Introduction
Rapid diagnosis of pathogens grown in blood cultures reduces mortality and morbidity as appropriate treatment is started early. It notably reduces hospital costs because of less need for intensive care and earlier patient discharge (1, 2). Although rapid identification and antibiogram of pathogens can be made with automated blood culture, identification, and antibiogram systems, faster systems are needed. Therefore, over the years, microorganisms have been identified by various molecular methods and resistance genes have been identified (1, 2). Finally, with the introduction of matrix-assisted laser desorption/ionization-time of flight (MALDI-TOF) mass spectrometry (MS), rapid microbial identification and detection of some resistance phenotypes have become possible (3, 4).
This study used two multiplex tandem real-time PCR kits to rapidly diagnose Gram-positive cocci and Gram-negative bacilli that grew in blood cultures as sepsis agents and to detect resistance genes. The first one, the Gram-positive 12 (GP-12) kit (AusDiagnostics, Australia), detects Staphylococcus spp., Streptococcus spp., Enterococcus spp., and antibiotic resistance genes (mecA, vanA, vanB) in them. The second one, Gram-negative 12 (GN-12) kit (AusDiagnostics, Australia), detects Enterobacteriaceae, Pseudomonas spp., Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae, and their antibiotic resistance genes (Oxa-23 [carbapenem hydrolyzing beta-lactamase OXA-23], pan-IMP [IMP-1, metallo beta-lactamase IMP containing 4], pan-vim [metallo-beta-lactamase VIM-1, 2 or 3], aadA1 [aminoglycoside nucleotidyltransferase aadA1], aadB [aminoglycoside nucleotidyltransferase aadB], aac(6’)IIc [aminoglycoside-6’ acetyltransferase aac(6’)IIc]). We aimed to evaluate the performances of these two kits.
Materials and Methods
Collection of samples
Blood samples taken from patients at the sepsis clinic were inoculated into BACTEC™ (Becton, Dickinson and Company, USA) and BACT/ALERT® (bioMérieux, France) blood culture bottles. The study included 132 blood culture bottles with positive signals. First, Gram staining from the blood culture bottles gave a positive signal. Seventy-eight samples having Gram-negative bacilli in Gram staining were applied to the GP-12 panel. In Gram staining, 54 samples of Gram-positive cocci were applied to the GP-12 panel. At the same time, the passages of the samples were made and incubated. After that, identification and antibiograms were made in Phoenix™ automated system (Becton, Dickinson and Company, USA) and VITEK 2 Compact automated system (bioMérieux, France), and the results were evaluated.
DNA isolation
For DNA isolation, according to the recommendations of the kit manufacturer, the EZ1® Advanced XL (Qiagen, Germany) nucleic acid extraction device and EZ1® DNA Tissue Kit (Qiagen, Germany) were used. EZ1® DNA Tissue Kit (Catalog No: 953034; Qiagen, Germany) and EZ1® Advanced XL DNA Bacteria Card (Catalog No: 9018694; Qiagen, Germany) were used in the extraction device. For DNA extraction, 200 microliters of blood culture fluid from each sample were used as the starting material. DNA isolation took 17 minutes for 14 samples. The isolation was completed by following the instructions on the screen for the extraction device. At the end of the procedure, 50 microliters of DNA were obtained from each sample.
Pre-PCR and PCR
The study used a multiplexed Tandem PCR technique consisting of a two-step sequential PCR reaction. For each sample, five microliters of DNA were used as starting material. In the first step, a short 15-cycle multiplex pre-amplification reaction (pre-PCR) and PCR set-up steps were performed using homologous primers for all targets in the panel. Easy Plex pipetting robot (AusDiagnostics, Australia) was used for pre-PCR and PCR set-up stages. There was no difference in procedure between Gram-positive and Gram-negative panels. For the pre-PCR and PCR set-up stages, in line with the manufacturer’s instructions, the required filter pipette tips, 72 rotor disc, oil and water tubes used for pre-PCR, master mix 1, master mix 2 tubes and dilution plate were loaded into the Easy Plex pipetting robot. The products formed after the first step were diluted into the wells for the second real-time PCR reaction using the nested inside primers of the primers used in the first step.
After DNA isolation and pre-PCR stages, the materials were applied to the GP-12 and GN-12 panels (AusDiagnostics, Australia). The second step of the PCR reaction was performed in the Rotor-Gene Q (Qiagen, Germany). DNA amplification was detected by measuring the increase in fluorescence using EvaGreen™ dye (Biotium, USA). A 72-position Easy-Plex™ ring (AusDiagnostics, Australia) was used for the second step of PCR.
After approximately one hour of pipetting and pre-PCR steps, the 72-rotor disk was taken, and the reaction wells were covered with sealing film. Then, the 72-rotor disk was loaded into Rotor-Gene Q (Qiagen, Germany) real-time PCR device and amplified according to the kit manufacturer’s instructions.
Culture, identification, and antibiogram
After Gram staining from BACTEC™ (Becton, Dickinson and Company, USA) and BACT/ALERT® (bioMérieux, France) blood culture bottles that gave a positive signal, the 5% sheep blood agar and eosin methylene blue (EMB) agar media were inoculated from the bottles. The next day, cultures were evaluated, and antibiograms of grown microorganisms were identified using Phoenix™ automated system (Becton, Dickinson and Company, USA) and VITEK 2 Compact automated system (bioMérieux, France).
Results
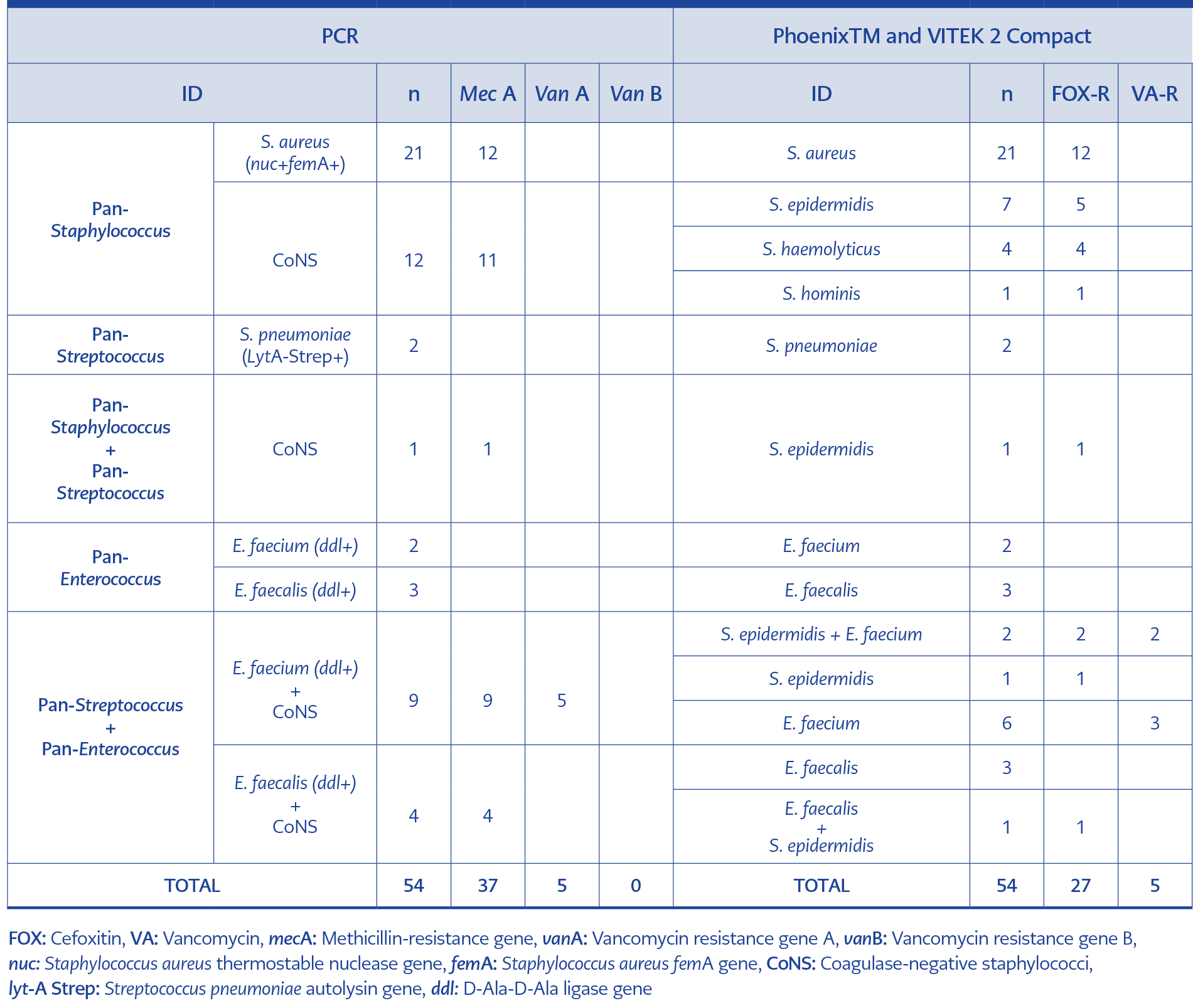
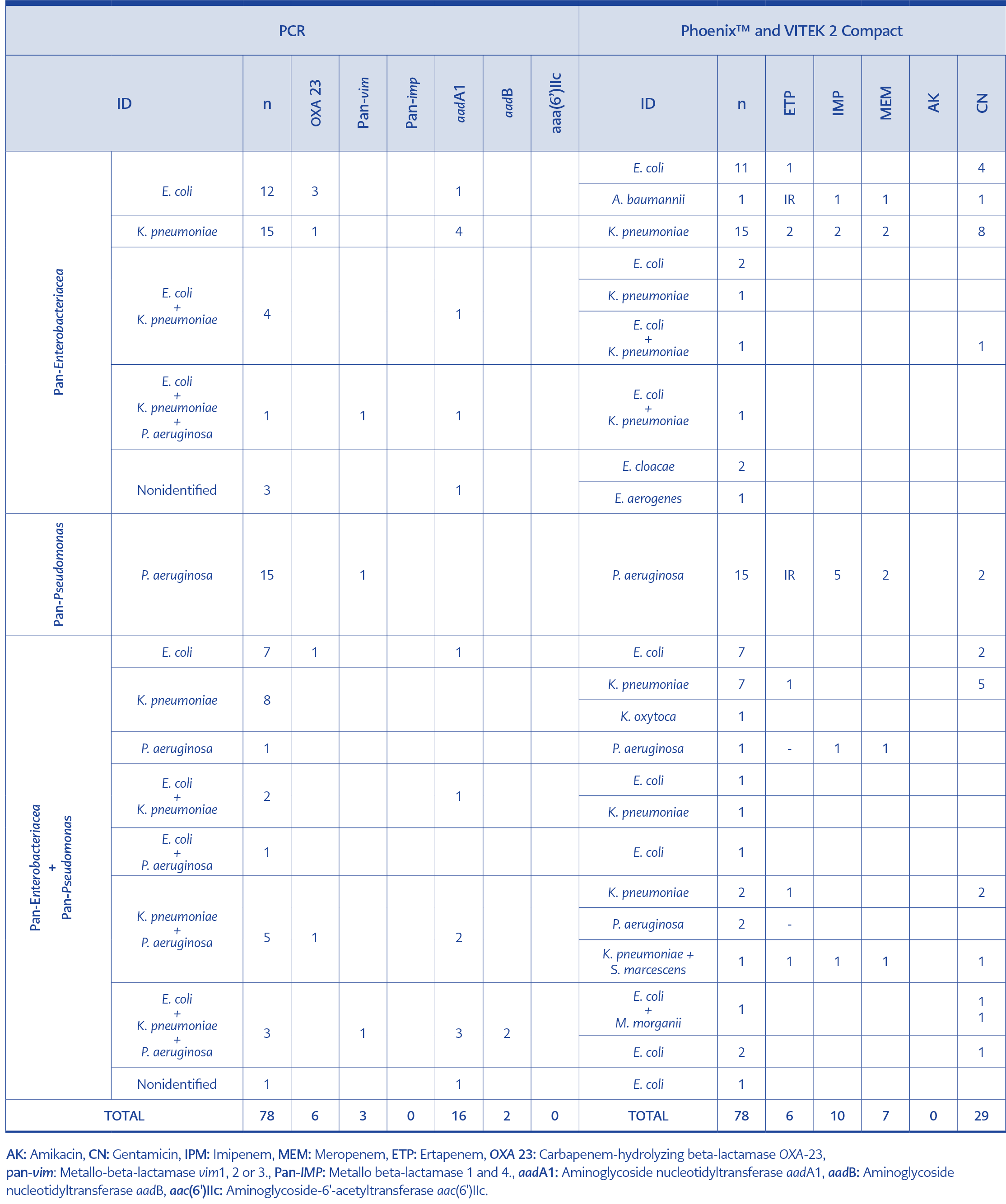
After the multiplex tandem real-time PCR, results were compared to those obtained from automated systems. All the results are given in Table 1 and Table 2.
Firstly, all the pathogens were successfully identified by using these two multiplex tandem real-time PCR kits. Twenty-one S. aureus and twelve methicillin-resistant strains were identified using GP-12 panels and the Phoenix™ and VITEK 2 Compact automated systems. Twelve coagulase-negative staphylococci (CoNS) found with GP-12 panels were also detected with Phoenix™ and VITEK 2 Compact automated systems. However, while the mecA gene was found in eleven samples with the GP-12 panel, methicillin resistance was detected in ten samples in automated systems. Two strains of S. pneumoniae were detected as the same in both GP-12 panels and automated systems. Two E. faecium and three E. faecalis were found to be the same in both GP-12 panels and automated systems. However, a difference was found between the GP-12 panel and the automated systems in the samples with mixed infection. While pan-Staphylococcus, pan-Streptococcus, and coagulase-negative staphylococci (CoNS) carrying the mecA gene were detected in one sample, an automated system identified one methicillin-resistant Staphylococcus epidermidis in the same sample. In nine samples, methicillin-resistant coagulase-negative staphylococci (MRCoNS) and nine E. faecium associations were detected, five of which carried the vanA gene. In the same samples, MRCoNS and two vancomycin-resistant E. faecium coexistence in two samples, MRCoNS in one sample, and six E. faecium in six samples, six of which were resistant to vancomycin, were found in automated systems. While one E. faecium and six MRCoNS strains could not be detected with automated systems, all vancomycin-resistant E. faecium strains were also detected with automated systems. While MRCoNS and E. faecalis were detected in four samples, only E. faecalis was found in three. Methicillin-resistant S. epidermidis and E. faecalis association was found in one sample with automated systems.
In Table 2, the GN-12 panel and automated systems are compared. According to the results obtained from the GN-12 panel, the results obtained under three headings, pan-Enterobacteriaceae, pan-Pseudomonas, and pan-Enterobacteriaceae + pan-Pseudomonas, were compared with the results obtained with automated systems.
In the first group, pan-Enterobacteriaceae and twelve E. coli, three of the OXA-23 gene and one aadA1 gene were detected by the GN-12 panel. In comparison, automated systems isolated eleven E. coli and one Acinetobacter baumannii in the same samples. Ertapenem resistance was found in one of the E. coli isolates; gentamicin resistance was found in four, while the A. baumannii strain was resistant to carbapenems and gentamicin. The absence of A. baumannii in the panel leads to the chance of predicting one of the two gentamicin resistances while detecting OXA-23 in three samples, which was considered a positive aspect.
OXA-23 gene was found in one of fifteen strains identified as pan-Enterobacteriaceae and K. pneumoniae with the GN-12 panel, and the aadA1 gene was found in four of them. Although fifteen K. pneumoniae strains were isolated in the same samples by automated systems, resistance to carbapenems was detected in two and resistance to gentamicin in eight. Although the panel identified all strains, it was weak in determining the resistance profiles.
The aadA1 gene was found in one of four samples isolated from pan-Enterobacteriaceae and E. coli + K. pneumoniae with the GN-12 panel. E. coli in two samples, K. pneumoniae in one and E. coli + K. pneumoniae with the aadA1 gene, were found in one of the same samples with automated systems. The panel was evaluated positively. E. coli + K. pneumoniae + P. aeruginosa containing pan-vim and aadA1 genes were detected in one sample with pan-Enterobacteriaceae with GN-12 panel. E. coli + K. pneumoniae was detected in this sample using automated systems. No carbapenem or aminoglycoside resistance was detected. The panel was found to be superior in polymicrobial infections.
With the GN-12 panel, only pan-Enterobacteriaceae could be detected in three samples, and no identification at the species level could be made. The aadA1 gene was detected in one of these samples. With automated systems, two samples were identified as Enterobacter cloacae and one as Enterobacter aerogenes. Although identification could not be made at the species level, it was determined that the infectious agents were members of Enterobacteriaceae. In addition, the aadA1 gene was found in one of them.
In the second group, pan-Pseudomonas, fifteen P. aeruginosa strains were identified, one of which had the pan-vim gene. Automated systems isolated fifteen P. aeruginosa strains; two were resistant to carbapenems and gentamicin, and three were resistant to only imipenem.
In the third group, pan-Enterobacteriaceae + pan-Pseudomonas, seven E. coli with one aadA1 and oxa23 genes were detected. At the same time, seven E. coli strains, two of which were resistant to gentamicin, were identified by automated systems. Automated systems identified eight K. pneumoniae strains, including one Klebsiella oxytoca and seven K. pneumoniae resistant to five gentamicin and one ertapenem. One P. aeruginosa strain was detected as P. aeruginosa resistant to imipenem and meropenem by automated systems.
In the pan-Enterobacteriaceae + pan-Pseudomonas group, two samples, in which one E. coli and K. pneumoniae with aadA1 gene were detected together, were identified as one E. coli and one as K. pneumoniae by automated systems. E. coli and P. aeruginosa were detected in one sample, and automated systems could only detect E. coli. The association of P. aeruginosa and K. pneumoniae with two aadA1 and oxa23 genes was detected in five samples. Automated systems isolated two K. pneumoniae and two P. aeruginosa from one sample; two were resistant to gentamicin, and one was resistant to ertapenem. Also, K. pneumoniae and Serratia marcescens were isolated from the same sample; they were resistant to gentamicin, imipenem, meropenem, and ertapenem.
In the pan-Enterobacteriaceae + pan-Pseudomonas group, E. coli, K. pneumoniae, and P. aeruginosa were detected in three samples. At the same time, two of them had aadB, three aadA1, and one pan-vim gene. Two E. coli, one resistant to gentamicin, and E. coli and Morganella morganii in one sample, both resistant to gentamicin, were identified by automated systems. One specimen in this group could not be identified at the species level, but the aadA1 gene was detected. In automated systems, this sample was defined as E. coli.
Discussion
Many studies have been conducted on the rapid identification of microorganisms grown in blood cultures using molecular methods and the detection of resistance genes, and the clinical benefits of these tests have been reported in terms of results. These tests, which provide early detection of essential resistance phenotypes, are practical in rapidly optimizing antimicrobial therapy by reducing off-label antibiotics (5-7). For this purpose, Gosiewski et al. (7) have tried to detect Gram-negative bacteria (E. coli), Gram-positive bacteria (S. aureus), yeast (Candida albicans), and filamentous fungi (Aspergillus fumigatus) in blood by nested-multiplex real-time PCR. According to the results, they stated that the method they designed allowed the detection of bacteria in whole blood samples, was much more sensitive than the culture method, and allowed the detection of the main groups of microorganisms within a few hours.
Wolk et al. (8) used the GenMark Dx ePlex blood culture identification Gram-negative panel in their study, identifying Gram-negative pathogens and determining the resistance genes (CTX-M, KPC, IMP, VIM, NDM, and OXA [OXA-23 and OXA 48]). They stated that the panel they recommend was also valuable for finding pathogens that might be missed in Gram staining containing the pan-Gram-positive and pan-Candida regions.
In their study, MacVane and Nolte (9) diagnosed and followed up patients with growth in blood culture using conventional methods and a rapid multiplex PCR panel and compared the results. Their results showed no difference between the two groups regarding mortality, 30-day readmission, length of stay in the intensive care unit, hospitalization period after culture, or costs. However, it was stated that the time to effective treatment was shortened in the group using molecular diagnosis compared to the group using conventional methods alone, and the use of antimicrobials was further developed.
Granato et al. (10) also conducted a qualitative study to detect mecA, vanA, and vanB resistance genes of S. aureus, S. epidermidis, S. pneumoniae, E. faecalis, and E. faecium responsible for bacterial bloodstream infections. They compared the multiplex test, the iC-GPC Assay (iCubate, USA), with the Verigene Gram-positive blood culture (BC-GP) assay (Luminex Corp., USA). They stated that the iC-GPC Test showed a 95.5% agreement with the BC-GP test. They emphasized that the iC-GPC Test is accurate and reliable for detecting the five common Gram-positive bacteria and their resistance genes.
Wang et al. (11) compared multiplex real-time PCR and PCR reverse blot hybridization (PCR-REBA) tests with each other and with conventional culture methods. While PCR-REBA was superior in detecting the mecA gene, Gram-positive bacteria, Gram-negative bacteria, and Candida spp. were equivalent for both tests. They emphasized that using these two molecular methods is fast and reliable for the characterization of causative pathogens in bloodstream infections since the results from the culture can take up to 48-72 hours, while all two methods take about three hours.
Pilarczyk et al. (12) used LightCycler® SeptiFast test M Grade (Roche Molecular Systems, Germany), a real-time multiplex PCR test capable of detecting twenty-five bacterial and fungal pathogens, to diagnose bloodstream infections after cardiothoracic surgery early. They found the test valid for Gram-negative pathogens. Still, they recommended its use with conventional blood culture methods, as it was weak in detecting Gram-positive pathogens and could not detect antibiotic susceptibility.
Lee et al. used the BD MAX StaphSR Assay (SR assay; BD, USA) to distinguish S. aureus from CNoS and detect methicillin resistance in positive blood cultures (13). As a result, they stated that the range of 0-27 cycle threshold (Ct) for positivity with the nuc/mec test was helpful for rapid detection of methicillin-resistant S. aureus (MRSA) and MRCNoS. They also emphasized genotypic v mecA-positive and oxacillin-susceptible isolates.
Similar to our study, Hazelton et al. evaluated the performance of the GP-12 multiplex tandem PCR (MT-PCR) test (AusDiagnostics, Australia) (14). A total of 673 aerobic and anaerobic positive blood culture bottles showing Gram-positive cocci morphology on microscopy were included in the study and compared with traditional phenotypic methods. They reported that the internal control amplification was inhibited in 11.7% of the samples. However, 96.6% (537/556) of the remaining monomicrobial samples obtained results consistent with the genus level and 100% (172/172) at the species level. They reported that for 94.7% (36/38) of the polymicrobial samples, the results matched the phenotypic methods, and the methicillin and vancomycin susceptibility result fully agreed with the phenotypic methods. They rated the results positively because of the accuracy of over 90%. They reported that this test, in which Gram-positive pathogens and their primary antibiotic resistance markers could be obtained within three hours, was reliable.
Sze et al. used the Accelerate Pheno® system (Accelerate Diagnostics, Inc., Tucson, AZ), which uses fluorescence in situ hybridization probes and a new rapid test that determines rapid identification and antibiotic susceptibility from positive blood cultures (15). They were compared with the FilmArray Blood Culture Identification (BCID) (Biofire, USA) and FilmArray BCID 2 (Biofire, USA) panels that perform nested PCR. They found rapid methods successful and stated that tests suitable for laboratory conditions could be used.
In another study conducted with positive blood culture samples using fluorescence in situ hybridization probes, Reitz et al. emphasized that the FISH technique, which they found helpful for laboratories with limited resources without advanced rapid diagnostic methods such as mass spectrometry, was a good option (16).
Bryant et al. used the ePlex system (GenMark Diagnostics, USA), a random-access multiplex PCR platform developed for syndromic diagnosis in the diagnosis of bacteremia and fungemia (17). They stated that sensitive and reliable results could be obtained with the ePlex BCID panels, where they could identify fifty-six pathogens and ten resistance genes. Simultaneously, the transfer of results was necessary to measure the effect on mortality and length of stay.
In our study, after Gram staining, 54 vials with Gram-positive cocci were applied to the GP-12 panel, 78 vials with Gram-negative bacilli were applied to the GN-12 panel, and the results obtained by PCR and conventional methods were compared. All pathogens identified with the Phoenix™ automated system (Becton, Dickinson and Company, USA) and VITEK 2 Compact automated system (bioMérieux, France) were successfully identified with these two multiplex tandem real-time PCR kits. However, both panels were found to be more effective in the diagnosis of polymicrobial infections. Thirteen mecA genes (methicillin resistance) that conventional methods could not detect, one pan-streptococcus, one E. faecium, and nine CNoS GP-12 panels could be detected. Similarly, nine K. pneumoniae, three E. coli, and eight P. aeruginosa were detected by GN-12 panels as the polymicrobial infection agent that conventional methods could not detect. Although two E. cloacae, one E. aerogenes, one S. marcescens, one M. morganii, and one E. coli could not be detected as a species, it was found to be pan-Enterobacteriaceae in the panel. One A. baumannii strain could not be detected because it was not found in the panel. Although the number of strains resistant to carbapenems was twelve, six OXA-23 and three Pan-vim could be detected with GN-12 panels. At the same time, one of the aminoglycoside resistance genes was found in sixteen of twenty-nine strains resistant to any of the aminoglycosides. Different susceptibility phenotypes might have been captured with larger content panels. Generally, the panel was found beneficial.
Rapid identification of pathogens from blood cultures is gaining more and more importance with new resistance phenotypes that are developing and increasing in frequency. The number of carbapenem-resistant, extended-spectrum beta-lactamases (ESBL), methicillin, and vancomycin-resistant isolates is constantly increasing, and their early detection is vital for reducing mortality and morbidity. Therefore, multiplex PCR, real-time multiplex PCR, DNA-microarray-based hybridization technology, in situ hybridization-based methods, nucleic acid amplification-based methods, and combined platforms are used (17-20).
This study has several limitations. One significant limitation is the requirement for trained molecular microbiology technicians or specialists, who may not always be available outside regular working hours or on public holidays. Additionally, the study is constrained by its sample size and the inability to detect fungal agents. For these reasons, syndromic sepsis panels are recommended for routine laboratory use because they do not require specially trained technicians and can be used by other laboratory personnel.
In conclusion, the two kits proved rapid (approximately three hours) and reliable in determining common Gram-negative and Gram-positive sepsis pathogens and resistance genes. As in many studies, using multiplex tandem real-time PCR kits helped detect sepsis agents and resistance genes. Considering all aspects, such as early initiation of treatment, a more successful and shorter treatment, reduced complications, and reduced mortality and morbidity, it is possible to say that rapid tests are not an extra burden in terms of cost. Today, with the widespread use of sophisticated technologies such as MALDI-TOF MS and FilmArray, different molecular tests can be used for laboratories that do not have these facilities. We believe that different multiplex tandem real-time PCR tests, which provide rapid identification and detect antibiotic resistance genes, will be beneficial depending on the possibilities of the laboratories.