Introduction
Real-time reverse transcriptase polymerase chain reaction (RT-PCR) is widely used to diagnose SARS-CoV-2. However, PCR tests need expensive equipment and qualified personnel, which makes them only used in high throughput and advanced laboratory settings. Improvements in SARS-CoV-2 diagnosis with easy, rapid, and cost-effective approaches are required to control the pandemic of the coronavirus infectious disease 2019 (COVID-19) (1, 2). Rapid SARS-CoV-2 antigen tests require less technical expertise and laboratory capacity (3). Additionally, antigen tests result in 5 to 30 minutes, which is better than PCR. This study compared the mö-screen Corona Antigen Test (Qiagen, Germany) with RT-PCR in suspected COVID-19 patients.
Materials and Methods
We included consecutive patients admitted to Uludağ University Hospital Pandemic Outpatient Clinic with respiratory infection symptoms, including fever, cough, shortness of breath, sore throat, headache, myalgia, dizziness, loss of smell or taste, diarrhea, and runny nose which lasted less than a week. We simultaneously collected two combined FLOQSwabs® oro/nasopharyngeal swabs (Copan, Italy) samples, which were collected by healthcare workers. One of the swab samples was transferred to the laboratory in a viral nucleic acid transport (vNAT) medium used for RT-PCR, and the other was sent to the laboratory in a sterile tube used for antigen testing.
We used the mö-screen Corona Antigen Test, an immunochromatographic test for detecting SARS-CoV and SARS-CoV-2 according to the manufacturer’s instructions. According to the manufacturer, the test results were within 15 minutes, and all necessary reagents were provided in the kit (4). Although the antigen test results may be affected by many parameters such as the time of sample collection, sampling technique, quality of the sample, time of study, and according to the person evaluating the test result, we tried to validate the test results by sampling by health care workers, testing the samples in four hours, only one operator for the antigen tests in the same laboratory who is the only one to evaluate the antigen test result. We tried to quantify the samples according to the test band’s colour intensity in three (strong positive, moderately positive, and weak positive) groups.
We used the Biospeedy® SARS-CoV-2 RT-PCR test (Bioeksen R&D Technologies Inc., Turkey) kit for the detection of SARS-CoV-2. Bio-Speedy® SARS-CoV-2 (2019-nCoV) RT-qPCR Detection Kit is on the World Health Organization (WHO) “Emergency Use List”. Validated with vNat® Sample Prep Solutions (Bioeksen R&D Technologies Inc., Turkey) were used for extraction of viral RNA. The vNat® Technology provides rapid, simple, and reliable sample prep solutions for various samples and swabs. Without any manual or robotic extraction, samples were ready to use directly in PCR in a few minutes. Pathogen activation and nucleic acid release occur in a single container, thus assuring biological safety, saving time, and reducing consumables costs (5). This kit targets SARS-CoV-2 specific N, ORF 1a, ORF 1b genes. We performed PCR by using a Rotor-Gene (Qiagen, Germany) RT-PCR device according to the manufacturer’s instructions. Cycle threshold (Ct) lower than 35 were considered positive for SARS-CoV-2. The SARS-CoV-2 RT-PCR and Ag tests were performed in the Molecular Microbiology Laboratory.
The study was conducted in accordance with the tenets of the Declaration of Helsinki. Informed consent was obtained from patients. The Bursa Uludağ University School of Medicine Clinical Research Ethics Committee approved the protocol on 6 October, 2021 with approval number 2021-15/11.
We statistically analyzed sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy. We used Fisher’s exact chi-square test with or without Yates correction, Pearson chi-square exact test, Shapiro-Wilk test, Fisher-Freeman-Halton test, and Pearson correlation test in the Statistical Package for Social Sciences (SPSS) 23.0 (IBM Corp., Armonk, NY, USA).
Results
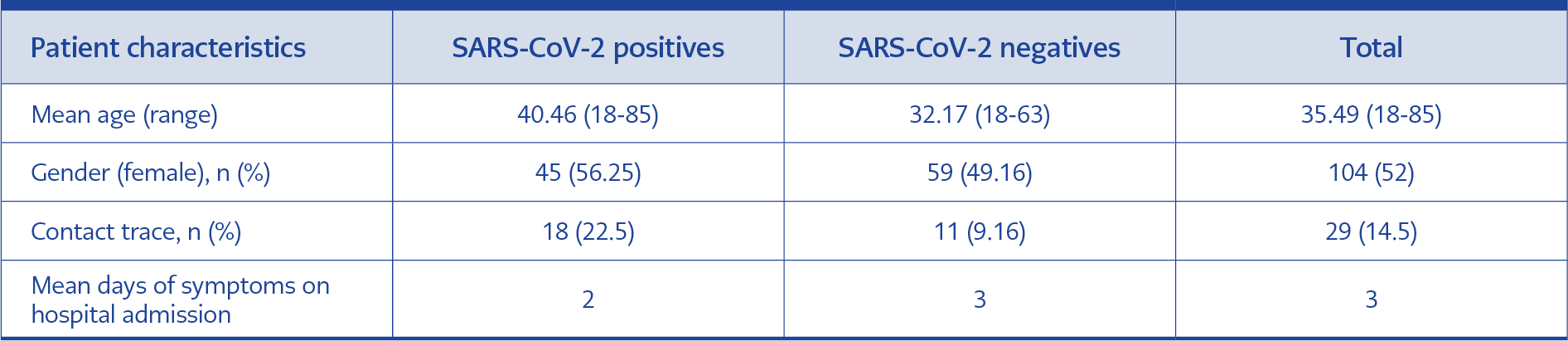
Table 1. Age and gender distribution of patients, number of contacts, and duration of symptoms at admission in days.
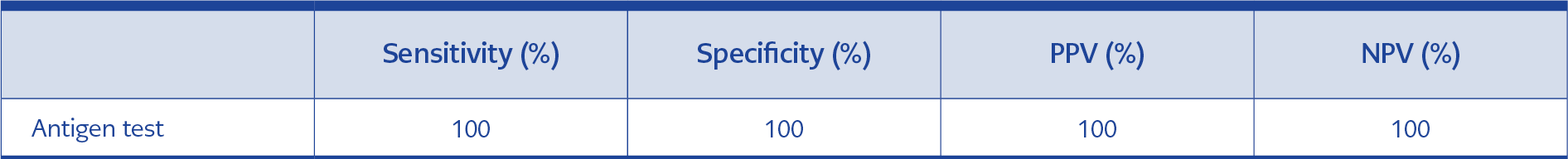
Table 2. Sensitivity, specificity, positive and negative predictive values of antigen test compared with RT-PCR.
We analyzed the performance of the mö-screen Corona Antigen Test (Qiagen, Germany), compared with the Biospeedy® SARS-CoV-2 RT-PCR test detection among symptomatic patients. The study group comprised 200 patients, including 104 (52%) women and 96 men (48%). The mean age was 35.49 years (Table 1). Among 200 samples, 80 were positive for the mö-screen Corona Antigen Test and SARS-CoV-2 RT-PCR test, and 120 were negative for both methods. The accuracy between the two methods was 100%. Antigen test’s sensitivity, specificity, PPV, and NPV were found to be 100% among PCR (Table 2).
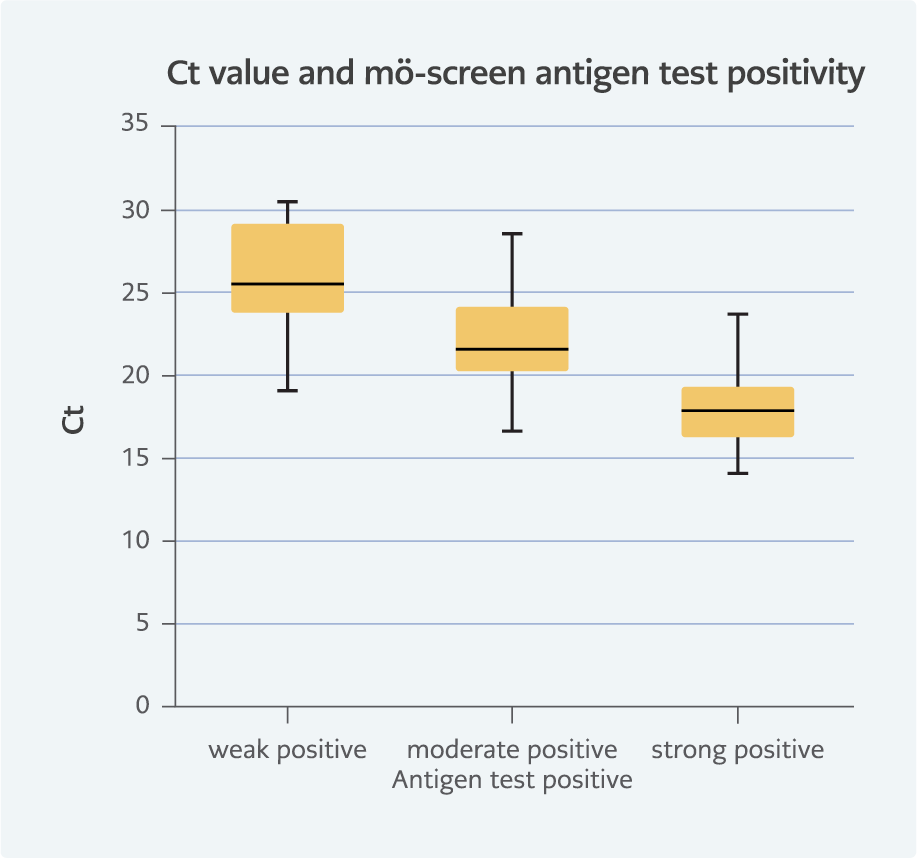
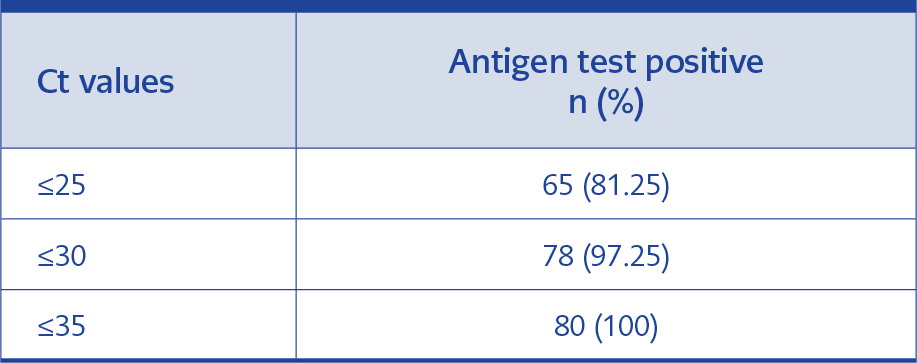
The median Ct value of 80 patients was 21.4, which ranged between 14.03 and 30.37. Although the manufacturer described the mö-screen Corona Antigen Test as a qualitative test, we quantified the samples according to the test band’s colour intensity. We divided the positive samples into three (strong positive, moderately positive, and weak positive) groups. Our semi-quantitative evaluation revealed 19 weak positive antigen tests with Ct values ranging between 18.9 and 30.37. Moderate and strong positive Ct values ranged between 16.56- 28.48 and 14.03- 23.66, respectively (Figure 1). Antigen test positivity and Ct values had a -0.706 correlation (p<0.001). While 65 (81.25%) positive samples had a Ct lower than 25, two samples had a Ct greater than 30 (Table 3). While 64 (80%) antigen tests resulted in positive in one minute, all of the positive tests resulted within five minutes. We compared the Ct values and the days of symptoms but could not find any correlation.
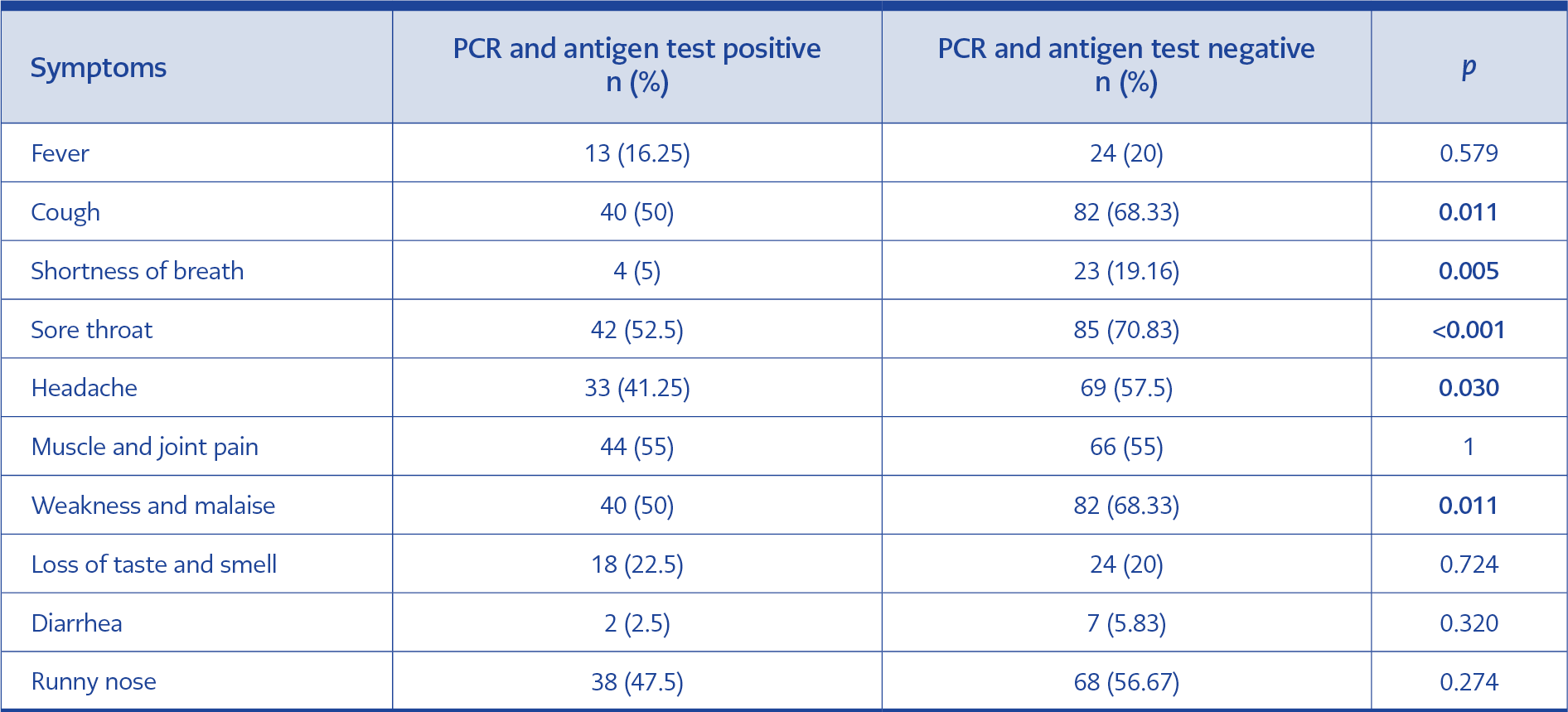
Patients’ symptoms (fever, cough, shortness of breath, sore throat, headache, muscle and joint pain, weakness and malaise, loss of taste and smell, diarrhea, and runny nose) were compared according to the positivity of the tests (Table 4). All symptoms were found to be numerically less in the group with positive tests compared to those with negative tests. The most common symptoms were cough, sore throat, malaise, and muscle and joint pain in both groups. The loss of taste and smell was slightly higher (22.5%) in the positive group. Diarrhea was the least common symptom in both groups. No significant correlation was found between symptoms such as fever, muscle and joint pain, loss of taste and smell, diarrhea, and runny nose in the two groups (p>0.05). It was determined that cough, shortness of breath, sore throat, headache, fatigue, and malaise symptoms were significantly higher in those with negative tests compared to those with positive tests (p<0.05).
Discussion
Rapid antigen tests are increasingly used as point-of-care testing options in COVID-19 diagnosis. There is a significant gap in performance data for symptomatic adults and asymptomatic adults and children due to the need to know how to perform rapid antigen testing optimally and the inability to perform all these tests equally in comparative studies (6). The WHO recommends using rapid antigen tests in adults with the onset of symptoms in less than seven days, and if the result is negative, the results can be confirmed by RT-PCR or repeated tests. In addition, during epidemics, it is recommended to monitor the trend in disease incidence, isolation, and screening for early detection of the disease by rapid antigen tests (7). Rapid diagnostic tests can be incorporated into efficient testing algorithms as an alternative to PCR to decrease diagnostic delays and onward viral transmission (8). The main limitation of the rapid tests is the possibility of false negative results in samples with low viral load. Hence, it might not often be suitable for detecting COVID-19 in less symptomatic and asymptomatic patients (9).
According to the WHO and the Centers for Disease Control and Prevention (CDC) recommendations, the PPV of a positive antigen test result is high at ≥5% prevalence, so negative results should be confirmed with NAT. In comparison, at a prevalence ≤5%, positive antigen test results should be confirmed with NAT. Antigen-detecting rapid diagnostic tests (Ag-RDTs) perform best in individuals with high viral load early in the course of infection and are most reliable in settings where SARS-CoV-2 prevalence is ≥5%. When there is no transmission or low transmission, the PPV of Ag-RDTs is low, and in such settings, nucleic acid amplification techniques (NAATs) are preferable for first-line testing or confirmation of Ag-RDT positive results. The WHO recommends using Ag-RDTs that meet minimum performance requirements of ≥80% sensitivity and ≥97% specificity. Ag-RDTs are less sensitive than NAAT, particularly in asymptomatic populations, but careful selection of cohorts for testing can mitigate this limitation (10, 11).
We used two combined oro/nasopharyngeal swab samples, one for antigen test and the other for PCR test. Although the manufacturer recommended nasopharyngeal sampling, we used combined swab samples to increase the test’s sensitivity. We found the sensitivity of the mö-screen Corona Antigen Test to be 100%, which is higher than the sensitivity (98.32%) of nasopharyngeal swab specimens in the kit insert. The sensitivity of the mö-screen Corona Antigen Test was 100% for samples with a Ct value lower than 25 but 47.8% for samples including Ct values between 25 and 30 (12). Although different sampling methods have been used for SARS-CoV-2 testing, nasal swabs, gargle, and mouthwash samples show less sensitivity among nasopharyngeal samples. We argue that using combined oro/nasopharyngeal samples increases the sensitivity of COVID-19 tests (13, 14).
Positivity in the mö-screen Corona Antigen Test was observed within the first five minutes. Although it is stated in the test insert that 15 minutes are required for the test to be evaluated, in our study, we found that only five minutes were required for the test result. Only five minutes of the test is a study-specific result, but the manufacturer can re-evaluate it with more data.
The Ct value, inversely proportional to the logarithm of viral load, can be used to infer viral load (15). Although the Biospeedy®SARS-CoV-2 RT-PCR kit is for qualitative evaluation, we tried to quantify the samples by Ct values. We categorized antigen test results into three groups according to band intensity. Since the CDC considers all samples with a Ct value below 33 to be contagious, all of our study’s positivity samples are considered contagious. The test sensitivity increases in high viral load samples (16-18). Viral quantity is in correlation with the colour intensity of the antigen test judgment line; it should be taken into account that a lower viral load in the specimen shows a lower positivity rate by visual judgment; thus, the visual judgment results may be different according to the visualizer (19). We observed heterogeneity in the distribution of Ct values in the groups. In addition, we found an inverse correlation (correlation coefficient -0.706, p <0.001) between the Ct value and the groups that we divided into weak, moderate, and strong positive results in the rapid antigen test. Reporting Ct values in qualitative RT-PCR tests is not a standardized quantification method and may lead to misinterpretation of the results.
Although the statistical comparison of subjective data in two qualitative methods gives an idea about the study’s results, it is not easy to adapt it to routine practical application. Saglik et al. compared median Ct values in samples obtained within the first five days of symptoms onset, which were lower in patients with severe disease when compared to mild and moderate, but the difference was not statistically significant (20). Pollock et al. found an inverse correlation between Ct values and antigen test positivity, concordant with our study (6). These two studies have conflicting results, so further investigation is needed to standardize PCR and antigen tests for quantitative results. Phillips et al. showed significantly lower Ct values (representing higher levels of viral RNA), suggesting that increased transmission of COVID-19 was temporarily associated with higher viral loads. Decreasing Ct values appear to be a leading indicator for predicting future COVID-19 cases, which can facilitate improved hospital-level surge planning (21).
In evaluating the results of the Abbott BinaxNOW rapid antigen test, three Ct values [25, 30, 35], considered threshold values, were used, and sensitivity was evaluated at three different Ct cutoffs, [25, 30, and 35]. Sensitivity in all subgroups combined was 99.3% with Ct values of 25, 95.8% with Ct values of 30, and 81.2% with Ct values of 35. Band strength (1 [n=41]; 2 [n=15]; and 3 [n=170]) as interpreted by the primary visualizer for the 226 positive BinaxNOW tests correlated with Ct value (6). Tamura et al. investigated symptomatic COVID-19 patients to study the diagnostic accuracy of a novel SARS-CoV-2 rapid antigen test. They showed the sensitivity of the antigen test 100% for the first six days of the disease using specimens with moderate or high viral load (Ct values <30). However, from day 7, the sensitivity was 70.4-90.6% and 83.9-84.6% for the anterior nasal and nasopharyngeal sites, respectively (19). Krüttgen et al., using 75 swabs from positive patients by SARS-CoV-2 PCR and 75 swabs from negative patients by SARS-CoV-2 PCR, investigated the sensitivity and specificity of the SARS-CoV-2 rapid antigen test (Roche, Switzerland) and found the assay’s sensitivity with samples with a cycle threshold of <25 as 100%, 25-30 as 95% and 30-35 was 44.8 % (22). In another study comparing fluorescent-based immunochromatographic rapid antigen test and RT-PCR with nasopharyngeal swab samples taken from 251 patients in Wuhan and Chongqing, China, the sensitivity of the rapid antigen test was 75.6% and the specificity 100%, with Ct value 40 as the cutoff (23). Krüger et al. compared rapid antigen test (SureStatus; PMC Private Limited) and RT-PCR test results in Germany and India; the sensitivity was 82.4%, and the specificity was 98.5% (24). Yıldız et al. compared rapid antigen tests and PCR and found the sensitivity and specificity as 80.6% and 93.7%, respectively (25). The quality of the antigen test, presence of respiratory infection symptoms, validation of sampling, transport, processing of antigen and PCR tests, and the prevalence of SARS-CoV-2 and other respiratory viral infections may affect the sensitivity and specificity of the tests (6, 18, 21-27).
For patient comfort, saliva or nasal swab samples could be more suitable than combined nasopharyngeal-oropharyngeal swab samples. Lee et al. compared sampling methods, saliva, oropharyngeal, nasal, and nasopharyngeal, and found that nasopharyngeal or combined oro/nasopharyngeal swab samples showed higher sensitivity than other sampling methods (28). Additionally, samples provided by a healthcare professional can increase the sensitivity of the tests (29). The sensitivity of the tests is highly dependent on the sampling technique, the type of sample collected, and the experience of the sampling personnel.
During the pandemic and our study, respiratory viruses other than SARS CoV-2 also caused respiratory tract infections (26). Notably, the symptoms of shortness of breath, cough, headache, sore throat, weakness, and malaise were statistically significantly higher in other respiratory tract infections with a negative COVID-19 test. There was no significant difference between the group with positive and negative tests regarding fever, muscle and joint pain, diarrhea, and runny nose symptoms. Loss of taste and smell symptoms were seen proportionally more frequently in the group with positive tests, but the difference was not statistically significant. In this study, we could not show a specific symptom of COVID-19. Although respiratory tract infection symptoms are similar, tests to determine the causative agent should be performed for differential diagnosis (27).
The sensitivity of our results was higher than many studies, which may be because we used combined oro/nasopharyngeal swabs, which a healthcare professional obtained, the same person evaluated antigen tests, samples’ Ct values were lower than 31, and we included only symptomatic adult patients (28-31).
Our study has some limitations. Ct values and viral load may depend on the quality of the sample, that is, the method of collection and the swab used. We included 200 patients in the study, and all samples were collected from one health center. To standardize visual judgment bias, only one professional evaluated antigen tests. The sensitivity of the antigen test was calculated for each day of illness; however, the number of samples in each group was small, which is why the statistical analysis is not robust.
Our study demonstrated the diagnostic accuracy of the mö-screen Corona Antigen Test for the accurate diagnosis of COVID-19 in terms of both sensitivity and specificity. We found the sensitivity and specificity of the mö-screen corona antigen test to be 100%. Sampling time, sampling method, and sampler can change the sensitivity and specificity of the test. The best testing accuracy is achievable when the sampler is a healthcare professional and acquires a combined oro/nasopharyngeal sample in adult patients’ first seven days of symptoms (32). The accuracy achievable by the mö-screen Corona Antigen Test, combined with the rapid turnaround time compared to RT-PCR, suggests that these tests could significantly impact the pandemic if applied in thoughtful testing and screening strategies.