Introduction
Over the last two decades, the rates of carbapenem-resistant (CR) pathogens have increased dramatically in Greek hospitals, with Klebsiella pneumoniae as the most worrisome representative (1). According to the recent European Annual Surveillance Report from the European Centre for Disease Prevention and Control (ECDC), Greece ranks first in Europe, with the highest percentage of CR isolates among invasive K. pneumoniae, although a decreasing trend is being observed from 68.2% in 2011 to 61.9% in 2015 (2).
Carbapenems have been the recommended therapy for extended-spectrum beta-lactam (ESBL)-producing Enterobacteriaceae and other multidrug-resistant (MDR) pathogens; however, their over-prescription was the driving force for the endemicity of carbapenem resistance of Gram-negative pathogens in Greece (2-4). Antimicrobial stewardship programs (ASPs) are interventions to improve and assess the proper use of antimicrobial agents, which requires the selection of the best antimicrobial drug regimen, i.e. doses, therapy duration, and administration routes (5-7). These programs are a useful tool, targeting to improve antibiotic use, spare the carbapenem class of antimicrobials and maybe diminish antibiotic resistance rates of key nosocomial pathogens (4, 5, 8). Decrease in carbapenem prescription when non-necessary, has become one of the pivotal ASP targets, particularly in areas with carbapenem-resistance endemicity, although optimal treatment of ESBL and CR infections with non-carbapenem containing regimens remains a matter of ongoing debate (4, 8, 9-11). Our purpose was to implement an ASP-based on judicious sparing of carbapenem prescriptions, in a Greek tertiary care hospital and investigate firstly its feasibility in a setting with longstanding “trust” in carbapenem-based regimens and secondly its safety for the patients.
Materials and Methods
Setting
The study was conducted at Thriasio General Hospital of Elefsina, a 450-bed tertiary care hospital serving the north-west part of Attika, Greece. The hospital comprises two Internal Medicine Departments, each served by a separate group of physicians, a General Surgery, a Neurosurgery, an Orthopaedic Surgery, a Neurology, a Pulmonology, and a Urology Departments as well as two General Intensive Care (ICU), one Cardiac ICU, one Burn and one Dialysis unit. Infectious Disease (ID) consultation for the entire hospital was provided by an ID specialist, upon request from the treating physician. Before the initiation of this study, there was no formal ASP implemented in the hospital.
Study design
This study is a quasi-experimental before-and-after study. We compared a 12-month pre-intervention period (October 2012 to September 2013) with a 27-month intervention period (October 2013 to December 2015), to investigate the feasibility of the program and its impact on clinical outcomes. Patients included in the study were adults (≥18 years of age) for whom the treating physician prescribed a type II carbapenem (imipenem or meropenem). Patients were excluded from the study if they were neutropenic (defined as a polymorphonuclear count ≤0.5×109 cells/l) for any cause, pregnant, transferred from an outside hospital already receiving a carbapenem, or if they died within 48 hours of the prescription request for the carbapenem. Patients who received more than one course of carbapenems within this period were only included once in the study. During the pre-intervention period (October 2012 to September 2013), an internist reviewed the clinical records of all eligible patients (retrospectively for the first six months and prospectively after that) and abstracted demographic, clinical and outcome data using a standardised case report form. Outcome evaluation and follow-up were done as described below.
Intervention
The During the intervention period (October 2013 to December 2015) an ASP of prospective audit and feedback was implemented throughout the hospital (except for the Burn unit and one of the two general ICUs because physicians in these units were unwilling to participate in the study). The ASP team, comprised of an ID specialist, two internists educated in Infectious Diseases and two Infection Control (IC) nurses, provided unsolicited face-to-face consultation for patients for whom the treating physician had prescribed a type II carbapenem (meropenem or imipenem). The team was alerted by the pharmacy upon prescription request for carbapenem and responded within 48 hours. After reviewing the medical records and examining the patient, the ASP team discussed with the treating physician alternative, carbapenem-sparing options for empiric coverage or de-escalation to narrow-spectrum effective antimicrobials, if relevant microbiological data were already available. Empiric carbapenem-sparing regimens were proposed based on clinical and epidemiological data including site and severity of infection, comorbidities, history of previous antimicrobial exposure over the past three months, history of previous hospitalisation over the past three months and any available microbiological data including previous clinical or surveillance cultures. As a rule, the ASP team avoided the empiric use of antimicrobial classes that the patient had received during the past three months (12, 13). The ASP team also reviewed the dosing regimen and the duration of treatment. During the intervention period, a focused educational program was also launched aiming to highlight the importance of judicious use of carbapenems, to familiarise prescribing physicians with alternative antimicrobials and to introduce algorithms for choosing among these antimicrobials based on the clinical characteristics of the patient and its risk factors for multidrug-resistant pathogens.
All patients included in the study were divided into two Groups: Group A consisted of those for whom the treating physician agreed with the proposing regimen and replaced the carbapenem, whereas Group B consisted of those for whom the physician disagreed and continued the carbapenem. Both Groups were evaluated for primary outcome death at 28 days. Those discharged were followed through the electronic medical records for readmission to the hospital within 30 days for any reason. Demographic, clinical and outcome data for all included patients were abstracted from the medical records and prospectively recorded. The severity of illness was evaluated with the Acute Physiology and Chronic Health Evaluation (APACHE II) score (14) calculated at infection onset.
The study was approved by the Ethics Committee of Thriasio General Hospital and was conducted under a waiver of consent as the ASP was considered a standard of care practice in the hospital and complied to international guidelines for control of antimicrobial resistance (6).
Microbiological methods
Isolate identification and MIC determination were performed using the BD Phoenix automated identification and susceptibility testing system (Becton, Dickinson and Company, NJ, USA) whereas for colistin and tigecycline E-test was used (BioMérieux, Marcy l’Etoile France). All MICs were interpreted according to CLSI recommendations and breakpoints, whereas for some antibiotics such as tigecycline and colistin using the EUCAST contemporary recommendations (15, 16).
Definitions
The criteria of Horan et al. (17) were used for the diagnosis of specific types of infections. Sepsis of undefined origin was used to describe patients who presented with sepsis while no specific infectious source was identifiable at the time of prescribing. Infections were classified as community-acquired non-healthcare-associated, community-acquired healthcare-associated or hospital-acquired based on previously defined criteria (17). Definitive antibiotic therapy included the final active antibiotic regimen after the return of susceptibility results. Patients were considered immunocompromised if they had received a transplant, had a splenectomy, a gamma globulin deficiency, HIV infection, were currently under cytotoxic chemotherapy, received at least 20 mg of prednisone/day for ≥30 days or received an immunosuppressant agent for systemic illness. Resolution of symptoms and signs of infection and improvement of relevant laboratory parameters was defined as a successful clinical outcome. Patients with an inadequate response and whose treatment regimen for this infectious episode was changed were characterised as having an unsuccessful clinical outcome (failure).
Statistical analysis
The Shapiro-Wilk test was performed to test for normal distribution of continuous variables. The results of normally distributed variables are given as mean (SD) and for non-normally distributed variables are given as median (IQR). All qualitative variables are presented as absolute and relative frequencies. The Student’s t-test was used to compare normally distributed variables between the groups under study while for non-normally distributed variables Wilcoxon rank – sum test applied. The Fisher’s exact test was employed for comparison of categorical variables. Boxplots were used to represent data. All tests were two-tailed and statistical significance was established at 5% (p<0.05). Factors associated with mortality were assessed by univariable analysis and then cox regression analysis. Data were analysed using Stata™ (Version 13.0 MP, Stata Corporation, College Station, TX 77845, USA).
Results
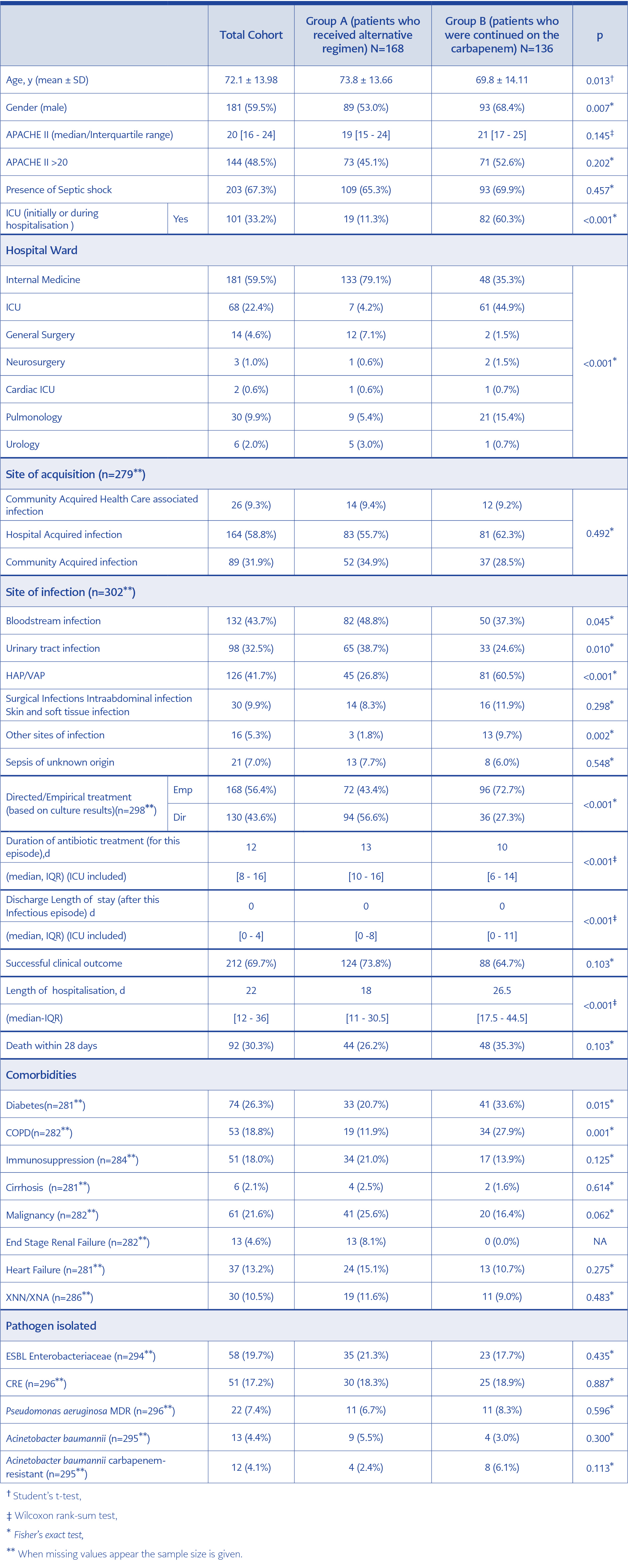
Table 1. Demographic and clinical characteristics and outcome for the 304 patients included in the study.
Strategy acceptance and patient demographics
A total of 304 patients were included in the study, 168 in Group A (received a carbapenem-sparing regimen) and 136 in Group B (received a carbapenem-based regimen). Prescribers-treating physicians’ adherence to the recommendations of the ASP team was 71.8%. Bedside consultation workload of the ASP team doubled during the intervention period, from 15 hours per week to 30 hours per week, divided among its five members according to their spectrum of permitted interventions. Time spent in the microbiology laboratory or pharmacy was not included in this estimation; a lesser increase for these activities was observed, compared to the pre-intervention period.
Table 1 presents demographic and clinical characteristics and outcomes for the total cohort and each one of the two groups. Statistically significant differences occurred between groups for age, gender and hospital ward between the two groups. Only 7 (4.2%) patients in group A were treated in ICU in contrast to 61 (44.9%) patients in group B (p<0.001). In group A, most patients were admitted to an internal medicine ward 133 (79.1%). Regarding comorbidities, patients in group B had significantly higher rates for diabetes (33.6%) and COPD (27.9%) in comparison to patients in group A (20.7% and 11.9%, respectively) (p=0.015 and p=0.001, respectively). There was no significant difference between the two groups with regards to site of acquisition of the infection. Most infections were hospital-acquired in both groups. No statistically significant difference was observed for APACHE II score or septic shock between the two groups. Most patients were severely ill (median APACHE II, 19) whereas 68% were in septic shock. Bloodstream and urinary tract infections were more frequent in group A (48.8% and 38.7%, respectively) than in group B (37.3% and 24.6%, respectively) (p=0.045 and p=0.01 respectively). HAP/VAP was more common in group B (60.5%) than in group A (26.8%) (p<0.001). ESBL-producing Enterobacteriaceae ranked first in both Groups, followed by CRE, P. aeruginosa and A. baumannii (Table 1). No statistically significant differences were observed for the rates of pathogens isolated between the two groups.
Antibiotic regimens
The most frequently adopted non-carbapenem regimens among 168 Group A patients were as follows: Piperacillin/tazobactam (P/T) plus aminoglycoside in 38 patients (22.61%), P/T plus an anti-Gram-positive agent (vancomycin, daptomycin, cotrimoxazole or teicoplanin) 21 patients (12.5%), P/T monotherapy 8 patients (4.8%). Colistin combinations with tigecycline ±an aminoglycoside was administered in 23 patients (13.7%), colistin with a beta-lactam in 14 patients (8.3%), colistin with an aminoglycoside in 8 patients (4.8%), colistin plus an anti-Gram-positive agent in 7 patients (4.2%), tigecycline with an aminoglycoside in 6 patients (3.6%). Various other combinations were administered in 28 patients (16.7%) with only two patients administered antifungal combination with beta-lactams and two more patients fosfomycin with beta-lactam.
Among 136 Group B meropenem was the only carbapenem used, given as monotherapy in 25 patients (18.4%), in combination with colistin in 36 patients (26.5%), with an anti-Gram-positive agent (either vancomycin, or teicoplanin or linezolid) in 26 patients (19.1%), with colistin plus anti-Gram-positive agent in 12 patients (8.8%), with an aminoglycoside in 6 patients (4.4%), with tigecycline in 5 patients (3.7%), with colistin plus tigecycline in 4 patients (2.9%), with an aminoglycoside plus an anti-Gram-positive agent in 4 patients, with an antifungal plus an anti-Gram-positive agent in 4 patients, with an antifungal in 4 patients ; finally 10 patients (7.4%) received other combinations with meropenem.
Outcomes
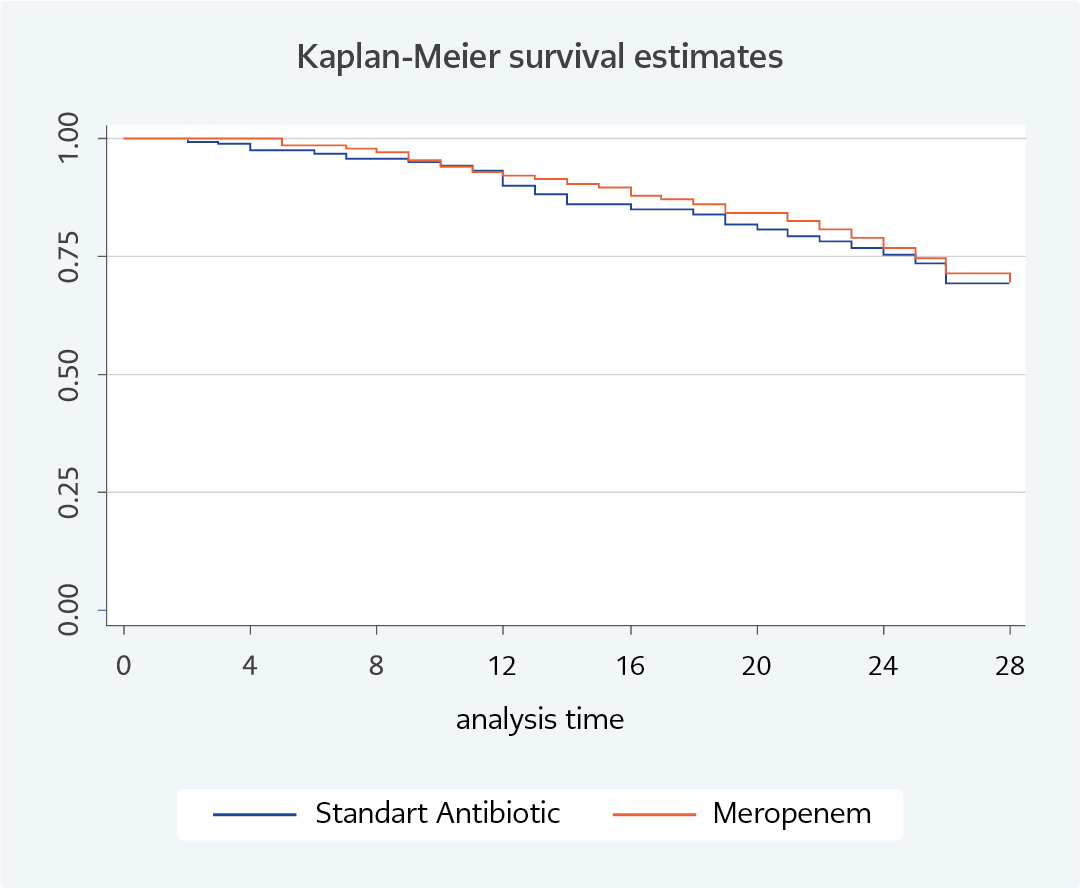
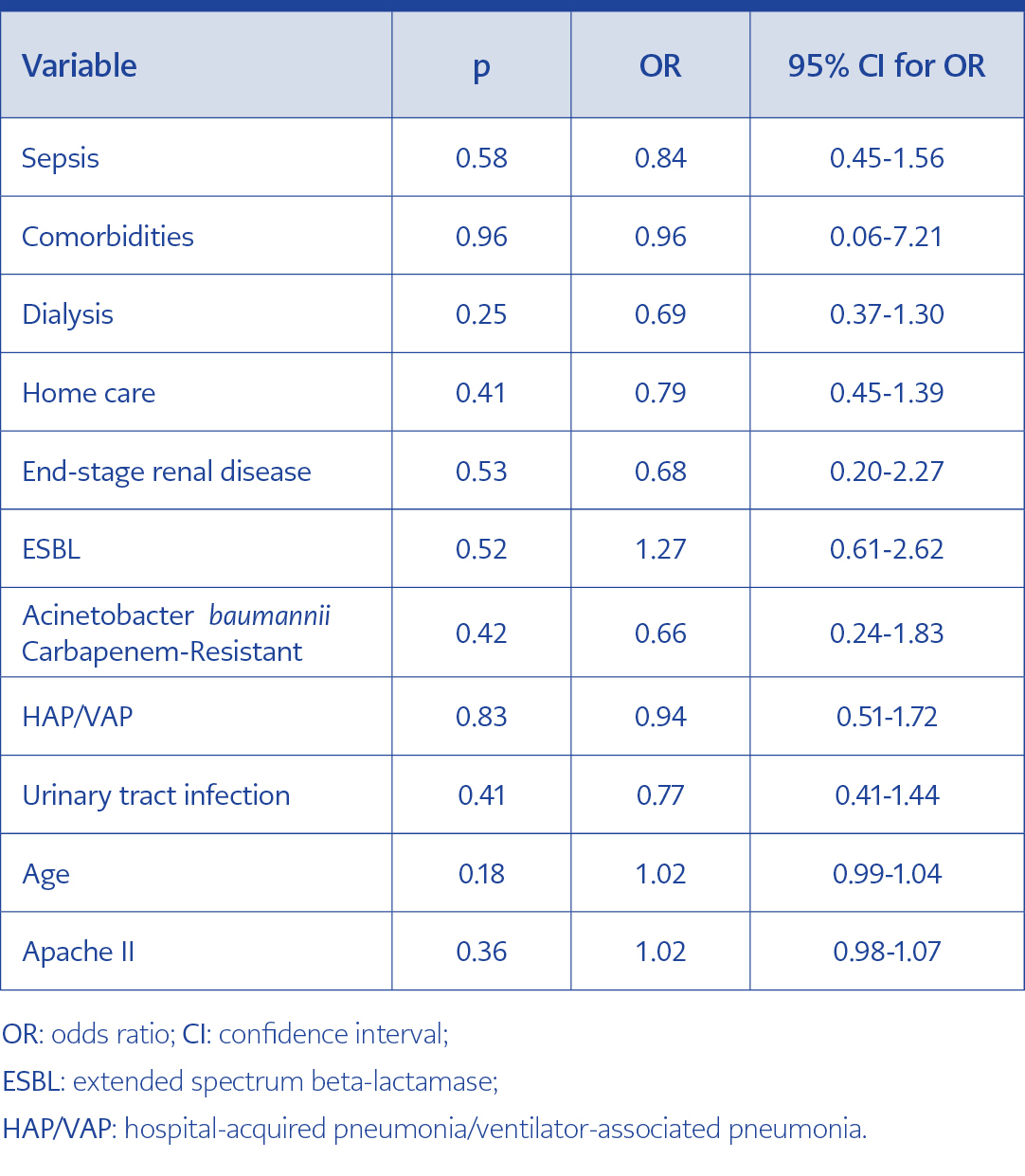
All-cause mortality for this cohort of severely ill patients was 30%. There was no significant difference in all-cause mortality within 28 days between the two treatment groups (26.2% versus 35.3% in group A and B respectively) (Table 1, Figure 1), whereas age>65years and APACHE II score >12 were associated with significantly increased mortality (p 0.03 and <0.001 respectively). Survival analysis was assessed by Cox regression (Table 3). No significant variable from the univariate mortality analysis was independently associated with mortality in Cox regression for mortality.
There was no difference between the groups with regards to the successful clinical outcome (Table 1). Patients treated with a non-carbapenem regimen (group A) had significantly longer antibiotic treatment as compared with those who received a carbapenem (group B) (mean duration, 13.3 vs 10.8 days, respectively, p<0.001), whereas group B experienced a significantly longer hospitalisation (median 18 vs 26.5 days in group A and B respectively, p<0.001), (Table 1).
Discussion
This is a pragmatic (real-world) prospectively recorded intervention of an ASP aiming to answer the question whether judicious sparing of carbapenems as empiric or definitive therapy is feasible and safe, in a high-resistance setting, in view of a possible impact on carbapenem resistance containment. Safety of the strategy was demonstrated, with no difference in crude mortality observed between the two comparator study groups. The studied cohort consisted of severely ill patients with a mean APACHE II of 19, with similar severity characteristics among the study Groups A and B. Treatment allocation of patients in the two Groups produced comparable 28-day mortality; however, survival analysis by Kaplan-Meier curves showed significantly lower survival rates with APACHE II score >12 and age >65years, thus verifying underlying disease severity and increased age as important contributors of mortality (p 0.03 and <0.001 respectively). This was not proven for survival analysis per treatment group.
A second important message from this study is its high acceptance among prescribers. The average compliance of physicians to spare carbapenems as part of the ASP-implemented strategy was 71.8%, underlining the significant workload of the ASP team members who were assigned to this task. It is worth mentioning that the time allocated to the “field work” as patient’s bedside consultation doubled compared to the pre-intervention period, from 15 hours per week to 30 hours per week. This workload was divided into the five members of the ASP team (one ID physician, two internists with ID training and two IC nurses) according to their spectrum of permitted activities. Dedicated time for unsolicited consultation, probably was the major driver of the acceptance of the strategy, since median change in antibiotic prescribing was only 42.3% for the effective interventions described in the literature (18, 19). This commitment of the ASP team is vital to ensure trust between “strategic stakeholders” and prescribers (20, 21), particularly in settings with established antimicrobial resistance conferring additional concerns about its impact on patient’s outcomes (8). In a new ASP carbapenem-restriction strategy from a single centre in Spain, 81.5% acceptance of the strategy was demonstrated (22). However, the strategy was applied only in the 38.7% of carbapenem prescriptions which the committee considered as non-justified. In our cohort, the strategy was applied in every carbapenem prescription whenever an alternative antibiotic was deemed adequate and safe optionby the ASP team, denoting a greater difficulty in changing prescribing behaviours. Given the fear of increased mortality whenever MDR isolates are encountered, empirical treatment, covering prevalent MDR pathogens should be initiated in severely ill patients accounting for individual or local risk factors. After the initial empiric treatment, de-escalation therapy should be performed if feasible from the microbiological and pharmacokinetic viewpoint (8, 23). Although physicians usually agree, in principle, with national guidelines, the absence of accompanying strategies for local implementation often presents a significant barrier. Therefore, interventions applied in medium-sized hospital and by persons with good communication skills among infection control practitioners had better odds for success (20, 21).
Infectious Diseases Society of America (IDSA) has placed the evaluation of the effectiveness of ASP strategies in specialised populations as a research priority (6, 7). Reports about outcome safety of carbapenem-sparing ASP programs in adult populations are scarce; three recent studies are all reporting no concerns about increased mortality or even increased rates of survival with the implemented strategy (20-22). It is noteworthy that all of these strategies were applied in settings with lower rates of antimicrobial resistance compared to our hospital and targeted at decreasing only non-justified carbapenem prescriptions.
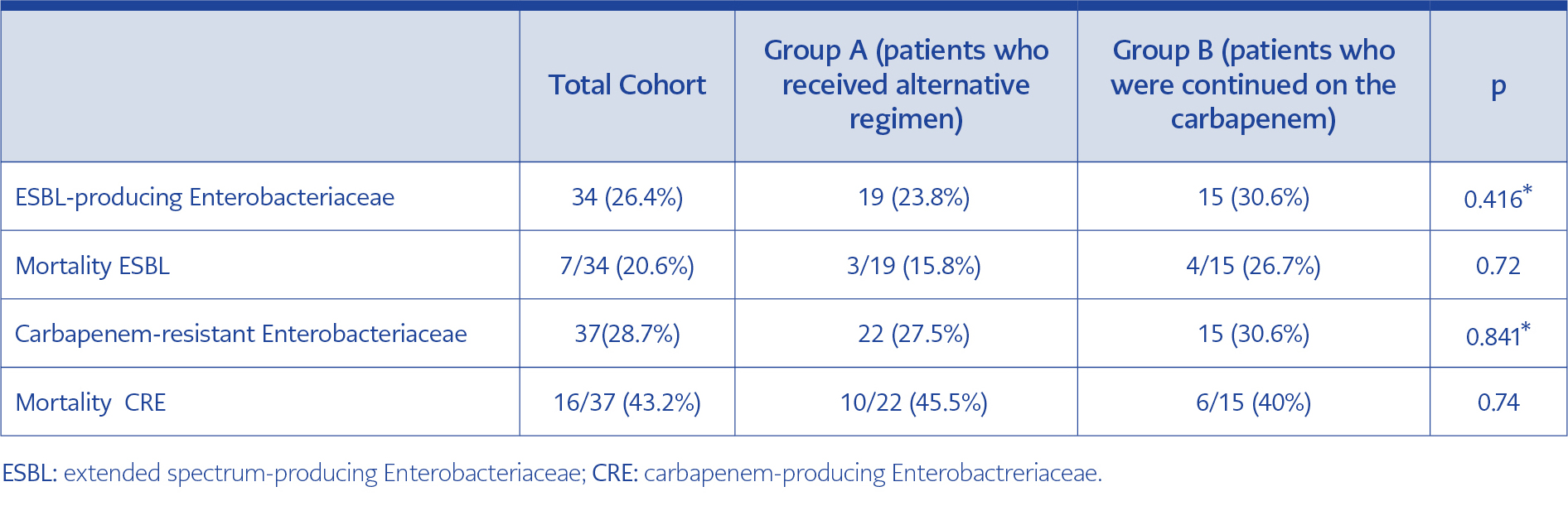
Table 2. Bacteremic infections by extended spectrum-producing and carbapenem-resistant Enterobacteriaceae: Distribution per treatment group and main outcome.
No significant differences in mortality between carbapenem-sparing and carbapenem-containing regimen found in our study should also be seen in the light of recent conflicting publications regarding the optimal treatment of ESBL infections (10, 11). In a subset of the studied population presented in Table 2, the mortality of bacteremic infections by ESBL was not different (and arithmetically lower) with a non-carbapenem regimen, compared to the carbapenem-containing regimen. Results of the INCREMENT study are in line with our observations, although derived from a retrospective approach (11), demonstrating the safety of non-carbapenem regimens in patients with no increased mortality risk. Similar results have been reported from two recent meta-analyses of observational studies, showing that beta-lactam/beta-lactam-inhibitor combination (BL/BLI) regimens may represent a safe alternative to carbapenems for infections by ESBL-producers (9, 24). However, results from a recently published randomised clinical trial (the MERINO study), including only bacteremic infections caused by ESBL-producing pathogens, showed increased mortality when a BL/BLI combination was used, as compared to carbapenem-containing regimens and the study was prematurely terminated (10). The results presented herein are real-life data and preclude in many cases a selection of patients by the physicians. We can easily suggest that treating physicians refused to use alternatives to carbapenems in patients with a bacteremic profile indicating a high mortality risk, similar to that measured by the INCREMENT score (11, 25). Maintenance of these high-risk patients as group B (receipt of carbapenem) by the treating physicians, may also explain the prolonged hospitalisation of this group, which had also more comorbidities compared to group A, despite similar APACHE II score at the onset of infection. Clinical judgment stands out as an important factor with two-way reading: in non-randomised trials, it may jeopardise the effect of the studied attribute, but in real life it may contribute to the favourable outcomes of patients deemed at increased risk. We believe that the unsolicited and bedside consultation of the ASP team contributed to mortality compared to the national median and relevant literature, despite the underlying severity of this cohort of patients, as indicated by their high APACHE II score (median 20).
Despite similar mortality, Groups A and B had different length of stay and duration of antibiotics. Prolonged length of stay in Group B may be explained by the significantly more frequent comorbidities and the higher percentage of ICU patients compared to Group A. Duration of antibiotics in group A was significantly lengthier and this cannot be fully explained by disease- or infectious episode-severity, since the ASP team was supervising both antibiotic selection and duration. However, if the non-carbapenem approach is seen as a “de-escalation” strategy, this trend for more prolonged treatment in the de-escalation group has been already reported. A “less-harmful perception” or a “less-effective perception” for de-escalating regimens by the prescribers may explain their tendency to retain antibiotic regimen for more days (26, 27).
The realistic approach of this study, is also underlined by the outcomes of patients with CR infections; their crude mortality is very close to that reported by the National Registry “Prokroustis” for carbapenem-resistant infections in Greek hospitals, indicating that data from this tertiary Hospital reflect national average of 42% (unpublished data) and do not deviate from international published experience summarised recently (28). Interestingly, for this subgroup of patients with CRE infections and particularly those with bacteraemias, as shown in Table 2, Group A had arithmetically higher mortality compared to Group B, although non-statistically significant. Several early observational studies from countries with endemicity of KPC-producers have reported on this issue (23, 28-30), lower mortality with carbapenem-containing combinations indicating an in vivo efficacy of carbapenems despite the production of carbapenemase, provided that the MIC of the isolates against meropenem is less or equal to 16mg/L (29, 30). High dose carbapenem is recommended in isolates with MICs up to 32 mg/L if drug monitoring can be performed (23). Our sample size might be small to verify these observations; however clinicians’ perception about the beneficial effect of carbapenems in the treatment of CRE with low carbapenem MICs was a difficult-to-defeat argument with prescribers of carbapenems. Real-time report (along with the rest of the antibiogram) of carbapenem MICs with E-test is crucial when antibiotic stewardship programs targeting carbapenem restriction are in place (23). We have not studied the MICs of carbapenems of the isolated pathogens, to see if a residual activity of carbapenems could account for this beneficial although the non-significant effect on mortality, however, cumulative microbiological reports of our hospital showed non-permissive carbapenem MICs (data not shown).
Our study has limitations. First, it is a single centre study; thus generalisation of the results must be made with caution. Nevertheless, all-cause mortality with CR infections reflected national data and contemporary literature from countries with similar epidemiology. Second, the cohort was a case-mix of patients treated in the wards and the ICU; however, high APACHE II scores of the cohort indicate that both subgroups were critically ill patients. Third, not all infections were microbiologically documented, but among bacteremic infections, the results were similar to the total cohort.
The Carbapenem-Sparing Program, was a safe approach for patients with Gram-negative MDR infections, in a Greek hospital with the predominance of MDR and particularly CR pathogens, allowing to conclude that sparing prescriptions of carbapenems is feasible. Bedside dedicated consultation of the AST ensured acceptance of the strategy in 71.8% of prescribers. Further study is required to clarify the potential efficacy of this approach in decreasing antimicrobial resistance trends.