Introduction
Reprocessing a disposable medical device in which sterility deteriorates without contact with the blood and body fluids is called “reprocessing.” If it is ready for use by being processed again for the same or another patient, it is named reuse. The increasing number of blood-borne diseases led to the broader use of disposable instruments. Cardiac catheters, percutaneous transluminal coronary angioplasty (PTCA) catheters, and arterial catheter needles are the primary reused disposable critical tools (1). As sterilization techniques improved, reprocessing and reusing single-use instruments became a reality due to economic and environmental concerns, especially in developing countries (2, 3).
Nevertheless, reprocessing and reuse are less common in developed countries. France and England do not allow reuse for patient safety and technical reasons. In contrast, the USA, Canada, and some European countries allow in limited cases considering ethical and legal issues, personnel training standards, risk assessment, and management of the sterilization process. Reuse rates of critical tools are high in Brazil and Asian countries (2, 4). In Turkey, reuse is forbidden formally but allowed only under the user’s responsibility (5, 6).
Although studies show widespread reprocessing and reuse of critical disposable instruments, there is no standardized procedure in the hospitals where the application is performed (7). Cleaning is crucial in tools with narrow lumens, such as cardiac catheters (8). Reprocessing and reuse, leading to ineffective sterilization, can cause many issues, such as endotoxin reaction and deformation in medical instruments. Therefore, manufacturers may be unwilling to share the responsibility of reprocessing (1-3). Ethylene oxide (EO), hydrogen peroxide (HP), and peracetic acid solutions sterilize disposable instruments such as PTCA catheters. EO, a low heat sterilization method with good penetration power, has no limit for lumen diameter and length for the devices used, but HP causes minimal damage on instrument surfaces (9).
In our study, we aimed to show the structural changes on the covers of PTCA catheters depending on different sterilization types and the number of reprocessing procedures via electron microscopy.
Materials and Methods
A total of five PTCA catheters (InvaderTM PTCA; Alvimedica Inc., İstanbul, Turkey) were studied. One catheter was not processed to serve as the control. A total of four catheters were processed after being used once in patients. Two catheters were treated with EO, one five times and the other more than five. Likewise, two catheters were treated with HP, one five times and the other more than five. The effects of HP and EO gas plasma sterilization on the surface of four PTCA catheters and the control were examined by scanning electron microscope (SEM). Each catheter sample was randomly divided into four parts to represent the whole during SEM evaluations; 20 pieces were examined. Catheters were reprocessed through every regular sterilization step, used solely for study, and not reused in patients.
Each piece 10 mm in length was prepared in sterile conditions and then covered with gold-palladium 10 nm thick before performing SEM evaluation. Samples were examined using a JEOL JSM-7001F electron microscope in the Black Sea Advanced Technology and Research Center (KİTAM) at Ondokuz Mayıs University, Samsun, Turkey. The surface features of the samples were examined first at x2500 magnification and then at x7500 magnification for further evaluation.
Statistical evaluations of histological scoring made on images obtained from scanning electron microscopic images were made using the GraphPad Prism 8 (GraphPad Software, Boston, USA) program. The Kruskal-Wallis test was used for intergroup comparisons. The statistical significance was set as p>0.05.
Results
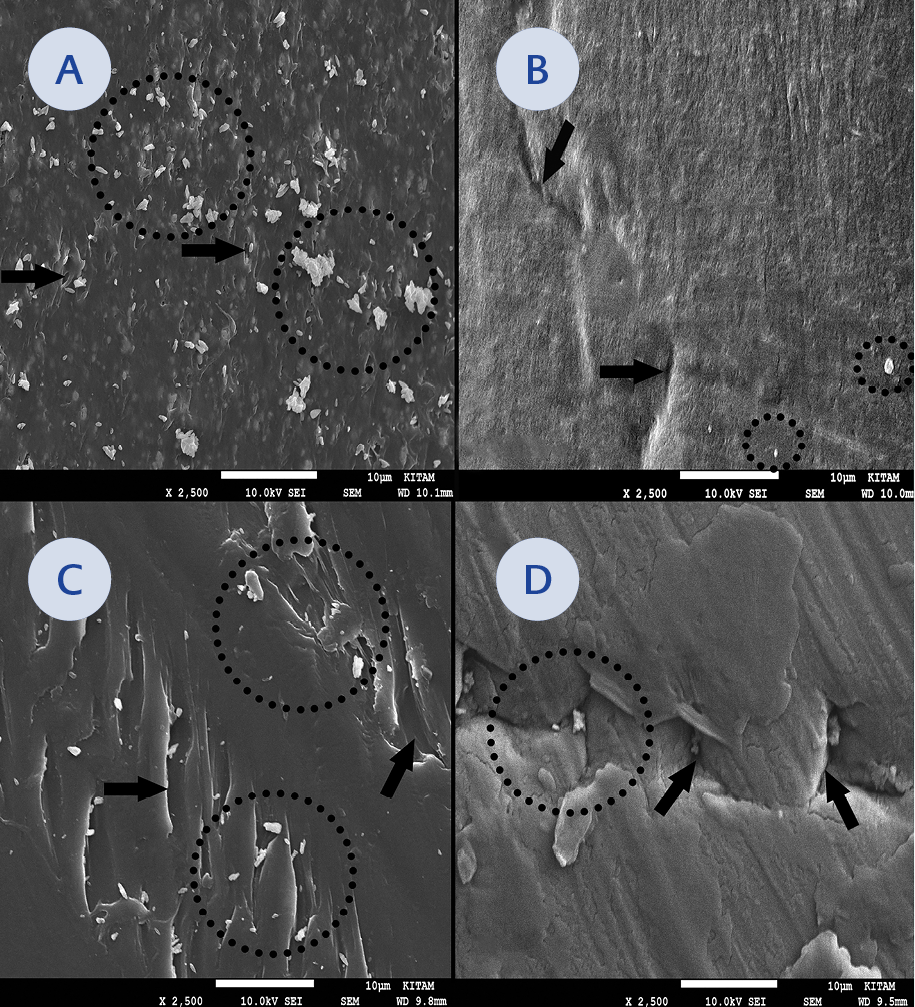
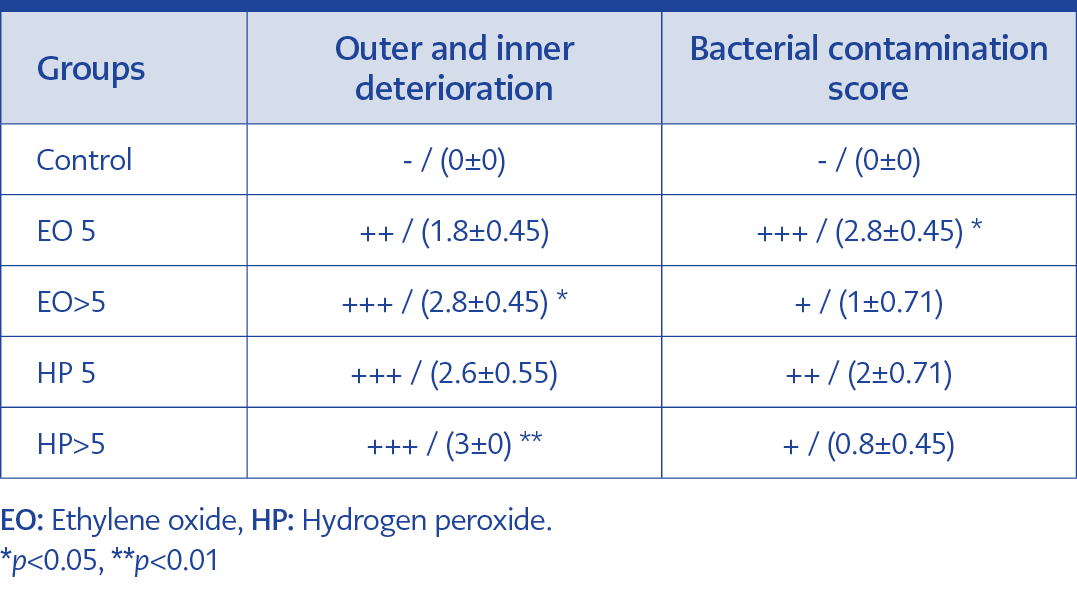
Figure 1. (A-D) Outer surface examination. Detrimental effects on ethylene oxide and hydrogen peroxide: Five cycles (EO5) (A), (HP5) (C), and more than five cycles (EO>5) (B), (HP>5) (D). Dotted circles indicate bacterial growth in relevant areas. Arrows indicate the deterioration in surface area (SEM images, x2500 magnification).
Sixteen PTCA catheter pieces were treated with HP or EO; then, the treated pieces and control pieces were examined by SEM. Electron microscopic observations (Figures 1-3) showed that in EO, no apparent damage was observed within five cycles at x2500 magnification (Figure 1A); however, damage was detected at x7500 magnification (Figure 2B, 2C). Both types of reprocessing caused cracks and crevices on the samples’ inner and outer surfaces. Regarding outer surface examination, significant damage was noted after five sterilization cycles with HP (Figure 1C). More than five HP sterilizations resulted in more damage (Figure 1D).
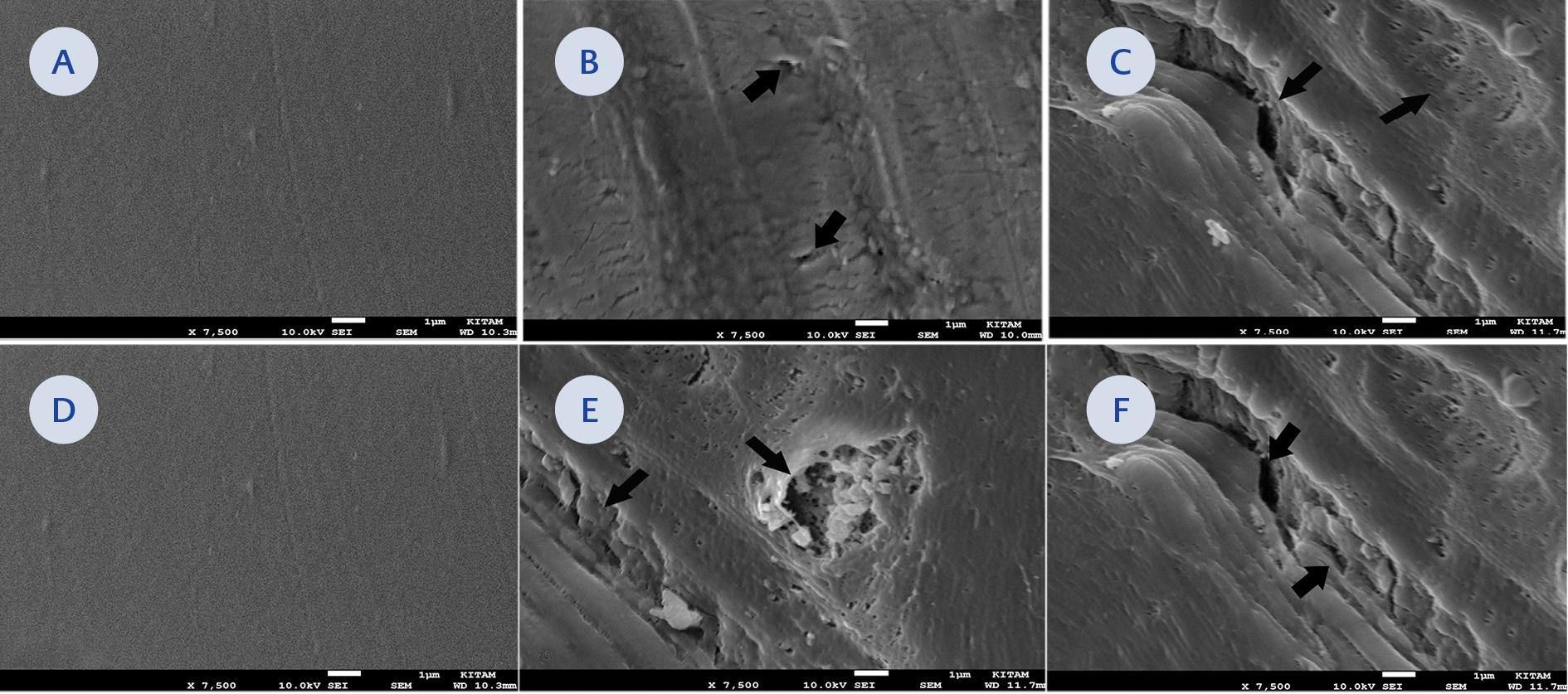
Figure 2. (A-F) Outer surface examination. (B, C, E, F) Detrimental effects on ethylene oxide and hydrogen peroxide in high power magnification: Five cycles (EO5) (B), (HP5) (E) and more than five cycles (EO>5) (C), (HP>5) (F) (SEM images, x7500 magnification). Arrows indicate the deterioration in surface area. (A, D) No apparent changes in new samples (Control).
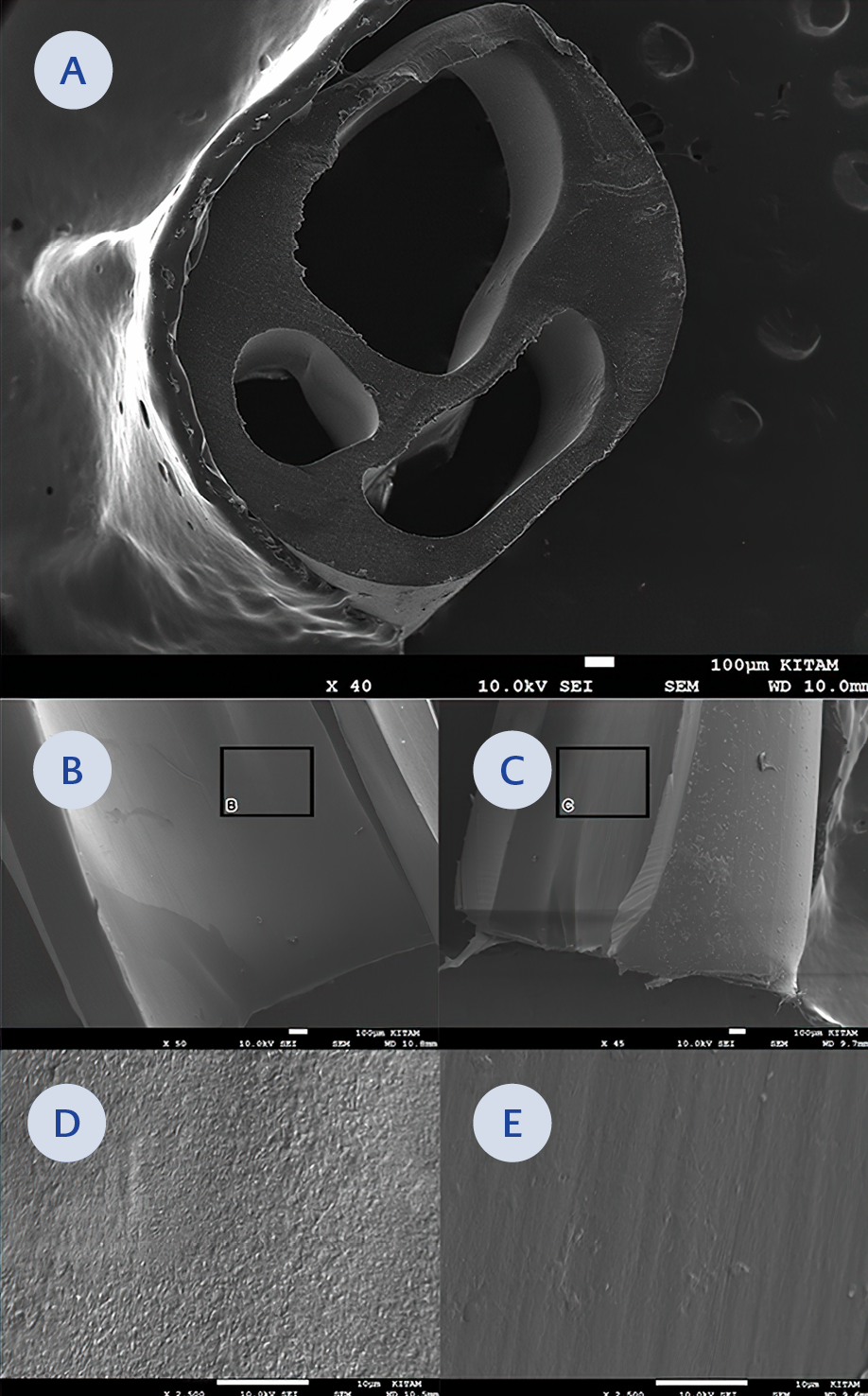
Figure 3. (A-E) Inner surface examination. (A) Transverse section of PTCA catheter (x40 magnification). (B, C) Inner surface observations in ethylene oxide and hydrogen peroxide groups (x50 magnification). (D) Inner surfaces on ethylene oxide (x2500 magnification). (E) Inner surfaces on hydrogen peroxide (x2500 magnification), which belong to the areas indicated by the black rectangle.
In EO sterilization, while no major damage was noted within five cycles, significant damage was observed at x2500 magnification as the number of processes increased (Figure 1B). Compared with EO, more vigorous and deeper lines and distortions were observed in HP sterilization as reprocessing cycles were increased (Figures 1A, 1B, 2B, 2C). In addition, severe scattered seed-like distortions were also noticed, especially in the HP group (Figure 2E, 2F). On the examination at x7500 magnification, the harmful effects of EO were significant on the surface of catheters reprocessed more than five times with EO compared to those reprocessed five times (Figure 2B, 2C). No significant damage was noted in the new disposable catheter (Figure 2A, 2D).
It was noted that relatively fewer cracks and crevices were revealed on the inner surface than on the outer surface (Figure 3A-3C). The mean value, standard deviation, and statistical differences between the groups are given in Table 1. The outer and inner deterioration scores were significantly higher in the EO>5 group than in the control group (p=0.037). Similarly, the outer and inner deterioration scores in the HP>5 group were significantly higher than in the control group (p=0.0097). However, the bacterial contamination score in the EO>5 group was higher than the control group (p=0.0032). In addition, there was no significant difference between the other groups regarding bacterial contamination and deterioration (p>0.05).
Discussion
Disposable instruments are reused mainly for economic reasons (10, 11). There is no definite limit to the cycles in which the tools can be used safely, and there is no estimated decrease in work capacity or increase in infection (2). Although reusing PTCA catheters with blood contact is prohibited in some developed countries, reprocessing is frequently applied. The main problem is severe destruction in the structure of the disposable device because of reprocessing.
Our study showed that HP and EO sterilizations cause marked distortions and may affect the inner and outer catheter surfaces. Besides, it is well known that repeated balloon inflation during interventional procedures causes deterioration in the structure (12). In addition to hygiene, mechanical failures of the devices and safety problems can be challenging (13-15). Our study revealed that the destruction was higher in HP gas plasma sterilization than EO for the same number of processes on the same type of PTCA catheters. In their study, Yoshida and Kobayashi evaluated the effects of HP sterilization, EO gas sterilization, and low-temperature steam formaldehyde sterilization on 11 different plastic panel surfaces by SEM. Unlike other sterilization methods, they detected structural changes on the plastic surfaces after HP sterilizations. They showed the destruction of plastic shells and the instrument structure even after one cycle of reprocessing (16, 17). Unverdorben et al. reported that mechanical properties deteriorated in PTCA catheters from two companies after repeated sterilization cycles with EO (18). We found that both sterilization methods caused deterioration on the surface of catheters as the number of reprocessing procedures increased, and this deterioration was particularly prominent in HP sterilization. As the cycles increased, the damage was observed even in less damaging EO sterilization. While some studies have indicated no morphological or chemical changes in catheters reworked with EO, combining chemical cleaning with mechanical vibration during pre-cleaning caused coarse anatomical and chemical surface degradation (19). However, in our study, the same pre-cleaning method using enzymatic solvents was applied for both sterilization types, and the destruction was found to be greater after HP sterilization.
The catheter might break during the procedure due to damage occurring when reused (20-22). Although catheter rupture is rare, as a severe complication, this might expose patients to complications arising from reuse. Balloon rupture during stent placement may cause arterial spasm, vascular dissection, sudden chest pain, angina pectoris, and shock (22-24). Therefore, angiographic and interventional catheters should not be reprocessed or reused thrice due to mechanical integrity and loss of function (25). Besides, reusing PTCA catheters might lead to several clinical problems; some authors argued that reusing after standardized reprocessing would be safe and effective (26). Although the effectiveness of sterilization was not a priority and not evaluated in our study, bacterial clusters were shown in the cracks on the catheter surfaces by electron microscopy despite being used once and reprocessed five times and more. In a study in which interventions with reused disposable PTCA catheters were evaluated, it was stated that the complications, including infection and the number of catheters used per procedure, were high (27). Shaw et al. reported that they did not find a significant difference in procedure duration, complication rate, or success rate in a study comparing patients who were operated on with reused catheters for a maximum of four times and patients with a single-use catheter (28).
Since the economic, legal, and ethical aspects of instruments labeled as disposable are not the same as those prepared for reuse, the issue of reuse is controversial (29). It is emphasized that the number of reprocessing is associated with internal surface damage and the life span of catheter material (26). Frank et al. investigated increased risk due to bacterial contamination or pyrogenic reactions in a study involving 414 patients undergoing cardiac catheterization or angiography using a reused catheter. They studied single-use, once or twice-sterilized, and up to 10-sterilized catheters. They found no significant differences in fever reaction and no development of infection-related complications in the groups (13). Another study stated that local infections or systemic pyrogenic responses were observed in 4.3% of patients with reused catheters; however, there was no significant difference between the groups using reusable catheters and treated with disposable catheters (29). Some biological wastes remain in the reused catheters; however, they do not interfere with the bloodstream since they are fixed to the catheter (26). Collignon et al. reported that since PTCA catheters are difficult to clean because of their narrow lumens, the risk of infection increases significantly in more than 20 uses of general instruments (30).
The reuse of PTCA catheters is an accepted practice in some European countries. In the chapter on the reprocessing of medical devices in the Robert Koch Institute guide in Germany, cardiac catheters are included in the high-level critical medical device category, and it is stated that the reuse of these devices is particular and requires an active external quality control system (3). Rutala et al. stated that reusing is inappropriate since critical disposable instruments are treated with liquid chemicals and non-sterile water during resterilization (9). In the USA, single-use is preferred due to legal barriers. Nowadays, single-use applications are drawing attention worldwide (2, 3, 26). Reuse is widely applied in disposable instruments in Palestinian hospitals. Habib and colleagues reported no growth when they microbiologically examined PTCA catheters resterilized with formaldehyde, while they isolated Staphylococcus aureus in catheters resterilized with glutaraldehyde. In the Indian guidelines created for the use of cardiovascular catheters and instruments, while it is stated that PTCA catheters can be used up to three times in case of strict follow-up of cleaning, disinfection, and resterilization processes, it is recommended that the procedures should be controlled by reporting the risk of infection and insufficiency in balloon expansion (31).
In conclusion, our findings showed that HP and EO sterilizations caused some deterioration in the inner and outer surfaces of PTCA catheter samples. The damage from sterilizing PTCA catheters for reuse may cause life-threatening mechanical complications. Therefore, when necessary, we recommend reprocessing using EO, the least damaging method, and paying attention not to exceed five cycles.