Introduction
Procalcitonin (PCT) is a biomarker frequently used in the diagnosis and prognosis of infection (1-4). The lack of optimum cut-off values and the high serum PCT levels in some non-infectious conditions restrict its clinical use (3-5). Therefore, PCT use is not recommended regardless of clinical parameters (6). This limitation in clinical use has led to PCT kinetic evaluations rather than predictions based on single PCT measurements. The clinicians use PCT kinetics to predict the optimal duration of antibiotic therapy without worse clinical outcomes (5). However, due to heterogeneous patient groups and confounding factors on PCT kinetics, there are different published results and recommendations for the effect of PCT on the optimal antibiotic therapy duration (7, 8).
Acute or chronic renal failure is one of the main confounders of PCT kinetics (9, 10). In renal failure, altered immune responses to infection, ongoing inflammation, and altered PCT clearance affect serum PCT levels. Compared to patients with normal renal clearance, the PCT values accepted for the diagnosis of infection are higher than the standard PCT limit. However, the relationship between renal clearance, PCT kinetic, and its clinical effects remains unknown. The acceptable PCT decreases cut-off and time interval for PCT response in these patients are unclear (11, 12). This uncertainty and more variable PCT kinetic may lead to unnecessary antibiotic revisions and therapy extensions in renal failure patients compared to patients with normal renal clearance. Besides renal failure, other confounding factors such as patients’ comorbidities, source of infection, infectious agents, and severity of infection also affect PCT kinetics and increase the uncertainty between renal clearance and PCT kinetics (13).
This study evaluated the relationship between PCT kinetic and estimated glomerular filtration rates (eGFR) in critically ill patients with primary Gram-negative primary bloodstream infections (GN-BSIs) who had clinical and microbiological responses to antibiotic therapy.
Materials and Methods
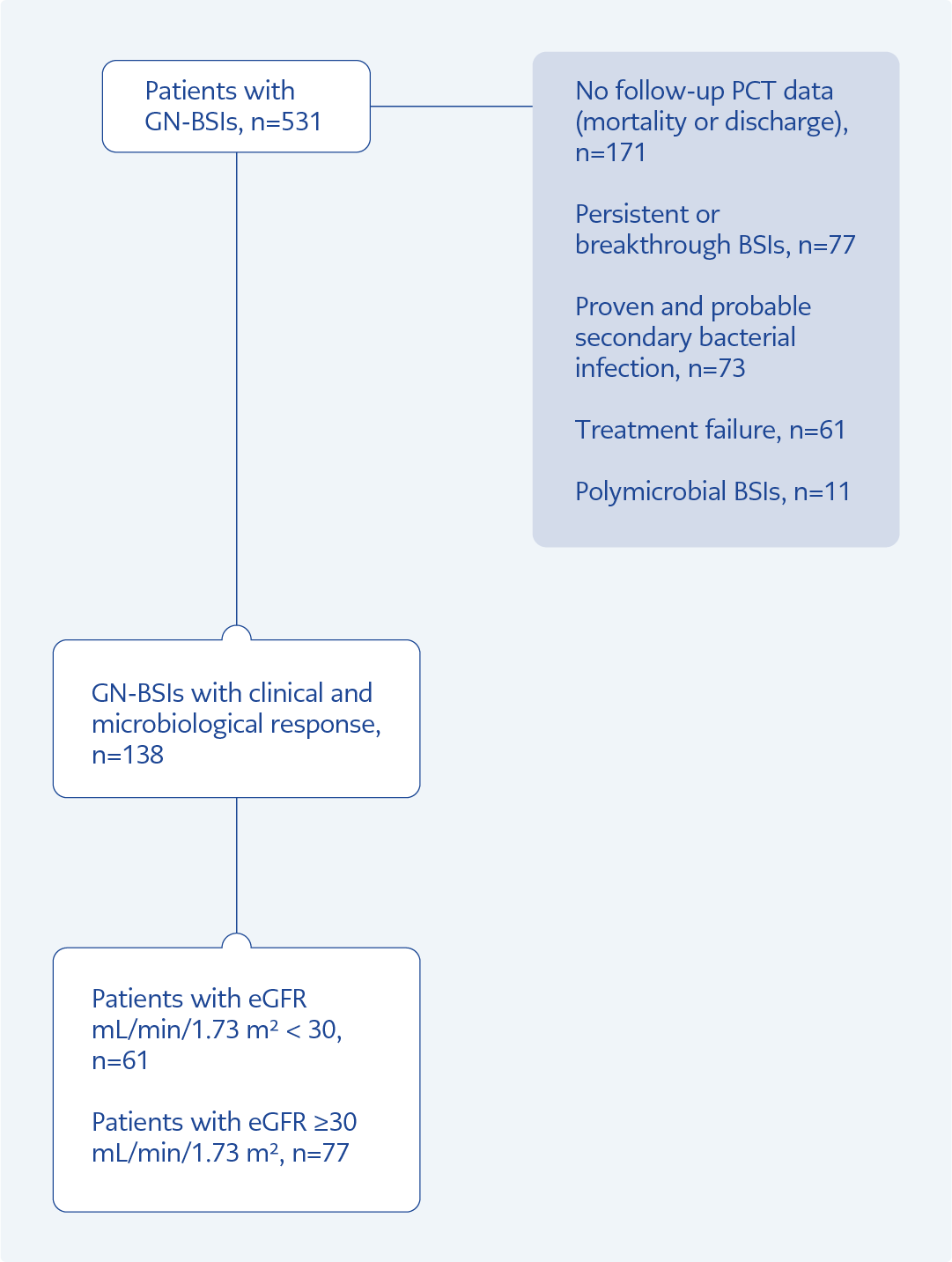
This study was a single-center, retrospective, and observational-analytic study conducted at Gazi University Hospital between January 2019 and December 2022. It included all adult patients (≥18 years) with GN-BSIs who had clinical and microbiological responses to appropriate antibiotic therapy. Patients with breakthrough bloodstream infections (BSIs) during antibiotic therapy, patients who had an antibiotic change due to a proven or possible secondary infection in any other site or therapy failure, and patients without follow-up PCT were excluded.
Renal function was assessed according to eGFR levels. eGFR was calculated based on creatinine, age, gender and race via the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) 2009 calculator (14). Patients were divided into two groups according to their eGFR levels. Clinical response was defined as the resolution of infection signs (such as fever, hypotension, and leukocytosis). Microbial response was defined as sterilization of blood culture under antibiotic therapy (15). Breakthrough BSIs were defined as isolating the same or different microorganisms in blood culture during antibiotic therapy. Therapy failure was defined as the need to revise antibiotic therapy due to a lack of clinical and microbiological response. According to antimicrobial susceptibility testing, appropriate antibiotic treatment was defined as using at least one effective antibiotic as empirical or definitive treatment.
Age, gender, comorbid diseases, Charlson comorbidity index (CCI), systemic inflammatory response syndrome (SIRS), sequential organ failure assessment (SOFA) scores, blood culture results, empiric and targeted antibiotics, duration of antibiotic treatments, and clinical outcomes (intensive care unit stay and mortality) were recorded. The first day of the appropriate antibiotic therapy was considered day zero. Blood PCT, C-reactive protein (CRP), creatinine levels, and eGFR values were measured and recorded for 14 days from day zero. Patients were divided into eGFR <30 mL/min/1.73m² and ≥ 30 mL/min/1.73m², according to their lowest eGFR level within 14 days. These two groups were compared for PCT kinetic. The procalcitonin test was measured quantitatively in serum samples using the electrochemiluminescence immunoassay “ECLIA” (Elecsys® BRAHMS PCT; Roche Diagnostics Inc., USA) method.
The study primarily aimed to evaluate the effect of renal clearance on PCT kinetics in patients with GN-BSIs who had clinical and microbiological responses. Its second aim was to assess the changes in PCT kinetics depending on eGFR between fermenting and non-fermenting Gram-negatives (GNs).
Statistical Analysis
The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 25.0 (IBM Corp., Armonk, NY, USA). The normality of the data distribution was determined by the
Shapiro–Wilk test, histograms, and Q-Q plots. The categorical variables of the patients were presented as numbers and percentages and compared by using the chi-square test. Parametric variables were presented as mean standard deviation (SD). Non-parametric variables were presented with median values and an interquartile range (IQR) of 25–75% and compared using the Mann-Whitney U test. A p value of 0.05 was considered statistically significant. Graphs were created with the GraphPad Prism 8 (GraphPad Software, Boston, USA) program.
Results
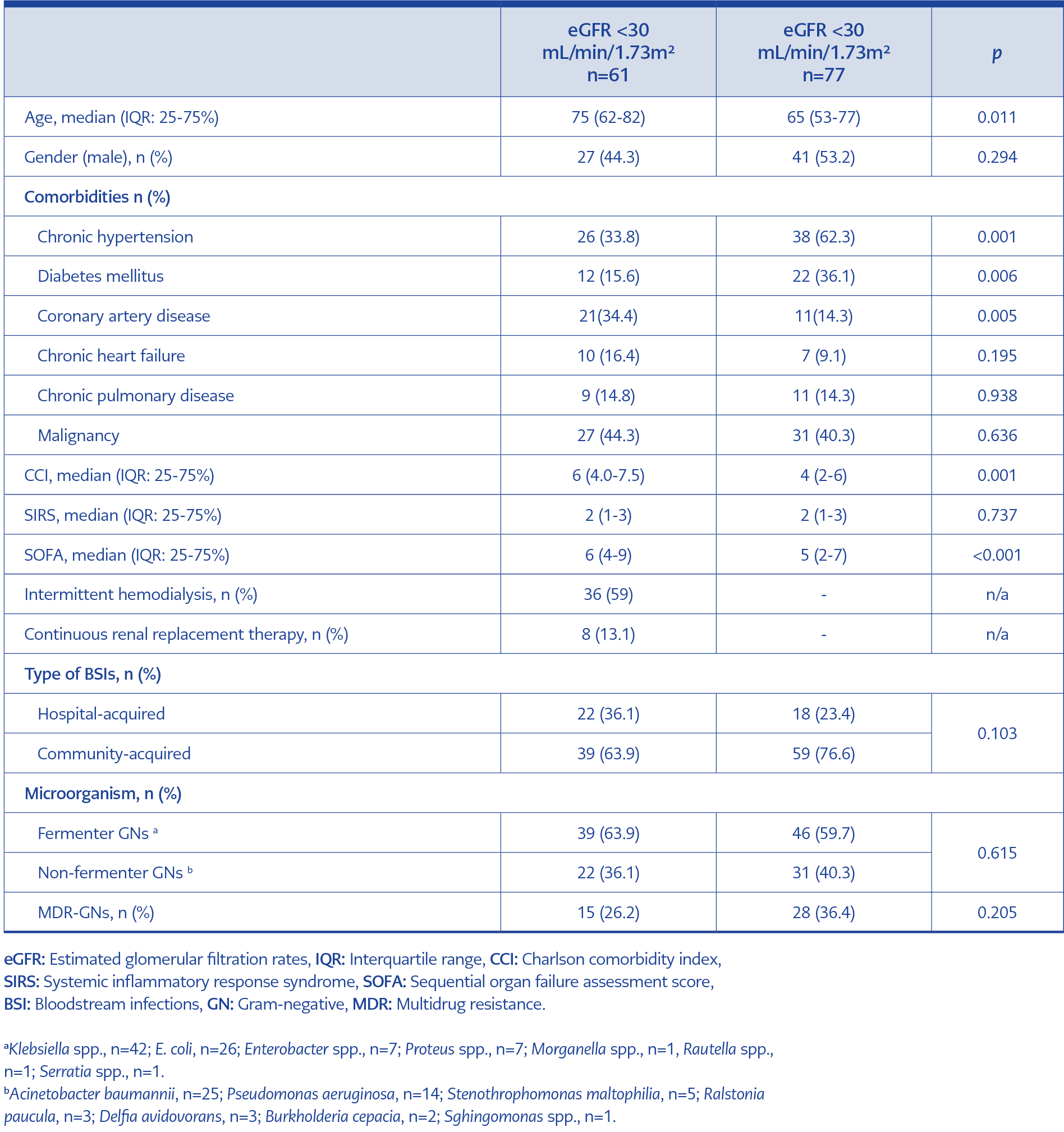
In the study, a total of 138 patients with eGFR <30 and ≥30 ml/min/ 1.73 m² were compared for their demographic and clinical characteristics (Table 1, Figure 1).
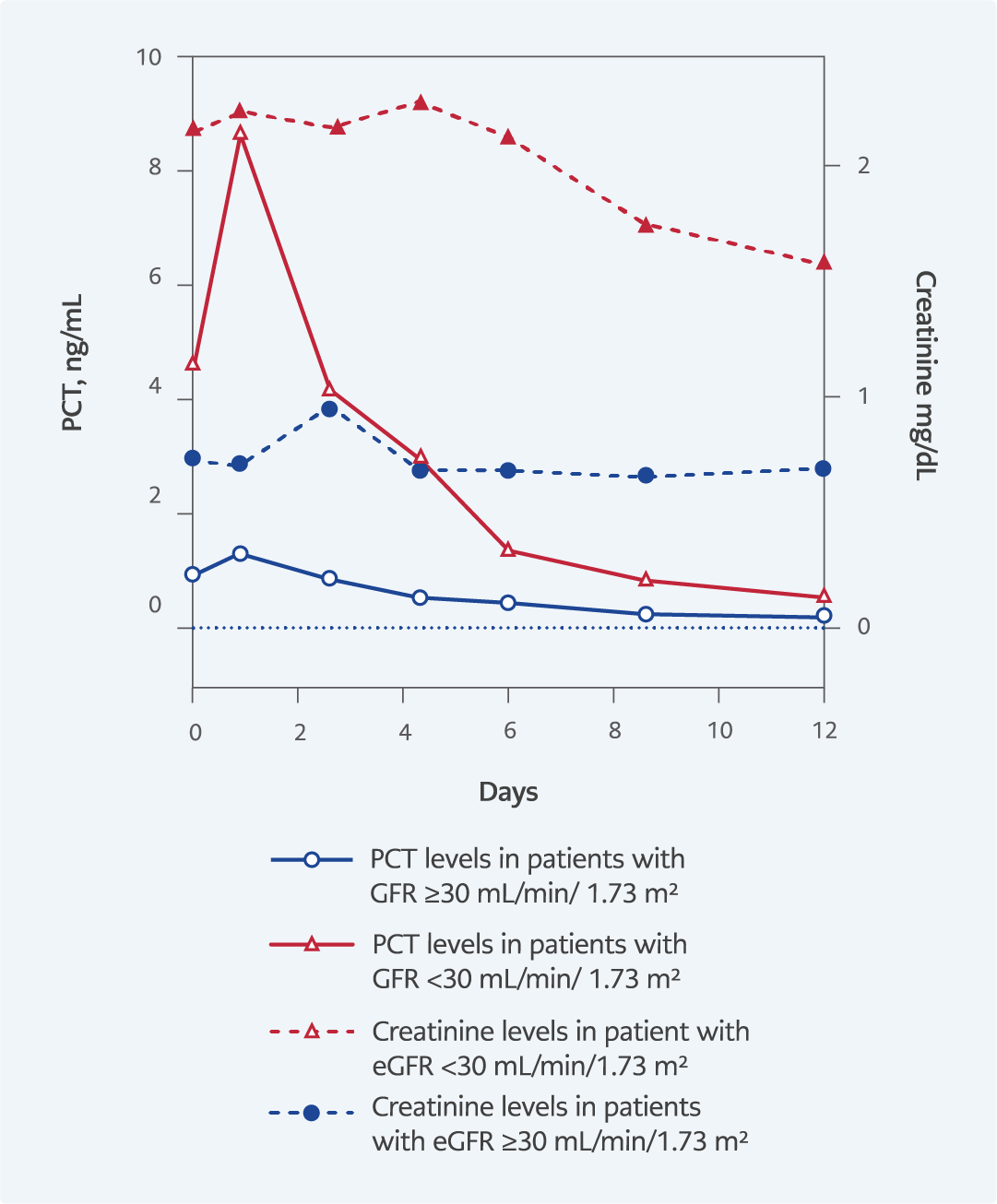
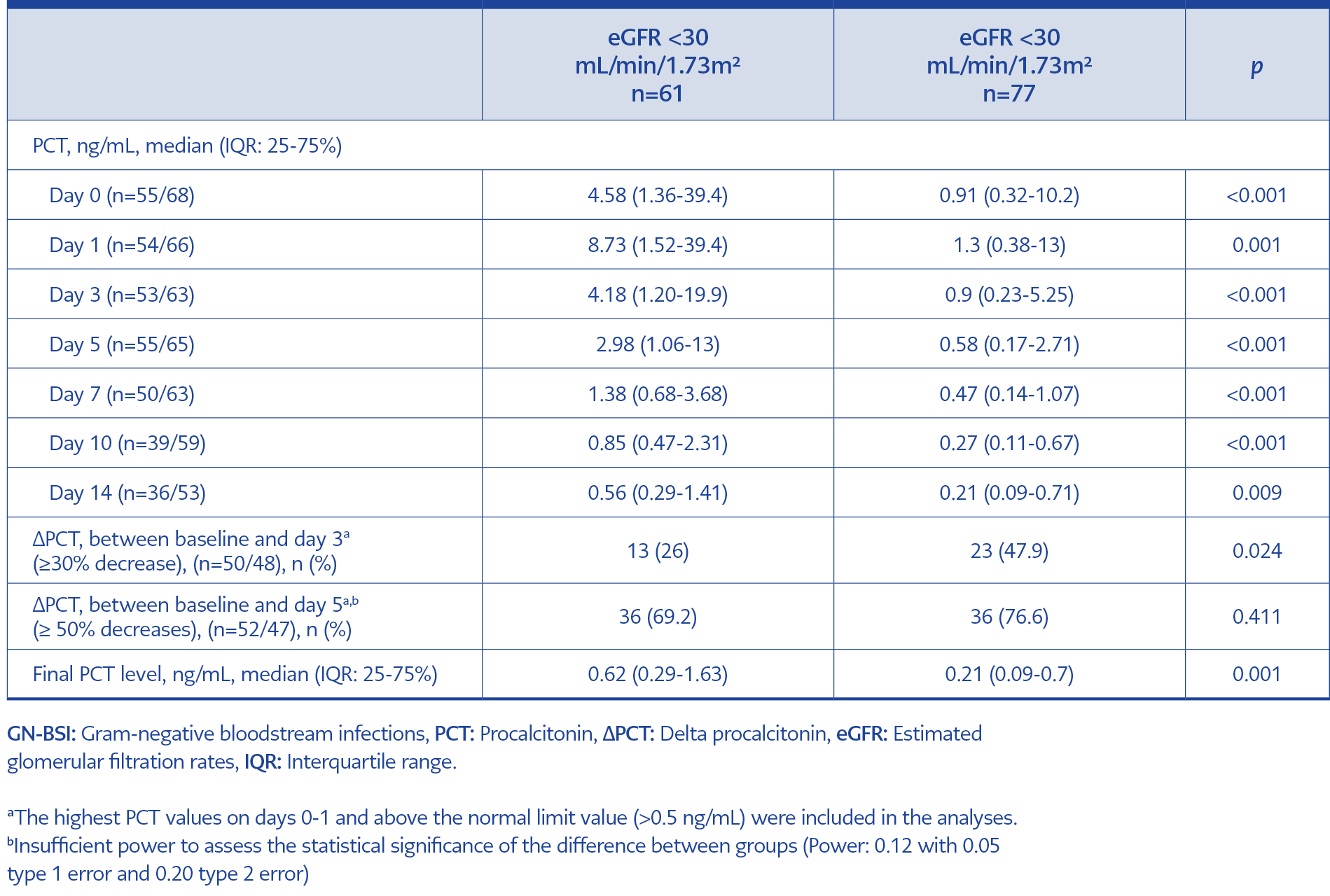
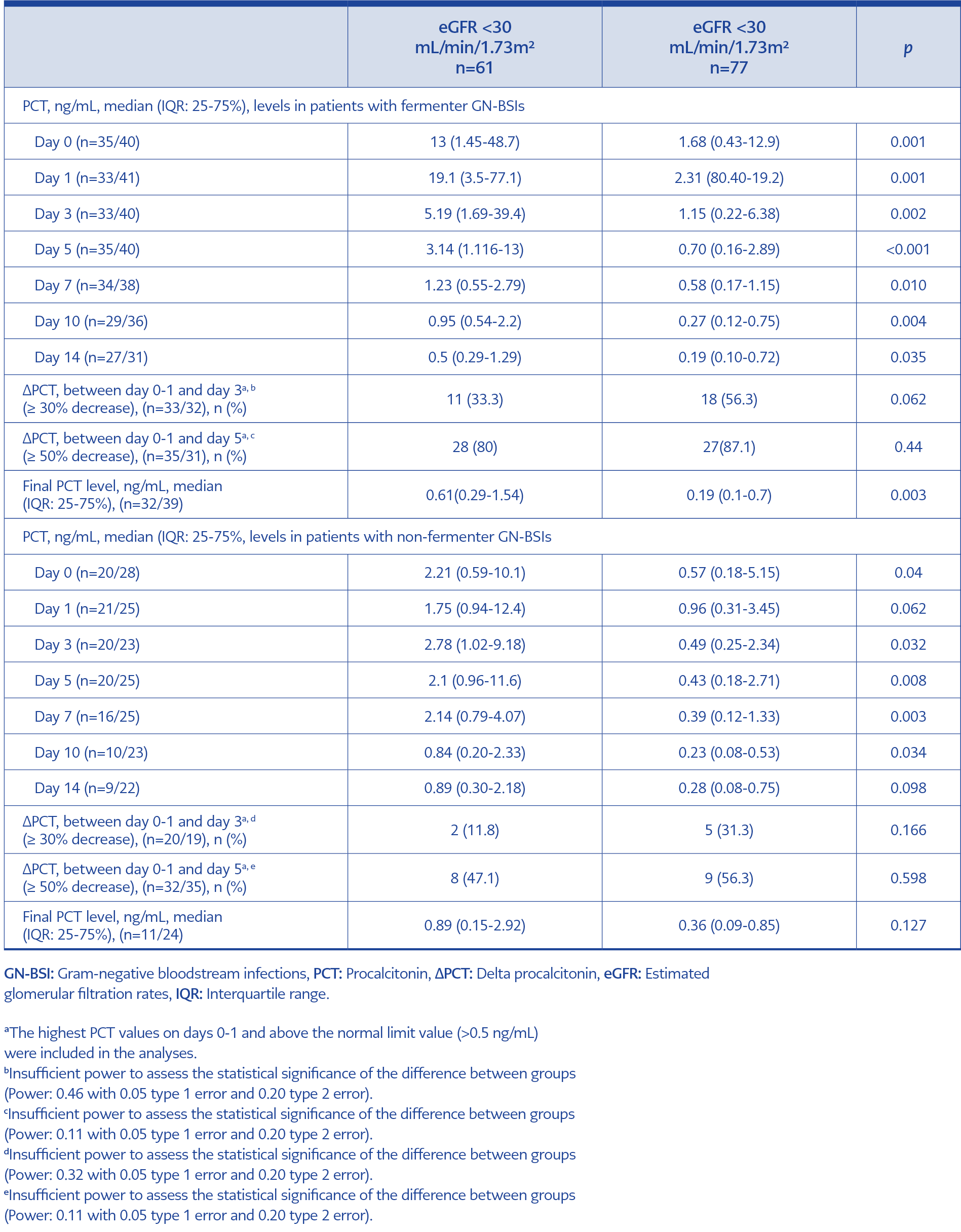
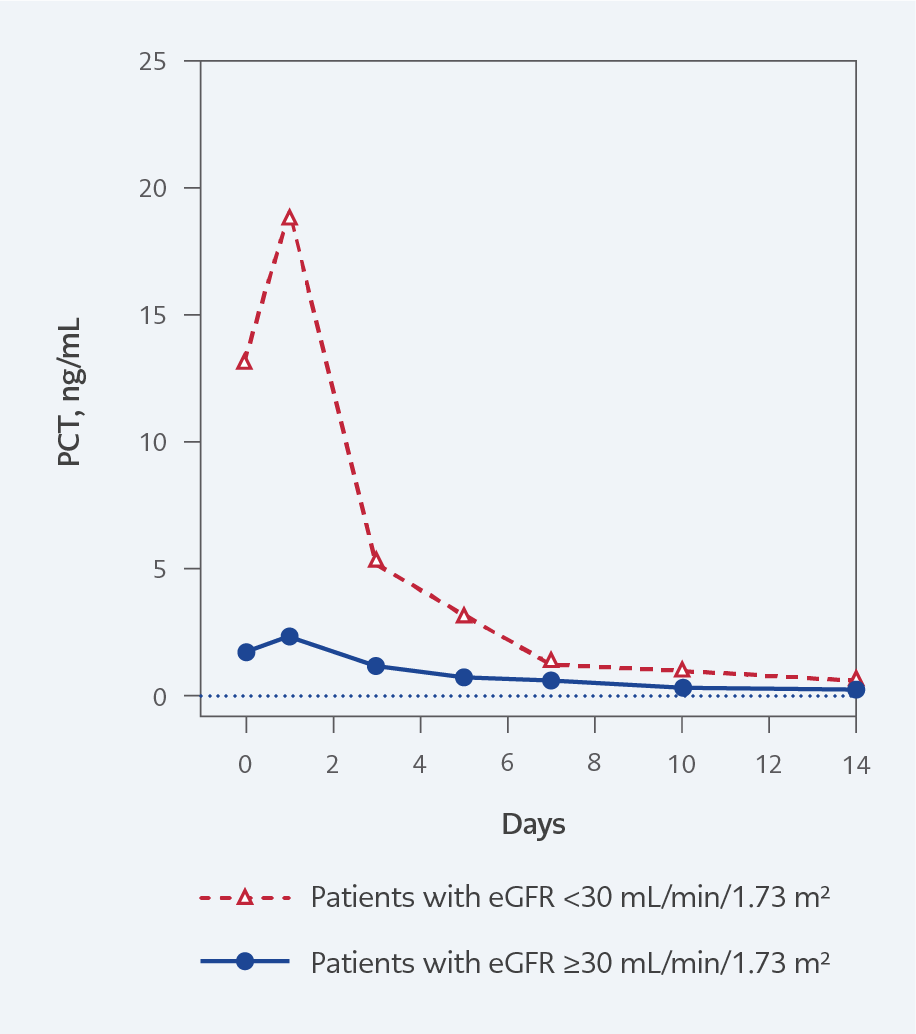
Of the patients, 71% (n=98) received empirical treatment, and 29% (n=40) received definitive appropriate antibiotic therapy. PCT levels on day zero of antibiotic therapy in patients with eGFR <30 mL/min/1.73m² and eGFR ≥30 mL/min/1.73m² were 4.58 (1.36-39.4) ng/mL and 0.91 (0.32-10.2) respectively (p<0.001). PCT level changes in both groups during therapy are presented in Figure 2 and Table 2.
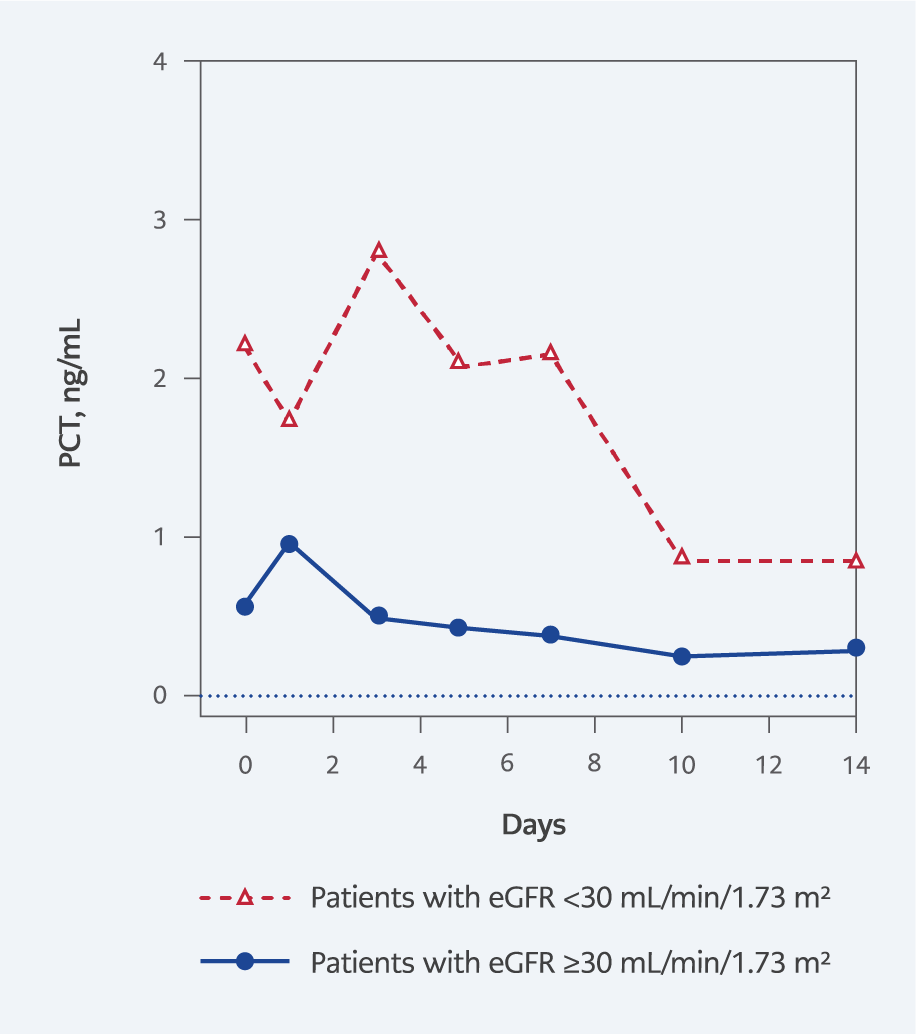
PCT levels on day zero of antibiotic therapy in BSIs with fermenter GNs were 1.68 (0.43-12.9) ng/mL in GFR ≥30 and 13.0 (1.45-48.7) ng/mL in GFR <30 (p=0.001). PCT levels on day zero of antibiotic therapy in BSIs with non-fermenter GNs were 0.57 (0.18-5.15) ng/mL in eGFR ≥30 and 2.21 (0.59-10.1) ng/mL in GFR <30 (p=0.040). Comparison of PCT levels during antibiotic therapy in patients with fermenter and non-fermenter GN-BSIs according to eGFR (<30 and ≥30 mL/min/1.73 m²) are presented in Table 3, Figure 3, and Figure 4.
Discussion
In our study, GN-BSIs-related PCT levels were higher at the beginning of antibiotic therapy in patients with low GFR levels. This significant difference in PCT levels associated with lower GFR levels persisted during antibiotic therapy. PCT elevation in patients with low GFR was higher in BSIs associated with fermenter GNs. On day three of antibiotic therapy, PCT response was inadequate in patients with low GFR levels. Due to the slow kinetics of PCT, most patients with low GFR had a PCT response by day five. Final PCT values in patients with low GFR levels were above normal serum PCT limits and higher than those with eGFR ≥ 30 mL/min/1.73m2.
The literature shows an inverse relationship between serum PCT and GFR levels (15). Compared with healthy controls, serum PCT values are higher and above the PCT normal limits in patients with renal failure without infection (10, 15). Also, in infected patients, the stage of renal failure directly affects serum PCT values (16). Therefore, higher PCT cut-off values are recommended to predict infection in patients with low GFR (9, 17, 18). As in diagnostic use, higher cut-off values are accepted for prognostic use of PCT in these patients (19). Decreased PCT clearance in renal failure is one of the possible causes of high serum PCT levels, but there is still no consensus on this hypothesis (10, 19). In their study, Meisner et al. found no relationship between serum PCT kinetic and age, gender, SOFA score, or GFR levels. So, they reported that renal secretion did not affect PCT elimination (20).
On the other hand, in some studies, PCT clearance decreased due to renal failure (9, 10, 18, 21). In our study, serum PCT level was significantly higher in patients with low eGFR in GN-BSIs during antibiotic treatment. This elevation may support the hypothesis that renal clearance of PCT is reduced due to renal failure. However, the low eGFR group had higher CCI and SOFA scores. This may cause differences in infection severity and immune response between groups, decreasing the causal relationship between renal clearance and high serum PCT levels. The possible increased severity of infection with renal failure confuses the relationship between PCT level and renal clearance (9). Therefore, in our study, we preferred to focus on PCT kinetics in patients with infection control rather than possible causes of PCT elevation.
Failure in PCT clearance is also a prognostic factor in critically ill patients (22-24). According to a study by Schuetz et al., 28th-day mortality was twofold high in patients without an 80% decline in PCT by day 4 (25). In other observational studies, an earlier 30-70% decrease in PCT values was associated with survival (12, 26). In a study by Giamarellos-Bourboulis et al., compared to baseline, a 30% decrease in PCT value on the second day, a 40% decrease on the fourth day, or detection of a normal PCT level (<0.5 ng/mL) on the fourth day was an early predictor of GNs-related bacteremia control (27). Kim et al. reported that the decrease in PCT levels on day three was associated with survival and renal recovery in patients with sepsis-induced acute renal failure. Every 10% decrease in PCT values was associated with a 10% decrease in mortality risk (11). Despite these studies, there is insufficient data for optimal cut-off and time interval for PCT decrease in patients with renal failure.
Our study showed that the PCT responses to antibiotic therapy in patients with infection control change according to eGFR levels. Patients with low eGFR had lower and slower PCT responses. eGFR directly affected PCT kinetics in both fermenter and non-fermenter GN bacteria-related BSI subgroups. This result is inconsistent with the study of Meisner et al., which suggested that the PCT serum clearance rate does not depend on renal function (20). According to our study result, the PCT response achieved in less than half of the patients on day three may lead to unnecessary PCT-based antibiotic therapy changes in patients with low eGFR. PCT response should be evaluated on the fifth day in patients with clinical responses to reduce unnecessary antibiotic revisions. However, in the fermenter BSI subgroup with a low eGFR level, the sharp PCT decrease on the third day may be helpful for an early response.
In clinical practice, serum PCT is generally used for optimal antibiotic therapy duration apart from its diagnostic and prognostic use. In their meta-analysis, Heilmann et al., PCT-guided antibiotic therapy in patients with renal failure resulted in an approximately two-day reduction in antibiotic use without increasing mortality risk. However, measurement times of PCT and PCT cut-offs for antibiotic therapy optimization were quite different in the studies included in the meta-analysis (28). This heterogeneity in the meta-analysis does not allow recommendations for clinical practice. In our study, final serum PCT levels at the end of antibiotic therapy were above normal limits in patients with low eGFR in the fermenter and non-fermenter GNs-related BSIs. In a PCT-guided antibiotic therapy approach, these high final PCT values may lead to unnecessarily longer antibiotic therapy. Therefore, in optimizing antibiotic therapy duration in patients with low eGFR, changes in PCT kinetics should be evaluated together with the resolution of clinical infection signs instead of the final PCT level.
Our study had some limitations. First of all, despite the strict inclusion criteria, all confounding factors that may affect PCT kinetics could not be excluded due to the retrospective study design. Although we determined some criteria to exclude other active infections that may affect PCT kinetics, these infections may not have been wholly excluded. Our study used the CKD-EPI 2009 formula to calculate eGFR and did not measure actual GFR (29). All eGFR formulas known to us are validated in stable patients without acute kidney injury (AKI), and they tend to overestimate eGFR when AKI is present. To tackle this issue, some researchers suggest using newer indicators of AKI such as kidney injury molecule-1 (KIM-1), neutrophil gelatinase-associated lipocalin (NGAL) and others, but their success and triumph over eGFR is not well established (30, 31). Furthermore, measuring the actual GFR is a cumbersome process which can only be employed in studies with a prospective design and intent (32). However, to minimize the effect of eGFR’s well-known constraints on our work, we demonstrated creatinine trends, which are more valuable than a single estimate of kidney function (33). Another limitation related to the retrospective and descriptive study design is missing data in PCT serial measurements. This may cause the sample size to change in each comparison and increase the risk of type 2 errors. Another limitation of our study is that since PCT values were not normally distributed, pairwise comparisons could be made at the measurement points instead of mixed ANOVA between the study groups.
In conclusion, according to our study results, serum PCT levels were higher in patients with low eGFR at baseline, during, and at the end of therapy. Early PCT response evaluation should not be performed, especially in these patients with non-fermenter GN-BSIs, as the PCT response is delayed until the fifth day. Considering high PCT levels and slower PCT kinetics in patients with low eGFR may reduce unnecessary antibiotic revisions and extensions.