Introduction
The incidence of acute pancreatitis ranges from 2.2-136/100,000 people and increases by 3.7% per year (1). Necrosis occurs in nearly 15% of acute pancreatitis. The sterile necrosis of pancreatic or peripancreatic tissue gets infected by translocation of gastrointestinal flora or peripheral spread from the skin, respiratory, or urinary tract. Mortality rates increase with infection in necrotic tissue and rise from 19.8% to 35.2% in acute pancreatitis (2). Therefore, it is intended to prevent infections in necrotic tissue and reduce the mortality rate by early use of antibiotics. Numerous available studies have used various antibiotic drugs with different administrations and heterogeneous study outcomes. Fluoroquinolones, cephalosporins, carbapenems, and many antibiotic therapies have been used against infection of pancreatic necrosis (3-5). The concentrations of the antibiotics in the pancreatic and peripancreatic necrotic tissue vary. High pancreatic tissue concentration of carbapenems, especially imipenem, above the minimum inhibitor concentration (MIC) causes their often prophylactic use (6). However, despite the advantages of carbapenems’ pharmacokinetic/pharmacodynamic (pk/pd) in pancreatic tissue, the effect of their prophylactic use on necrotic tissue infection and pancreatitis-related outcomes, such as mortality, is still uncertain. Particularly, high-quality randomized controlled trials with a low risk of bias have detected no relationship between prophylactic carbapenem use and pancreatitis-related outcomes (7, 8). However, some observational studies have detected a reduction in infection risk through the use of prophylactic carbapenems, leading them to be used frequently in daily practice (9).
This systematic review and meta-analysis aimed to determine the effect of prophylactic use of carbapenems for acute pancreatitis and acute necrotizing pancreatitis on mortality, surgical intervention, and pancreatic or non-pancreatic infection.
Materials and Methods
This study was designed as a systematic review and meta-analysis. It was conducted with three reviewers according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines based on PICO (population, intervention, comparison, outcome) research questions. Two reviewers searched the PubMed database independently using the keywords “Pancrea* AND carbapenem OR imipenem OR ertapenem OR meropenem OR doripenem” for related studies until October 30, 2022. The detailed search strategy is described in Appendix, pages 1-2.
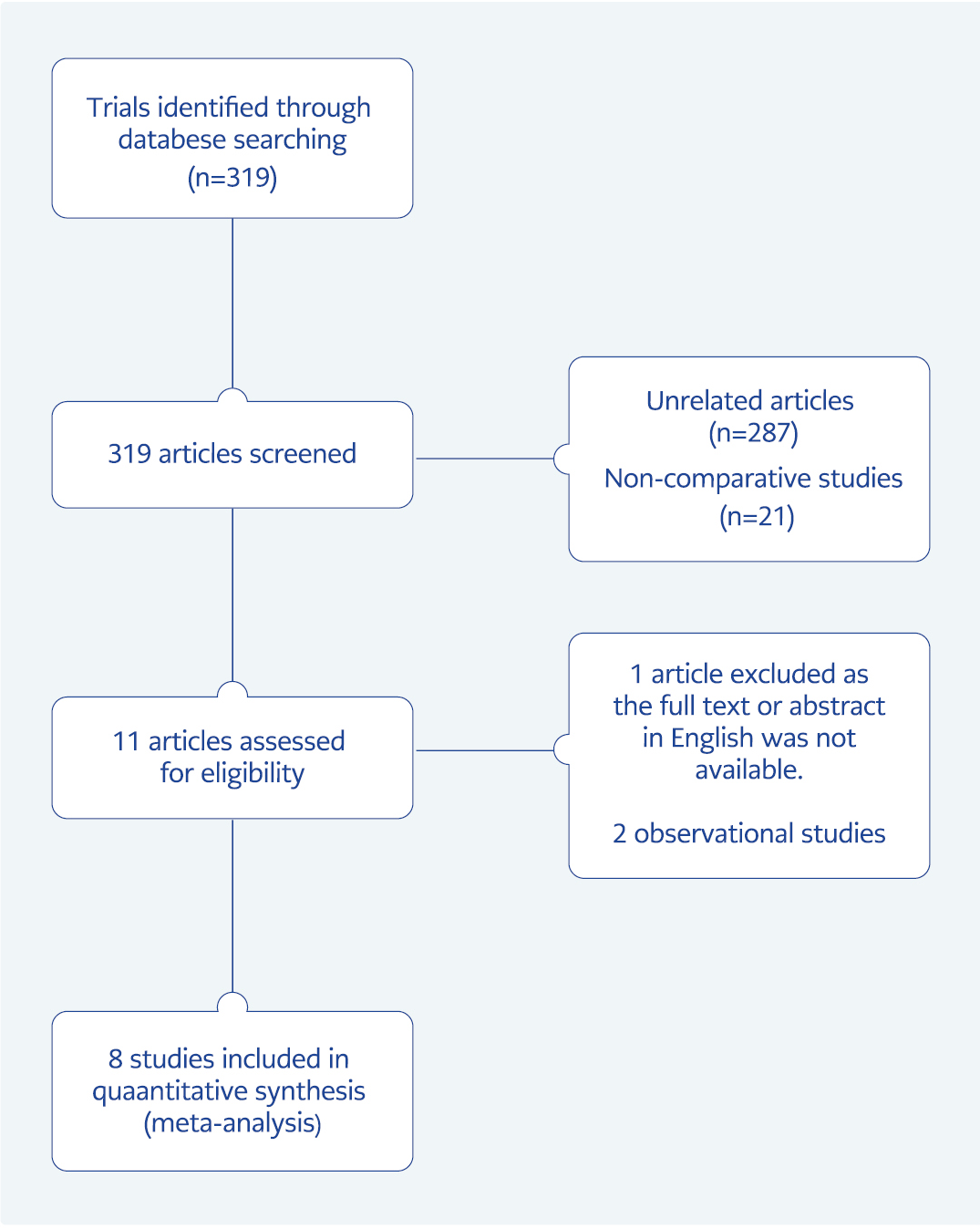
The randomized controlled trials that compared prophylactic carbapenem versus placebo or standard treatment for acute pancreatitis cases, regardless of etiology, were selected for the qualitative and quantitative synthesis (Figure 1). The eligible studies were evaluated and recorded for patients’ characteristics, diagnostic criteria for pancreatitis, therapies for intervention and control groups, carbapenem treatment (type, dose, start time, duration), and outcomes (mortality, surgical intervention, pancreatic and non-pancreatic infection) by three reviewers. In the end, the results were shared and compared, inconsistencies were discussed, and the agreed decision was followed for the meta-analysis (Appendix, pages 2-9). Two reviewers evaluated the risk of bias.
Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) was used to assess the risk of bias for randomized controlled trials (10). The studies were classified as “high risk of bias”, “unclear risk”, and “low risk of bias” by each reviewer, with justification.
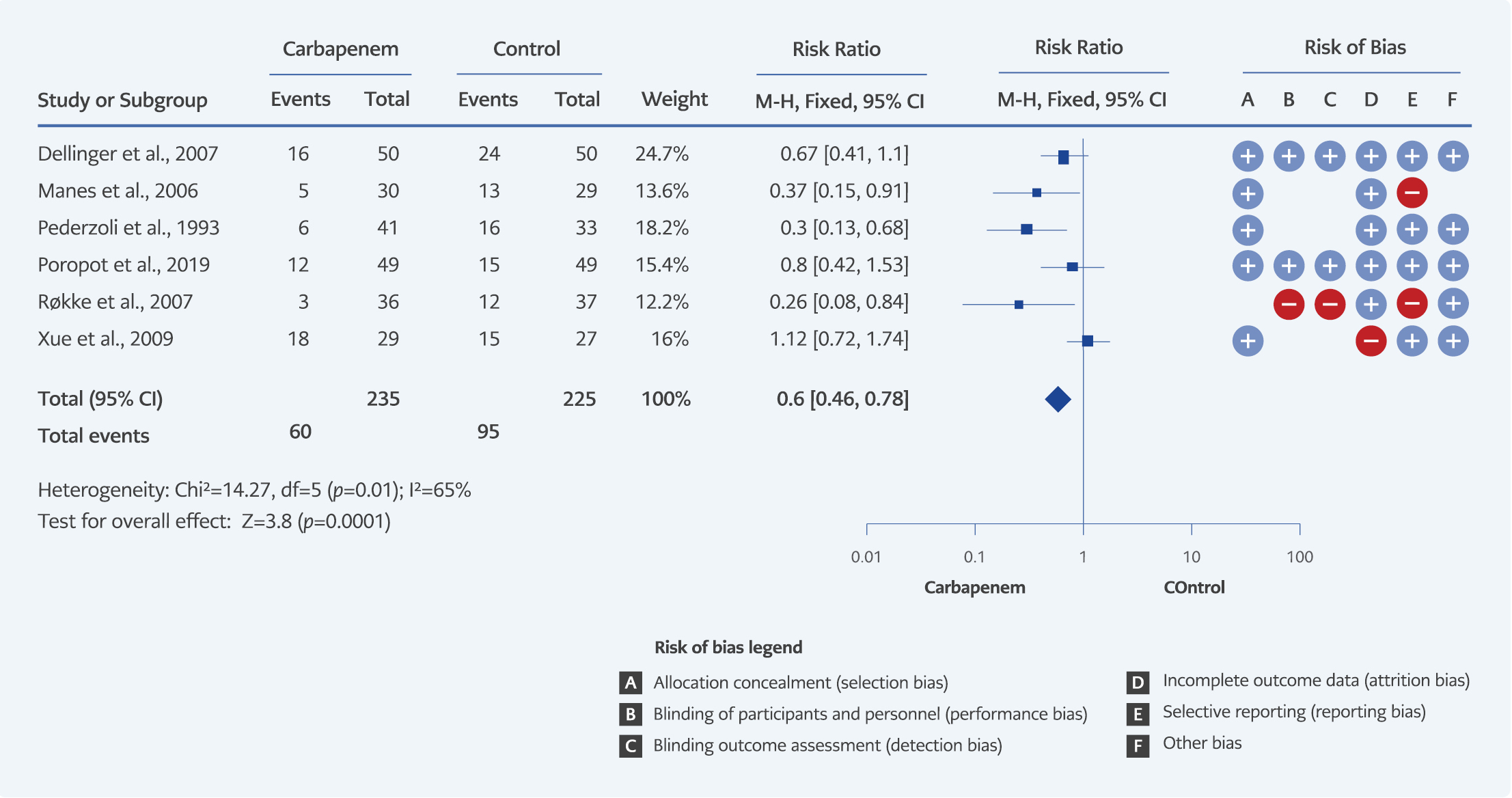
The frequency of mortality was 12.5% (35/280) for the carbapenem group and 15% (42/279) for controls. The power of our study was 13.5% for mortality outcome, with a 0.05 type-1 error. The surgical intervention rate was 19.9% (42/211) for the carbapenem group and 23.4% (49/209) for the control group, and we calculated a power of 13.8% with a 0.05 type-1 error for this outcome. Peripancreatic infection frequency was 14.5% (37/255) for the carbapenem group and 22.7% (56/246) for the control group; the power of our study for peripancreatic infection was 65.6% with a 0.05 type-1 error. Non-pancreatic infections of carbapenem and control groups were 25.5% (60/235) and 42.2% (95/225), respectively. For the non-pancreatic infection outcome, we calculated the power of our study as 96.6% with a 0.05 type-1 error.
Statistical analyses were performed using Review Manager (RevMan) software version 5.4 (The Cochrane Collaboration, London, England). A fixed-effects or a random-effects model was applied to the statistical analysis for each outcome. Results for outcomes were expressed as risk ratio (RR) with a 95% confidence interval (CI). Statistical heterogeneity among the included studies was assessed by the use of the I² value and was defined as insignificant (I²<30%), moderate (I²=30%-50%), and significant (I²>75%) heterogeneity. To reduce the risk of bias and heterogeneity between studies, subgroups such as studies involving only necrotizing pancreatitis, studies involving imipenem intervention groups, and high-quality studies were analyzed using fixed-effects or random-effects models.
Results
A total of 319 articles were screened according to the selection criteria. Finally, eight randomized control studies were included in the meta-analyses (Appendix, pages 2-9). The risk of bias assessments of the studies is presented in Figure 2 and Figure 3.
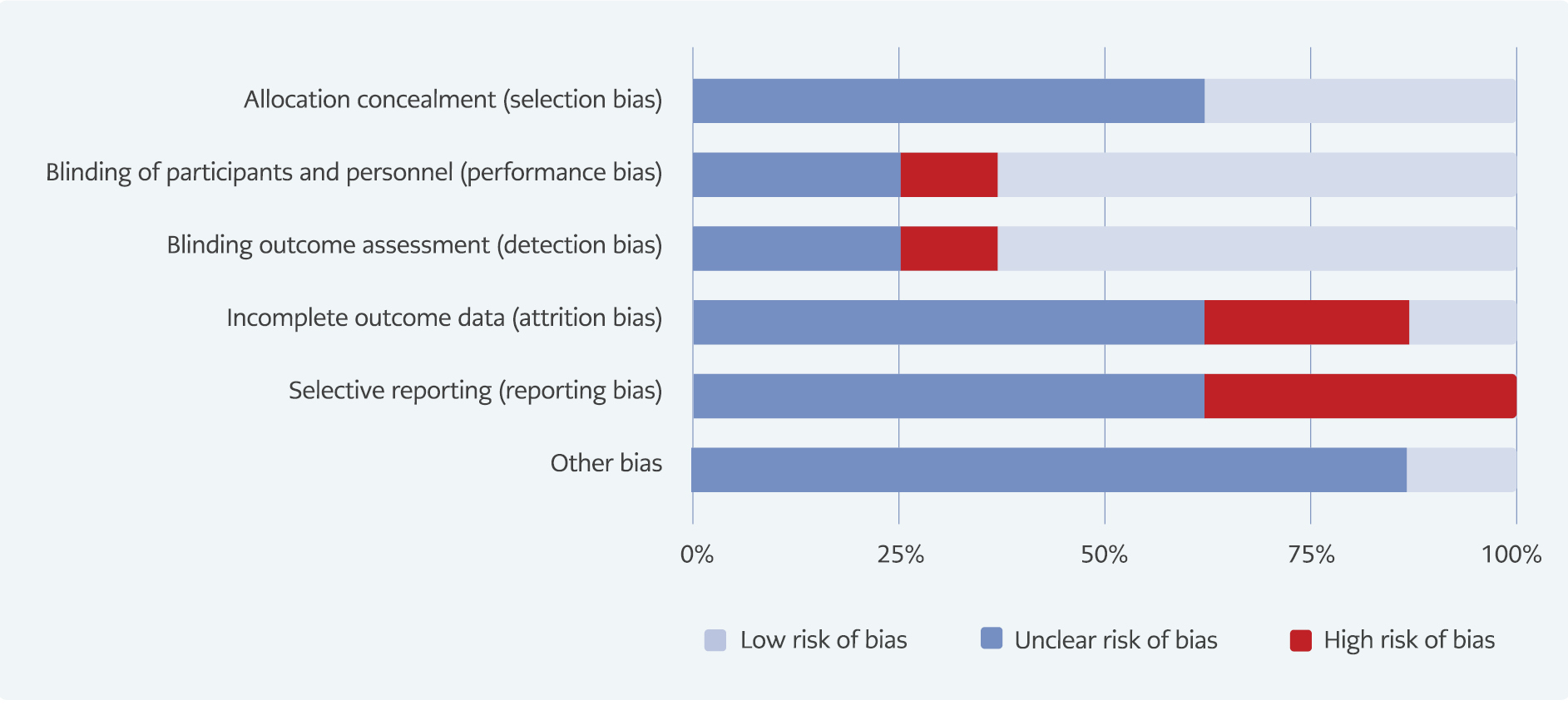
Figure 2. Risk of bias graph: review authors’ judgments about each risk of bias item presented as percentages across all included studies.
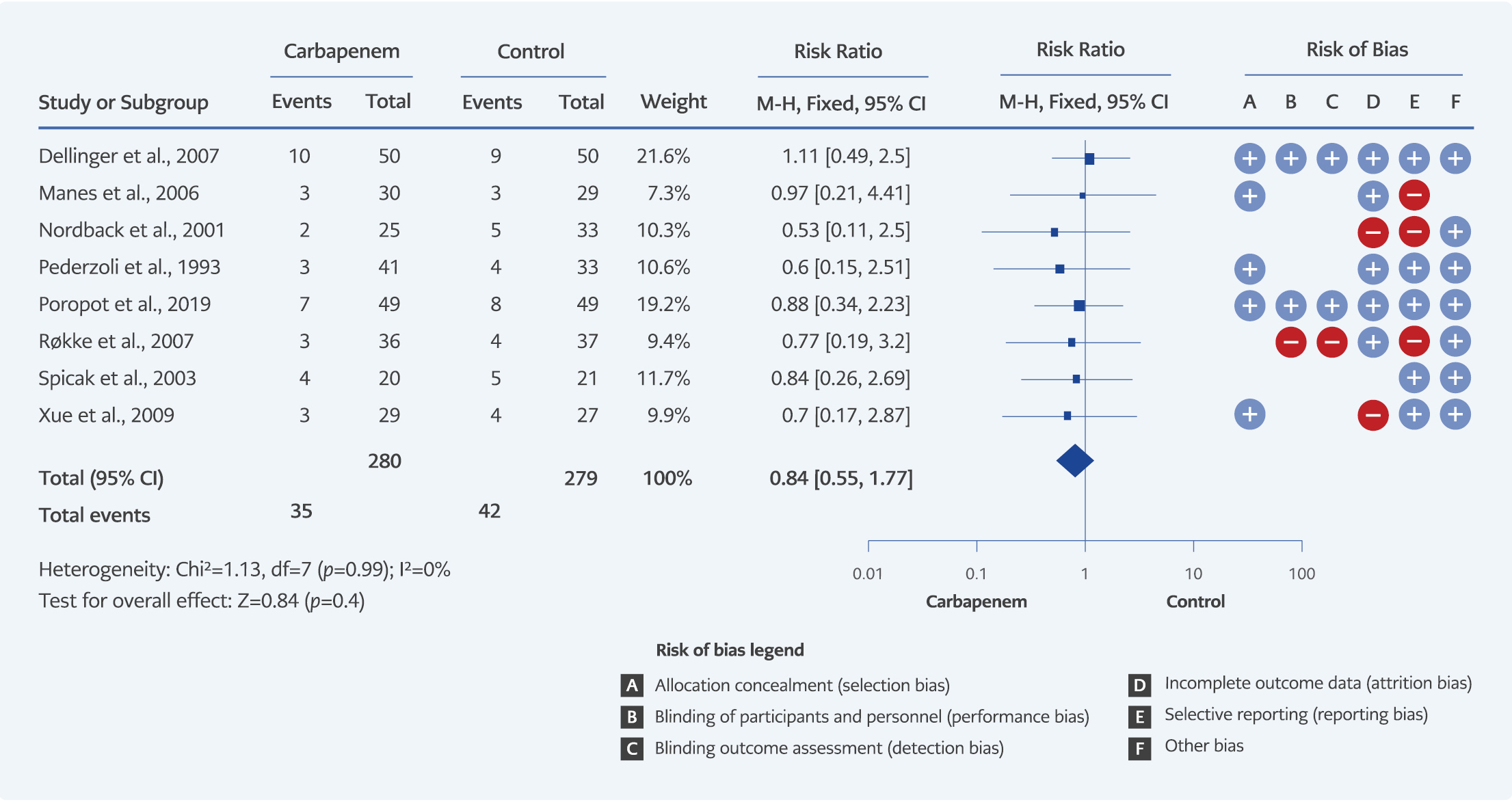
Eight studies, including a total of 559 patients, each reported mortality outcomes. According to the studies, prophylactic use of carbapenems had no statistically significant effect on mortality (RR=0.84, 95% CI=0.55-1.27, I²=0%)(Figure 4).
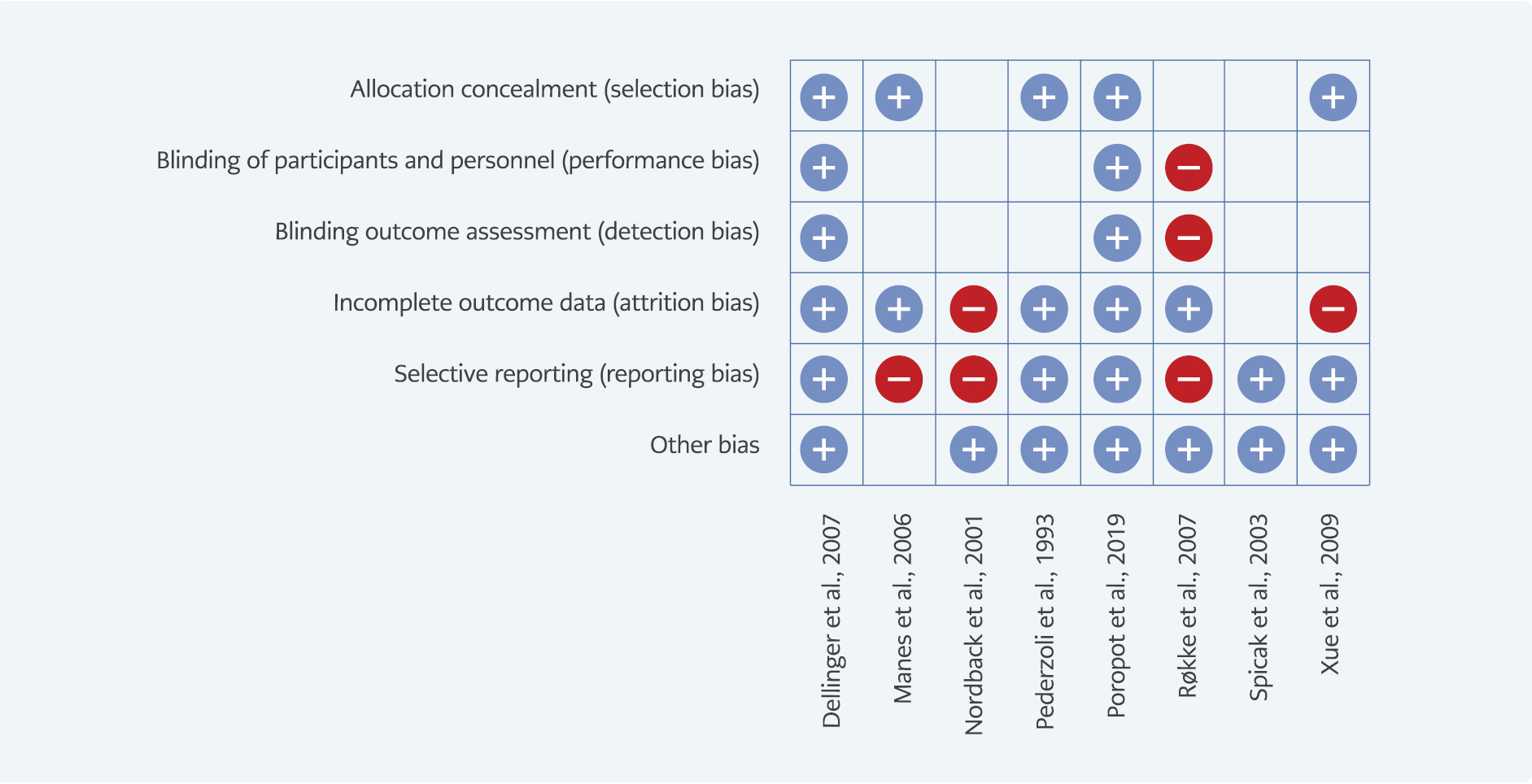
Figure 3. Risk of bias summary: review authors’ judgments about each risk of bias item for each included study.
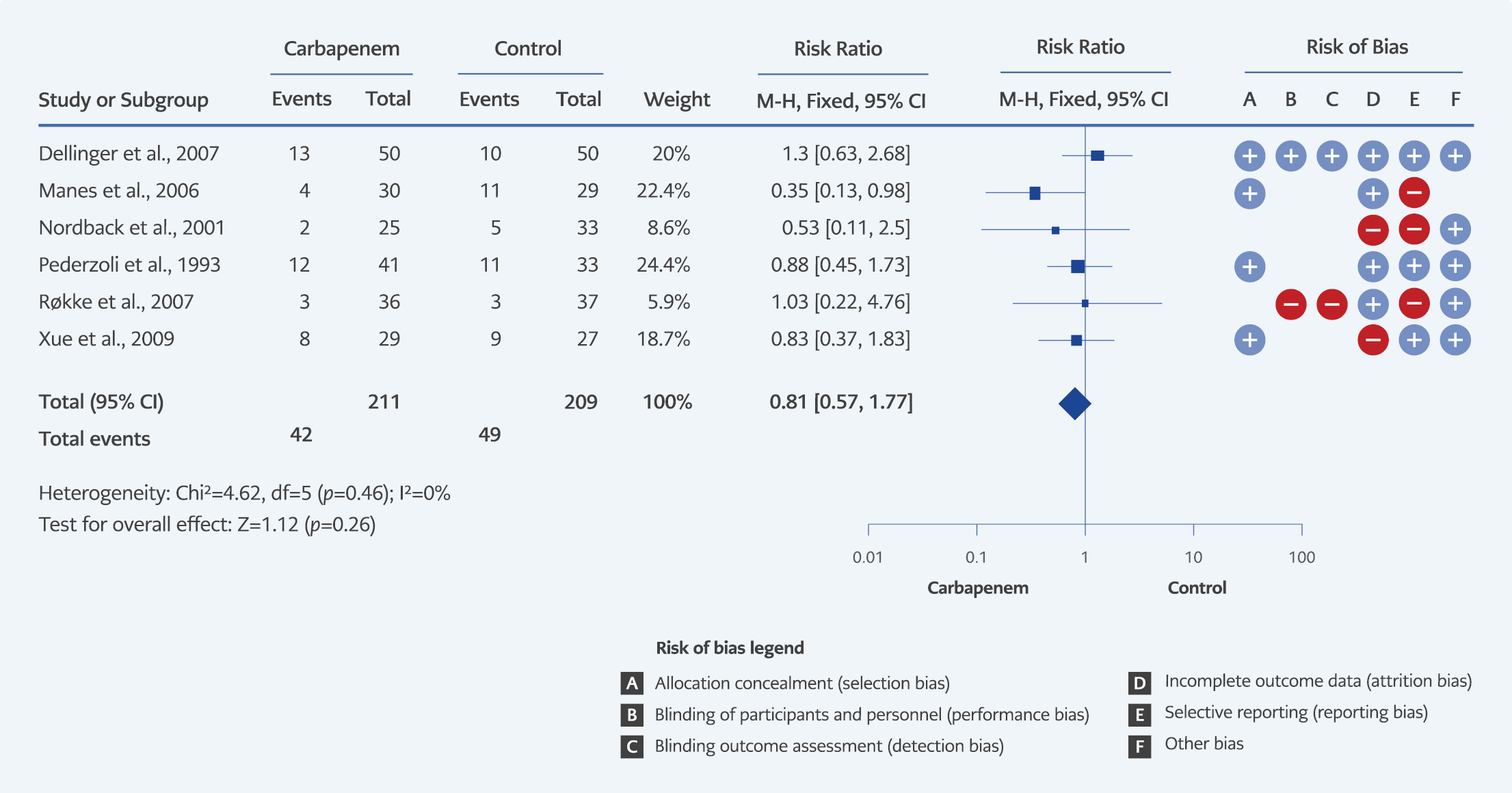
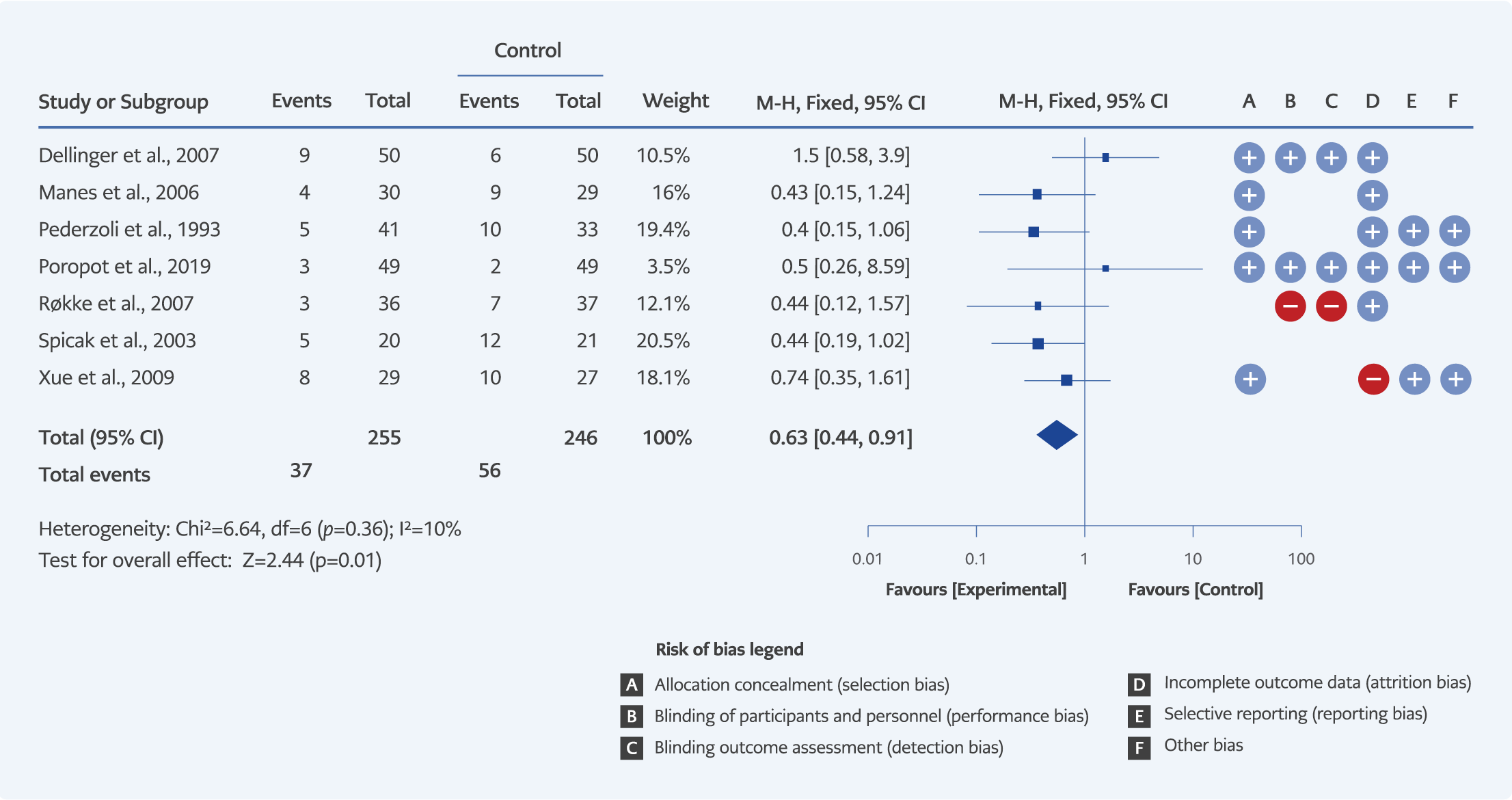
The number of studies evaluating a surgical intervention was six (n=420), peripancreatic infection was seven (n=501), and non-pancreatic infection was six (n=460). The prophylactic use of carbapenems had no statistically significant effect on surgical intervention (RR=0.81, 95% CI=0.57-1.17, I²=0%) (Figure 5). Nevertheless, the prophylactic use of carbapenems was significantly associated with a lower risk of peripancreatic infection (RR=0.63, 95% CI=0.44-0.91, I²=10%) (Figure 6), and a lower non-pancreatic infection risk (OR=0.60, 95% CI=0.46-0.78, I²=65%) (Figure 7).
For acute necrotizing pancreatitis subgroup analysis, five studies evaluated outcomes for mortality and surgical intervention (n=328), four studies for peripancreatic infection (n=270), and three studies for non-pancreatic infection (n=229). When the analysis was conducted on the studies that included only necrotizing pancreatitis, there were no significant differences between mortality (RR=0.85, 95% CI= 0.51-1.43, I²=0%), surgical intervention (RR=0.96, 95% CI=0.61-1.49, I²=0%) and peripancreatic infection (RR=0.71, 95% CI=0.46-1.11, I²=28%). Nevertheless, prophylactic use of carbapenems was associated with a lower risk of non-pancreatic infection. (RR=0.71, 95% CI=0.51-0.98, I²=71%) (Appendix, Figure 1b, 2b, 3b, 4b).
Studies with imipenem in the intervention group evaluated outcomes mortality in five studies (n=359), surgical intervention in four studies (n=261), peripancreatic infection in four studies (n=301), and non-pancreatic infection in four studies (n=301). No significant difference was detected between the prophylactic imipenem use and the control groups for mortality (RR=0.72, 95% CI=0.41-1.27, I²=0%), surgical intervention (RR=0.82, 95% CI=0.52-1.32, I²=0%) and peripancreatic infection (RR=0.60, 95% CI=0.36-1.00, I²=0%). Prophylactic imipenem use was associated with a lower risk of non-pancreatic infection (RR=0.63, 95% CI=0.45-0.87, I²=76%) (Appendix, Figure 1c, 2c, 3c, 4c).
Two randomized controlled trials with 198 participants, rated as high-quality studies, were analyzed for all four outcomes (7-9,11-17). When only high-quality studies with low bias risks were included in the analysis, our results showed no significant difference for mortality (RR=1.00, 95% CI=0.54-1.84, I²=0%), peripancreatic infection (RR=1.54, 95% CI=0.65-3.47, I²=0%) and non-pancreatic infection (RR=0.72, 95% CI=0.48-1.07, I²=0%) (Appendix, Figure 1d, 3d, 4d).
Discussion
In our meta-analysis, no relationship was observed between prophylactic carbapenem use and mortality or surgical intervention. However, the prophylactic use of carbapenems reduced the risk of peripancreatic and non-pancreatic infections. This result was based on low-quality studies with high bias risk. On the other hand, high-quality studies with low-bias risk did not show the same risk reduction.
The role of prophylactic antibiotics for acute pancreatitis is still controversial (18). In the early meta-analysis, prophylactic antibiotics reduced the risk of infection in necrotic pancreatic tissue and death. However, recent analyses did not support these results (19-21). Published meta-analyses include different antibiotic groups and cases of necrotizing and non-necrotizing pancreatitis. Because of this heterogeneity, the results were insufficient to make specific recommendations for prophylaxis in daily practice.
Furthermore, despite meta-analyses, most of these studies had insufficient sample sizes and a high risk of bias for their results. In our meta-analysis, the use of prophylactic carbapenem in acute pancreatitis cases had no effect on mortality and surgical intervention. However, the sample size in our meta-analysis was insufficient to demonstrate the effect of prophylactic carbapenem use on mortality and surgical outcome, as in previous meta-analyses. Therefore, large case series or meta-analyses are needed to support our hypothesis that there is no significant association between prophylactic carbapenem use and mortality or surgical intervention.
Infection prevention of necrotic pancreatic tissue is a significant intention for antibiotic prophylaxis. However, conflicting results have been reported in the literature due to different methodologies (22). Most published studies supported that there may be a negative association between antibiotic prophylaxis and the risk of necrotic tissue infection (19-21). In 2010, Villatoro et al. reported that prophylactic imipenem, unlike other antibiotics, reduces the risk of pancreatic infection (4). Our study detected a lower risk for peripancreatic infection by carbapenem prophylaxis. However, we did not obtain the same result in the subgroup analysis.
In addition, infection definitions and diagnostic approaches for infection were unclear in the included studies. The diagnostic approach to infection, such as microbiological sampling, was applied according to subjective criteria. Microbiological results in necrotic tissue samples were not presented in most studies. There were different doses and long-term use of antibiotics (sometimes up to 4 weeks) in prophylaxis. Therefore, the distinction between prophylaxis and treatment became unclear. Because of these uncertainties, despite the result we obtained in our meta-analysis, it is challenging to recommend prophylactic antibiotics in acute pancreatitis cases.
Non-pancreatic infection rates in acute pancreatitis vary between 3-41% (23). Marstrand-Joergensen et al. reported that non-pancreatic infections (17%), such as pneumonia, urinary tract infection, cholangitis, and bloodstream infections, were much more frequent than peripancreatic infections (2%) (24). Marstrand-Joergensen et al. showed that non-pancreatic infection was an independent predictor for mortality and increased organ failure risk five times.
The effect of prophylaxis on non-pancreatic infections is controversial. Although some meta-analyses determined that prophylaxis reduced the infection, especially urinary tract infections and sepsis (19, 20), some meta-analyses found antibiotic prophylaxis did not affect infection (21). Our meta-analysis showed that carbapenems were related to a lower risk of non-pancreatic infection risk in all subgroup analyses. However, the included studies, especially the ones that led to this result, had uncertainties for the non-pancreatic infection definition, and they were also based on subjective descriptive criteria for the approach to infection (13, 15, 16).
The collateral damages due to broad-spectrum antibiotic administration (such as side effects, C. difficile infection, breakthrough infections, and selection of resistant microorganisms) were not evaluated among the studies. Røkke et al. showed that infections occurred after the second week in the group of acute pancreatitis getting imipenem treatment, by contrast with the control group (15). It is obvious that after carbapenem prophylaxis, difficult-to-treat infections might develop by the selection of resistant pathogens. Furthermore, studies did not mention fungal infection risk secondary to broad-spectrum antimicrobial use. Previous studies indicate an increased risk of fungal infection after prophylaxis in acute pancreatitis (12, 25-27). Because of this high risk of bias, instead of a routine prophylactic approach to acute pancreatitis cases, monitoring patients closely for peripancreatic and non-pancreatic infection development with the Infection diseases specialist’s cooperation is convenient.
Our study has several limitations. First, we conducted our systematic literature search only on the PubMed database and selected studies only in English. Excluding studies in other languages and choosing just one database may have caused selection bias. The second limitation is the underpowered study sample size for mortality and surgical intervention outcomes. The reduced sample size due to subgroup analyses increased the risk of type 2 error and may have led to the absence of casual relationship. Third, the included studies had a high and unclear risk of bias. Only two of the included studies had a low risk of bias. The strength of our study design was the assessment of subgroup analysis (necrotizing pancreatitis cases, imipenem uses in the intervention group, and high-quality randomized trials) to diminish the risk of bias, contrary to published relevant meta-analyses.
In conclusion, based on current evidence, routine prophylactic use of carbapenem antibiotics in acute pancreatitis cases should not be recommended. Its effect on reducing the incidence of mortality and surgical intervention is unclear due to insufficient sample sizes; higher quality randomized controlled trials with larger sample sizes are required. Despite the reduction in the infection risk, carbapenem prophylaxis should not be preferred because of uncertainties in the diagnosis and treatment approaches of infection, inadequate collateral damage, and safety assessments in all included studies. Infection is a prognostic predictor of acute pancreatitis. Consequently, cooperation with Infectious Disease specialists and the development of diagnostic algorithms are required to prevent infection, especially non-pancreatic infection.