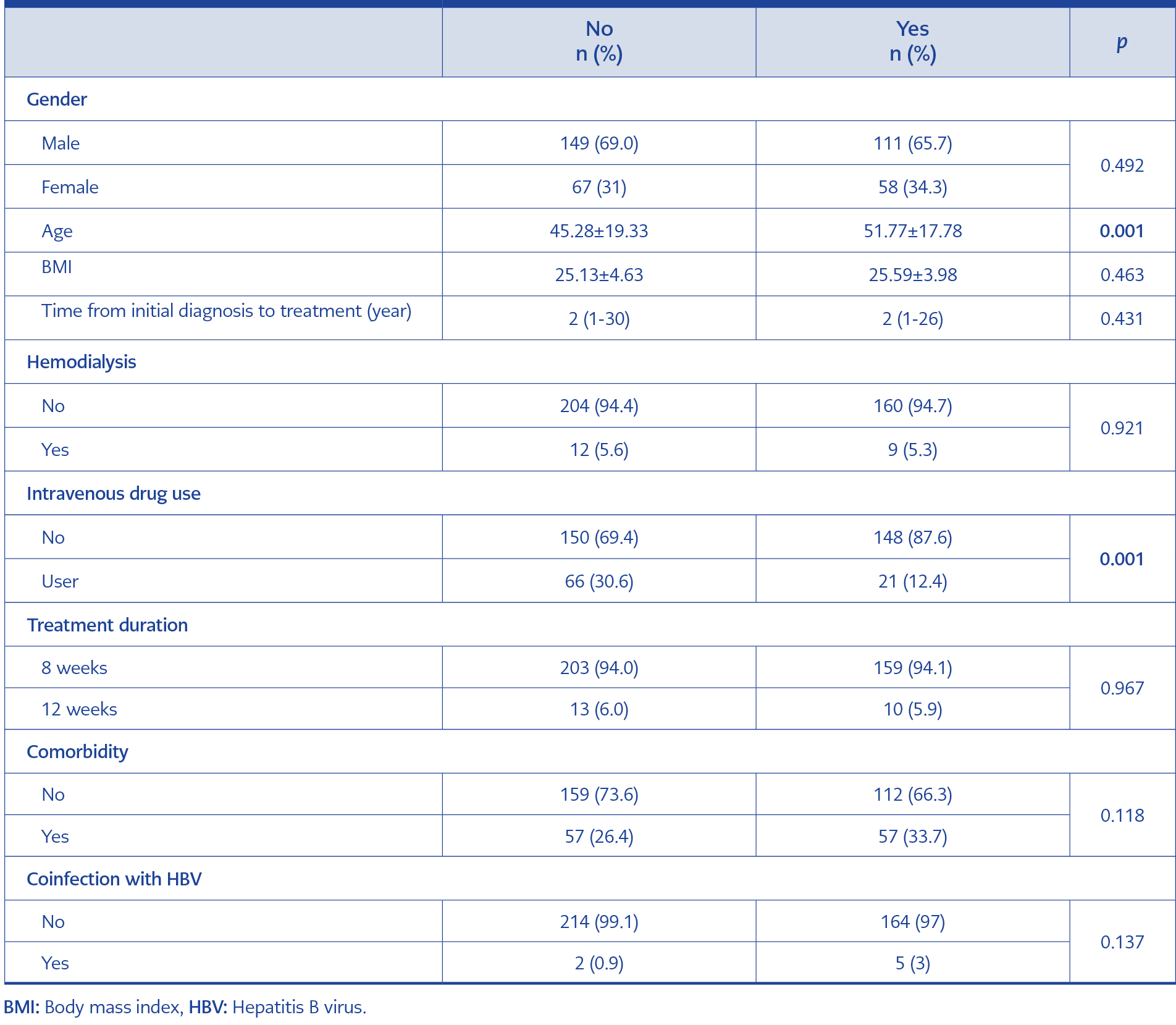
Table 3. Basic Characteristics of patients who attend regular follow-up visits and those who do not.
Twenty-two of the 385 patients were treatment-experienced, of whom fifteen received interferon + ribavirin, four received ombitasvir/paritaprevir/ritonavir plus dasabuvir, two received sofosbuvir + ribavirin, and one received sofosbuvir + ledipasvir. Three hundred sixty-three patients were treatment-naïve.
Patients were called for follow-up every month during treatment and in the third month after treatment. At the end of the first month, 272 out of 385 patients came to the follow-up visit, while the total number of patients who attended the follow-up visit was 323 at the end of treatment. One hundred eighty-eight patients attended the 12-week post-treatment follow-up visit where SVR 12 was assessed. In other words, 113 patients missed the follow-up visit at the end of the first month, 62 at the end of treatment, and 197 patients at week 12. It was found that the mean age of patients who did not return for follow-up and whose SVR was not checked at three months post-treatment was 45.28±19.33, while the mean age of those who returned for follow-up was 51.77±17.78 (p=0.001). The rate of loss to follow-up was higher among IV drug users (p=0.001) (Table 3).
Two hundred fifty-five out of 272 patients who attended the follow-up visit at the end of the first month showed an early virological response (93.8%, 255/272). BMI was lower in those with early virological response (25.23±4.28 vs 28.05±3.31, p=0.044). End-of-treatment response was achieved in all 323 patients who attended follow-up except one (%99.7, 322/323). In a 47-year-old female patient with an APRI score of 4.0 and genotype 1b, HCV RNA level was 167 IU/mL at the end of treatment, although HCV RNA was negative at the 4th week of treatment. Since HCV RNA was negative at the 12th and 48th week after treatment, this patient was considered to have a sustained virological response. It was thought that the HCV RNA level of 167 IU/mL at the end of treatment could be a laboratory error. Two patients whose HCV RNA could not have been quantified at the end of treatment had HCV RNA positivity below the detectable level. One of them was a 30-year-old man, and the other was a 70-year-old woman. The male patient had genotype 3 and an APRI score of 1.3, while the female patient had genotype 1b and an APRI score of 1.5. In these two patients who were prior-treatment- naïve, SVR 12 was achieved after G/P treatment. Sixty-two patients did not return for end-of-treatment follow-up.
Only 188 patients attended the 12-week post-treatment follow-up visit, and all had an SVR of 12. Per protocol efficacy analysis: 188/188 (100%), intention-to-treat (ITT): 188/385 (48.8%). Of the patients who achieved a sustained virological response, 13 were treatment-experienced patients.
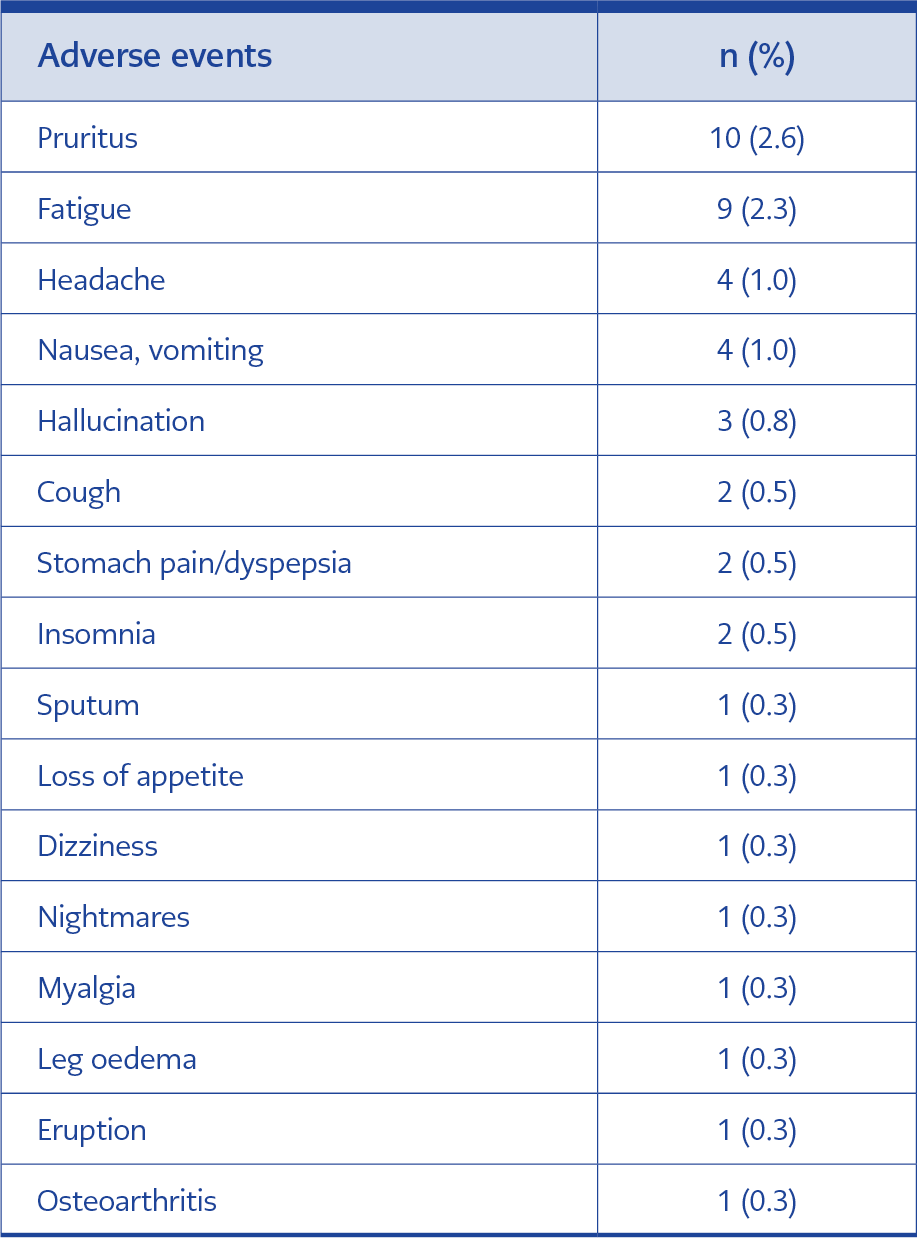
The most common adverse events were pruritis and fatigue, headache, nausea, and vomiting. These were followed by hallucinations, stomach pain/dyspepsia, and insomnia. Sputum, loss of appetite, dizziness, nightmares, myalgia, leg oedema, eruption, and osteoarthritis were less common adverse events (Table 4). Among the patients who could be followed up, no patient had to discontinue treatment due to adverse events.
Discussion
Around the world, the COVID-19 pandemic has disrupted essential health services needed to support the prevention, diagnosis and treatment of hepatitis C, as well as other chronic viral diseases. Responses to the pandemic, including stay-at-home orders, travel restrictions, physical distance requirements, and supply chain disruptions, disrupted essential healthcare services in many places and threatened to halt or reverse the progress made (19). The first case of COVID-19 in Türkiye was diagnosed on March 11, 2020, when the WHO declared the COVID-19 pandemic. On March 20, 2020, the Ministry of Health took new measures to minimize the pressure on healthcare providers and reduce the burden on healthcare workers. All hospitals were designated as pandemic hospitals.
Delays in healthcare during the pandemic can lead to delays in diagnosis and treatment, leaving people living with hepatitis C unaware of their disease status and vulnerable to the progression of advanced liver disease, including cirrhosis and hepatocellular carcinoma, and the potential spread of the virus. In the study by Gamkrelidze et al. in Georgia, the total number of people screened for anti-HCV decreased by 25.5% in 2020 compared to 2019, 59% fewer people were treated (3188 vs. 7868), and 46% fewer people achieved SVR (1345 vs. 2495) (20). A study by Kaufman and colleagues investigating the impact of the COVID-19 pandemic on hepatitis C testing and treatment found that, compared to 2018 and 2019, the volume of HCV antibody testing decreased by 59% in April 2020, and the number of positive results for HCV RNA decreased by 59% in March 2020. They also found that prescriptions for HCV treatment decreased by 43% in May, 37% in June, and 38% in July compared to the corresponding months in 2018 and 2019 (21).
In the study by İskender from Türkiye, comparing patient applications in a tertiary care teaching hospital in the pandemic and pre-pandemic periods, there was a 49.45% decrease in hepatitis B applications and a 55.5% decrease in hepatitis C applications (22). In our study, 113 of the 385 (29.4%) patients who started treatment did not return for follow-up in the first month. The number of patients who did not return for follow-up at the end of treatment was 62 (16.1 %). The number of patients who did not return for a 12-week post-treatment visit was 197 (51.2%). Thirty-four (8.8%) patients were never admitted to hospital after starting treatment. While the American Association for the Study of Liver Disease (AASLD) believes that chronic HBV and HCV patients should continue antiviral treatment during COVID-19 infection, they do not recommend starting chronic HBV and HCV treatment during COVID-19 infection (except for patients at risk of HBV reactivation) (23, 24).
In multicenter studies with real-world data, G/P efficacy was found to be between 96.9% and 99.3% in per-protocol analyses, and in the guidelines, it is recommended as one of the first treatment options in treatment-naïve and treatment-experienced chronic hepatitis C patients. (14, 15, 25-27). In this study, according to the ITT analysis, the efficacy of G/P treatment is 48.8% (188/385), and when per protocol analysis is performed, it is 100% (188/188).
In studies conducted before the pandemic, loss to follow-up rate was found to be between 2% and 5% (14, 15, 26). In the study conducted by Demirtürk et al., which was published in 2021, the rate of loss to treatment follow-up in patients using sofosbuvir/ledipasvir, with or without ribavirin, was found to be 4% (22 out of 552 patients). This study was performed before the pandemic, and patients were recruited from centers similar to those in our current study (28). In our study conducted during the pandemic period, this rate is 51.2%. Such a high rate of loss to follow-up may be significantly linked to the pandemic. The rate of loss to follow-up was higher among IV drug users (p=0.001). The study conducted by Cooper et al. showed that the COVID-19 cohort demonstrated significantly lower therapy completion rates (p=0.001), were less likely to obtain SVR laboratory tests (p<0.001), and had a significantly lower confirmed SVR rate (p<0.001) compared with the pre-COVID-19 cohort (29).
A total of 44 adverse events were observed in 31 patients (8%, 31/385). None of the adverse events led to patient death or discontinuation of treatment. Previous prospective studies reported adverse event rates between 20% and 28% (14, 25, 26). A retrospective study by D’Ambrosio et al. reported an adverse event rate of 8%, which is similar to our results (15). The lower rate of adverse events reported compared to previous prospective studies may be due to the decrease in the number of patient visits because of the pandemic and the retrospective study design.
Because all patients responded to treatment according to per-protocol analysis, the effect of different genotypes or being treatment-naïve or experienced on treatment outcome could not be evaluated. Secondary results of the study include genotype 3 being more common in IV drug users, lower BMI in those with early virological response, and lower mean age in those who did not attend treatment follow-up visits. The rate of no follow-up was higher among IV drug users.
Since this study was conducted retrospectively and included real-life data, it has some limitations, such as insufficient data collection, inadequate reporting of side effects, and laboratory data being studied separately in each center.
In conclusion, G/P treatment in chronic hepatitis C patients has very high treatment success and relatively low adverse events. However, disruption of services to patients with viral hepatitis during the pandemic period caused undesirable consequences, such as a decrease in the number of newly diagnosed patients, disruption of follow-up of newly diagnosed patients, delay in treatment of patients who need treatment, and disruption of follow-up of patients who are receiving treatment. New measures are needed for the follow-up and treatment of patients with chronic hepatitis C during pandemics.