Introduction
COVID-19 is caused by SARS-CoV-2 from the Coronaviridae family, Orthocoronaviridae sub family, Betacoronavirus genus, and Sarbecovirus subfamily (1). Cytokines and chemokines have been essential in the immune response against coronaviruses (2). First reports investigating clinical features of COVID-19 showed that serum levels of interleukin (IL)-2, IL-7, IL-10, granulocyte colony-stimulating factor (GSCF), IP10 (CXCL10), monocyte chemoattractant protein (MCP-1/CCL2), macrophage inflammatory protein (MIP) 1α, and tumor necrosis factor (TNF) α were higher in intensive care unit (ICU) patients (3). Subsequent reports confirmed the changes in serum levels of cytokines in COVID-19 patients compared with healthy individuals (4). Considering the role of cytokine storm in COVID-19 pathogenesis, some of the cytokines might be potential predictive markers for disease severity (5). However, longitudinal analyses of serum cytokine levels rarely focused on the first few days after symptom onset, and sample sizes varied from seven patients to 143 patients (6-8). A recent study showed that severity is associated with persistent viral levels, reduced cytotoxic natural killer cells, and increased inflammation (9).
In this study, we aimed to investigate the role of cytokines in predicting disease severity when measured in the first five days after symptom onset. Longitudinal sera collection was performed on COVID-19 patients to demonstrate temporal characteristics of serum cytokines and chemokines and to compare predictive performances for COVID-19 severity.
Materials and Methods
Control participants and hospitalized COVID-19 patients were recruited to the study voluntarily between March 1 and May 30, 2020. Patients were classified according to the World Health Organization (WHO) severity classification. Longitudinal serum samples of COVID-19 patients were collected until the 24th day after the onset of symptoms. Demographic characteristics, past medical history, and routine laboratory values regarding the first 24 days after the onset of symptoms were collected for COVID-19 patients who participated in the study. One-time serum samples were collected from the control group.
For assessing serum cytokine levels, the LEGENDplexTM Multi-Analyte Flow Assay Kit Human Inflammation Panel 1 (BioLegend, USA) was used. Serum levels of 13 cytokines including IL-1β, interferon (IFN) α2, IFN-γ, TNF-α, MCP-1 (CCL2), IL-6, IL-8 (CXCL8), IL-10, IL-12p70, IL-17A, IL-18, IL-23, and IL-33 were tested from the collected sera.
This study was approved by the Institutional Review Board, and informed consent was obtained from all patients in accordance with relevant guidelines and regulations.
Statistical Analysis
The statistical analyses were performed using Stata (StataCorp, USA) and the Statistical Package for Social Sciences (SPSS) 21.0 (IBM Corp., Armonk, NY, USA). The chi-square and Fisher exact tests were used to compare demographic and comorbidity differences. For the comparison of serum cytokine levels and routine laboratory values, the Kruskal-Wallis H test was used, and ad hoc analyses were performed by the Mann-Whitney U Test. Statistical significance was considered when the p-value was less than 0.05.
Results
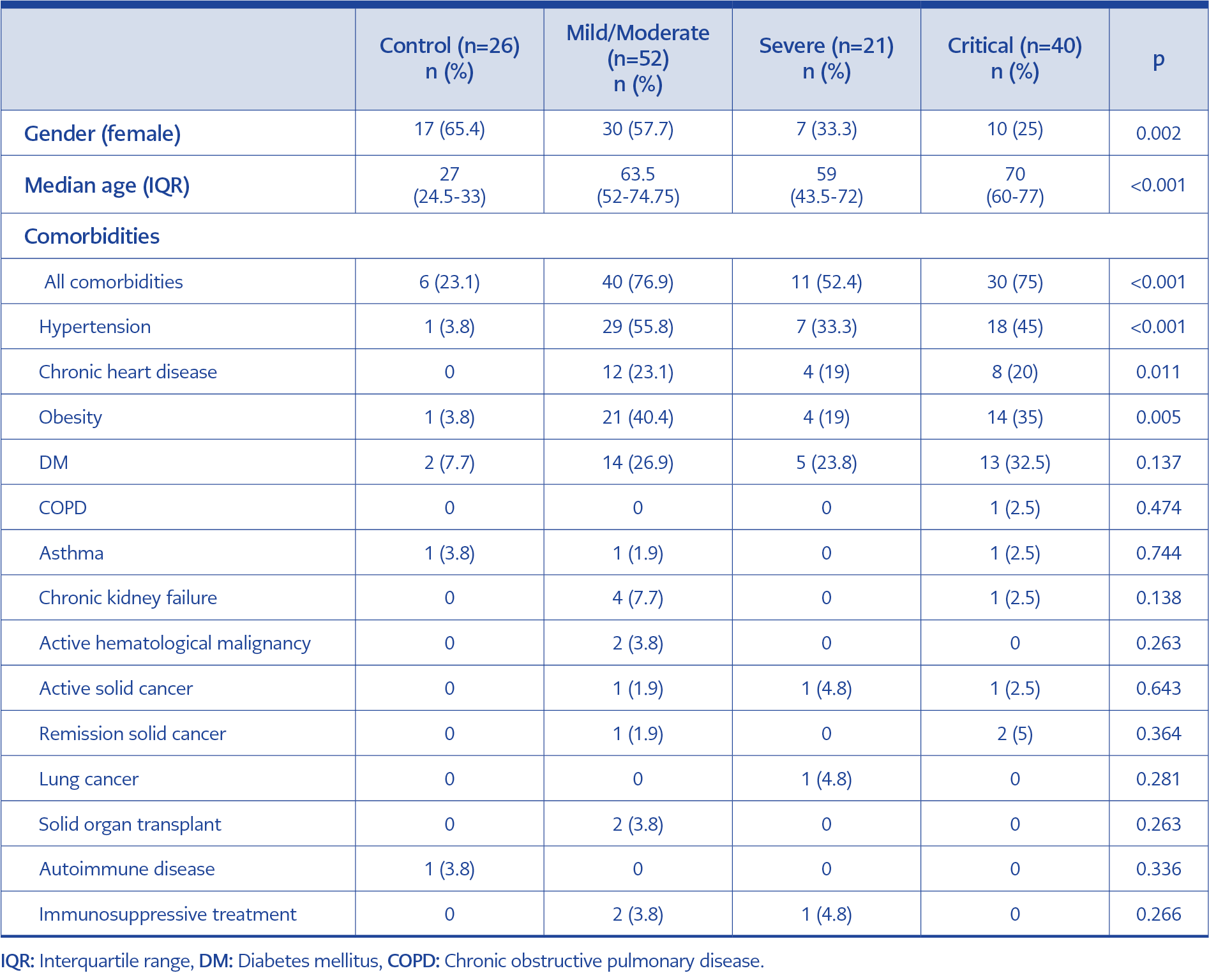
A total of 238 serum samples from 113 patients and 26 controls were studied for their serum cytokine levels. Among 113 patients, 52 had mild/moderate disease, while 21 had severe and 40 had critical COVID-19. ICU admission was required for 31 of the critical patients, and mortality was observed in nine patients. Demographic and clinical characteristics are demonstrated in Table 1. Male gender and advanced age were risk factors for developing more severe disease. The prevalence of hypertension, chronic heart disease and obesity was lower in the healthy control group, control participants had fewer comorbidities overall.
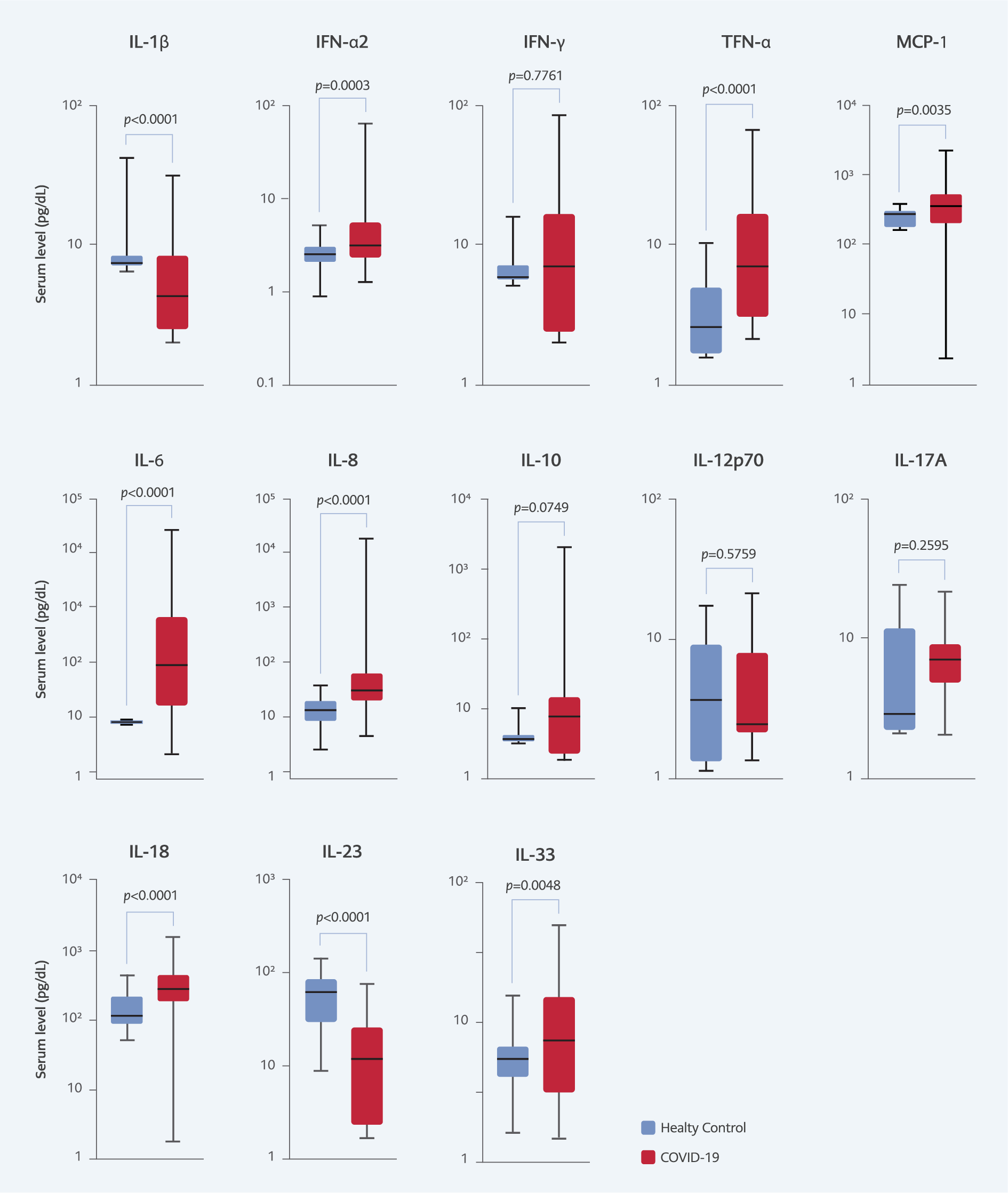
Among all tested cytokines, serum levels of IFN-α2, TNF-α, MCP-1 (CCL2), IL-6, IL-8, IL-18, IL-33 were elevated in COVID-19 patients compared with healthy participants (Figure 1). However, serum levels of IL-1β and IL-23 were found to be lower in the patient group compared with controls (p<0.0001). No statistically significant change was observed for serum levels of TNF-γ, IL-10, IL-12p70, and IL-17A when COVID-19 patients were compared to healthy controls (Supplementary Figure 6, 7, 9, 10).
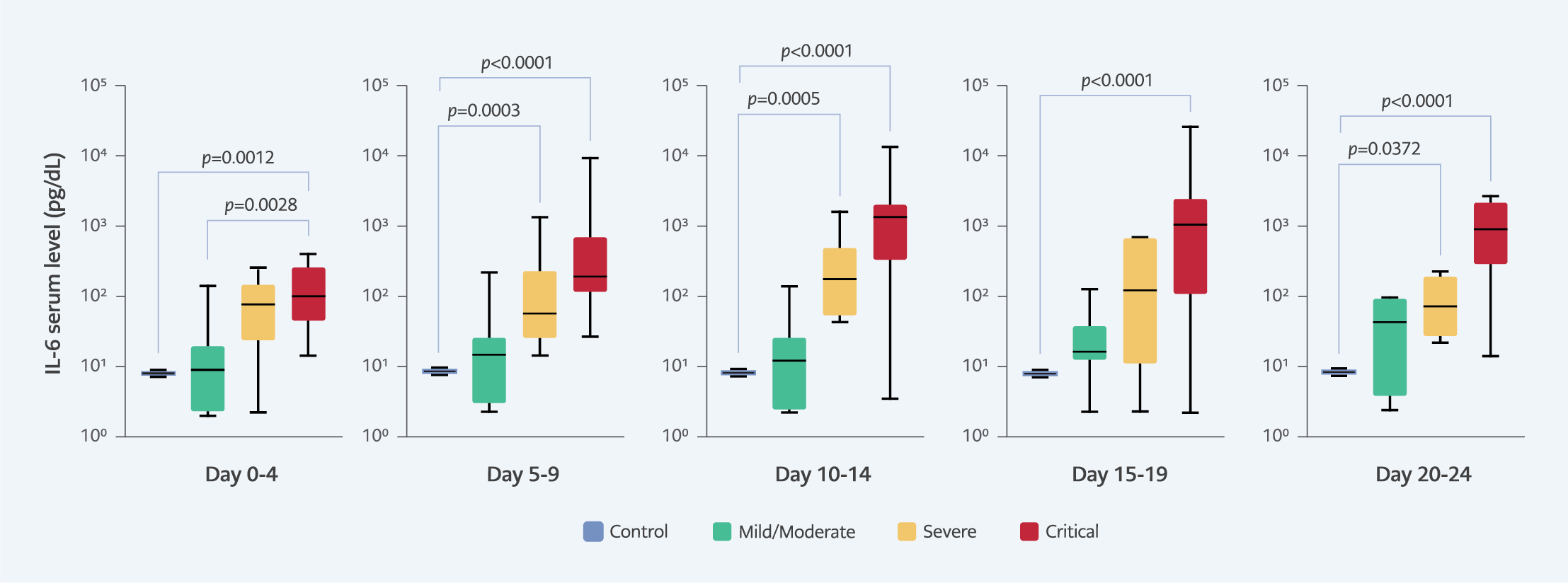
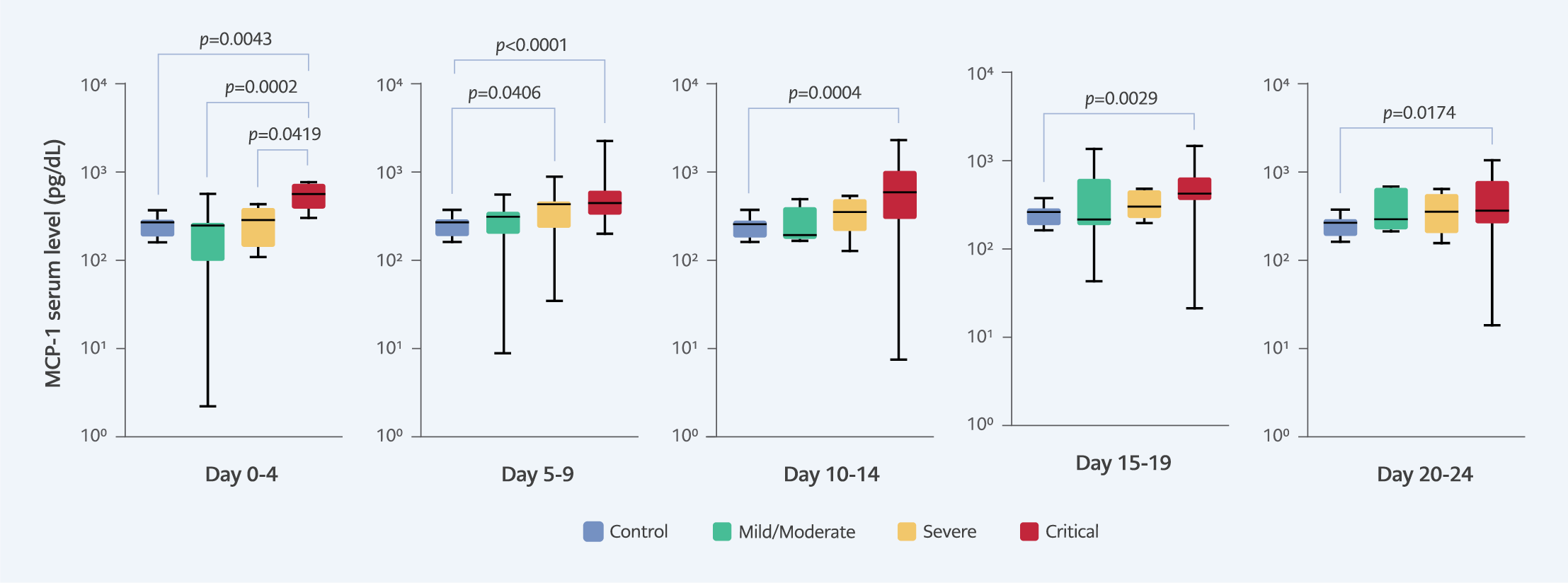
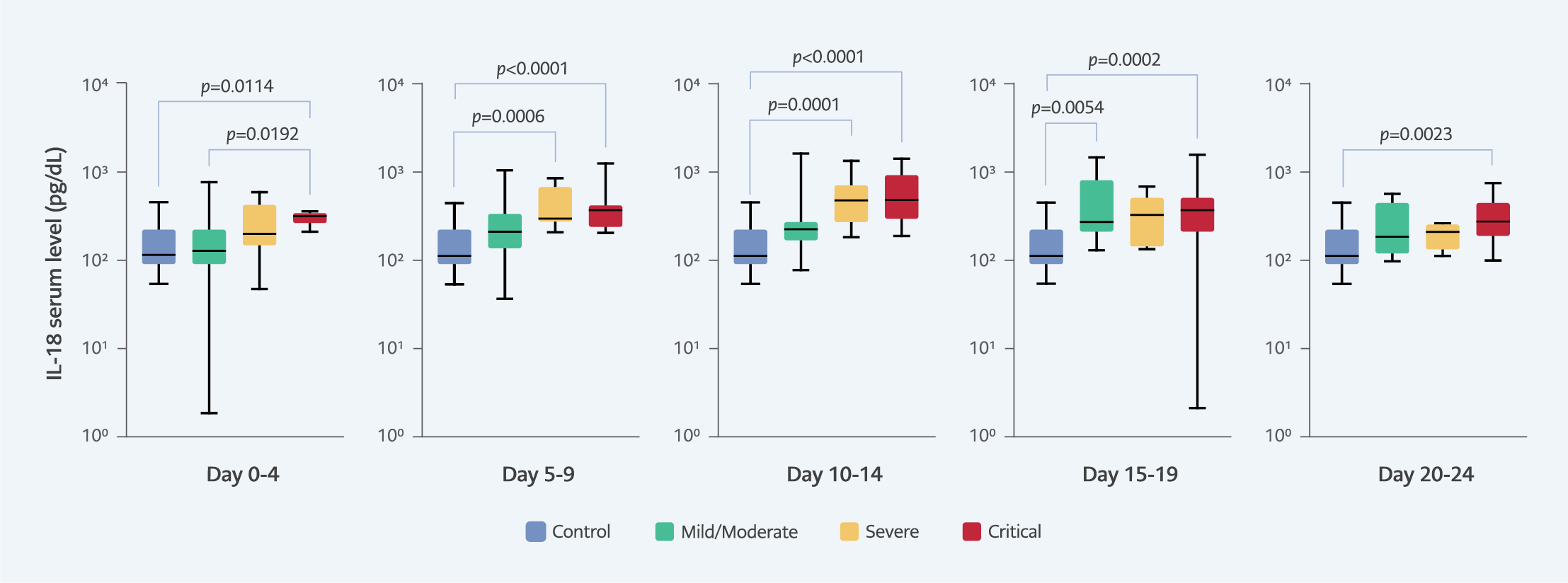
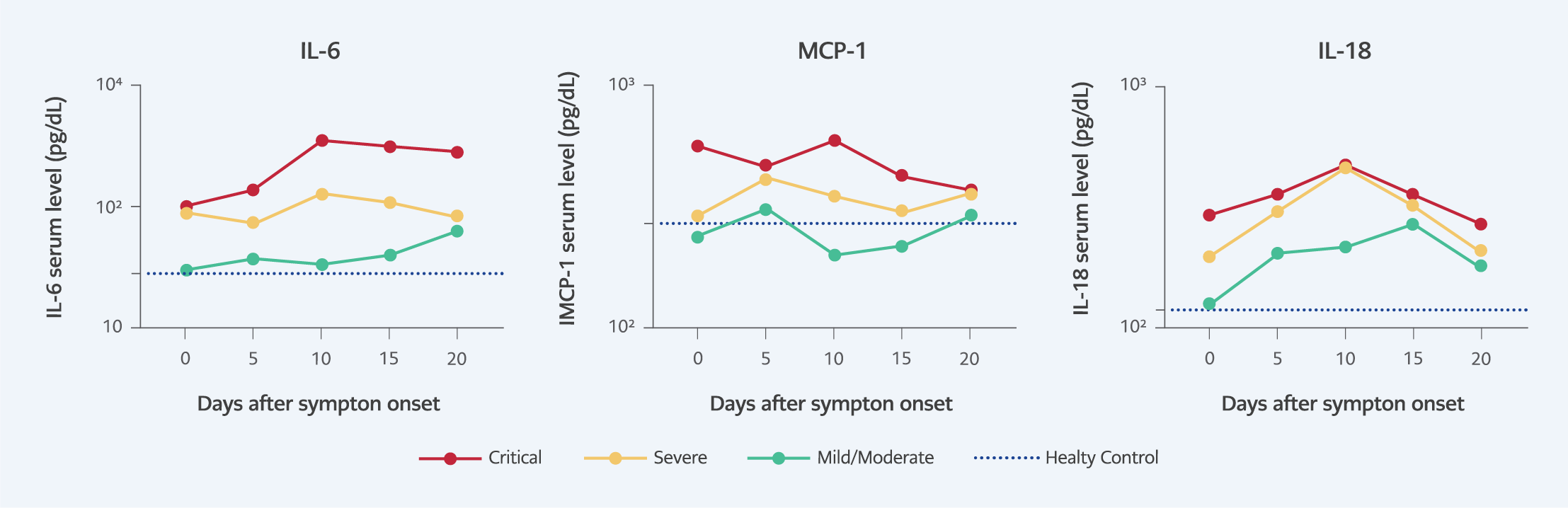
During the first five days after symptom onset (days 0-4), the serum cytokine levels of IL-6, MCP-1 (CCL2), and IL-18 were elevated in critical patients compared to the mild/moderate disease severity group (Figure 2-4). Additionally, serum MCP-1 (CCL2) levels were elevated in critical patients compared to the severe disease severity group. In the longitudinal analysis, median serum levels of these three cytokines were always the highest in the critical group (Figure 5). Similarly, median serum levels in the severe group were higher than the mild/moderate severity group during the 24-day follow-up period (Figure 5).
However, the pattern of serum cytokine levels differs among different cytokines and disease severities. In the critical severity group, the highest median cytokine levels for IL-6, MCP-1 (CCL2), and IL-18 were on days 10-14 after symptom onset (Figure 5). For IL-18 serum levels, critical and severe patient groups had increasing cytokine levels that peaked on days 10-14 and had a decreasing trend afterwards until the end of follow-up (Figure 5).
Although serum levels of IL-8 and IL-23 were not able to differentiate disease severity statistically, serum levels of IL-8 were higher in critical patients (Supplementary Figure 1). In contrast, serum levels of IL-23 were lower in critical (Supplementary Figure 2) compared to healthy controls. Between days 5-19, TNF-α serum levels were higher in all disease groups compared to controls (Supplementary Figure 3). Similarly, IFN-α2 serum levels were elevated in all severity groups compared to controls on days 5-9 (Supplementary Figure 4). However, the increased serum IFN-α2 levels were sustained until days 15-19 only in the mild/moderate patient group. No increase was observed in IL-1 β serum levels of COVID-19 patients (Supplementary Figure 5). However, lower IL-1β serum levels were observed in the mild/moderate COVID-19 severity group, compared to healthy individuals, between the fifth and twelfth days after symptom onset. Elevated IFN-γ serum levels were observed in the mild/moderate patient group compared to healthy controls only between days 15-19 (Supplementary Figure 6). Interestingly, IL-10 serum levels were elevated in the severe and critical patient groups compared to control participants between days 5-9 (Supplementary Figure 7). Moreover, serum levels of IL-33 were higher in critical patients compared to healthy controls between days 15-24 (Supplementary Figure 8). Longitudinal analysis of IL-12p70 and IL-17A serum levels yielded no statistically significant difference between COVID-19 severity groups and healthy controls.
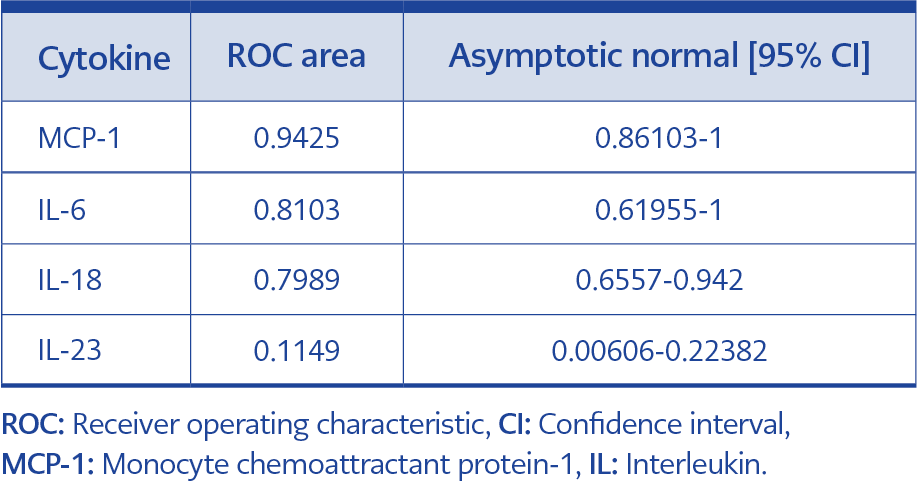
Table 2. Non-parametric ROC analyses of MCP-1, IL6, IL18, and IL23 for prediction of critical disease.
Receiver operating characteristic (ROC) analyses were performed on MCP-1, IL-6, IL-18, and IL-23 to assess predictive performance for critical disease severity prediction in the first five days after symptom onset (Table 2). MCP-1 showed the best performance, followed by IL-6 and IL-18. Decreased serum levels of IL-23 early in the disease course were associated with decreased COVID-19 severity. The area under the receiver operating curve (AUC) was 94% for MCP-1, 81% for IL-6, 79% for IL-18, and 11% for IL-23.
The severity prediction power of routine laboratory investigations was performed for procalcitonin, C-reactive protein (CRP), leucocyte count, neutrophil count, lymphocyte count, platelet count, hemoglobin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), lactate dehydrogenase (LDH), creatinine, D-dimer, international normalized ratio (INR), ferritin, triglyceride, fibrinogen, and troponin (Supplementary Figure 11-23). In the first five days after symptom onset, elevated CRP and decreased lymphocyte count were observed in the critical disease group compared to mild/moderate patients (Supplementary Figure 12, Supplementary Figure 14). Decreased lymphocyte count and elevated CRP levels persisted until day 14 in the more severe disease groups. Liver enzymes ALT, AST, and LDH serum levels were increased in the severe and critical disease groups compared to the mild/moderate disease group, especially between days 5-14 after symptom onset (Supplementary Figure 18-20). CRP and ferritin serum levels were higher in the severe and critical disease groups compared to mild/moderate disease groups between days 0-14 after symptom onset (Supplementary Figure 12, Supplementary Figure 23).
Discussion
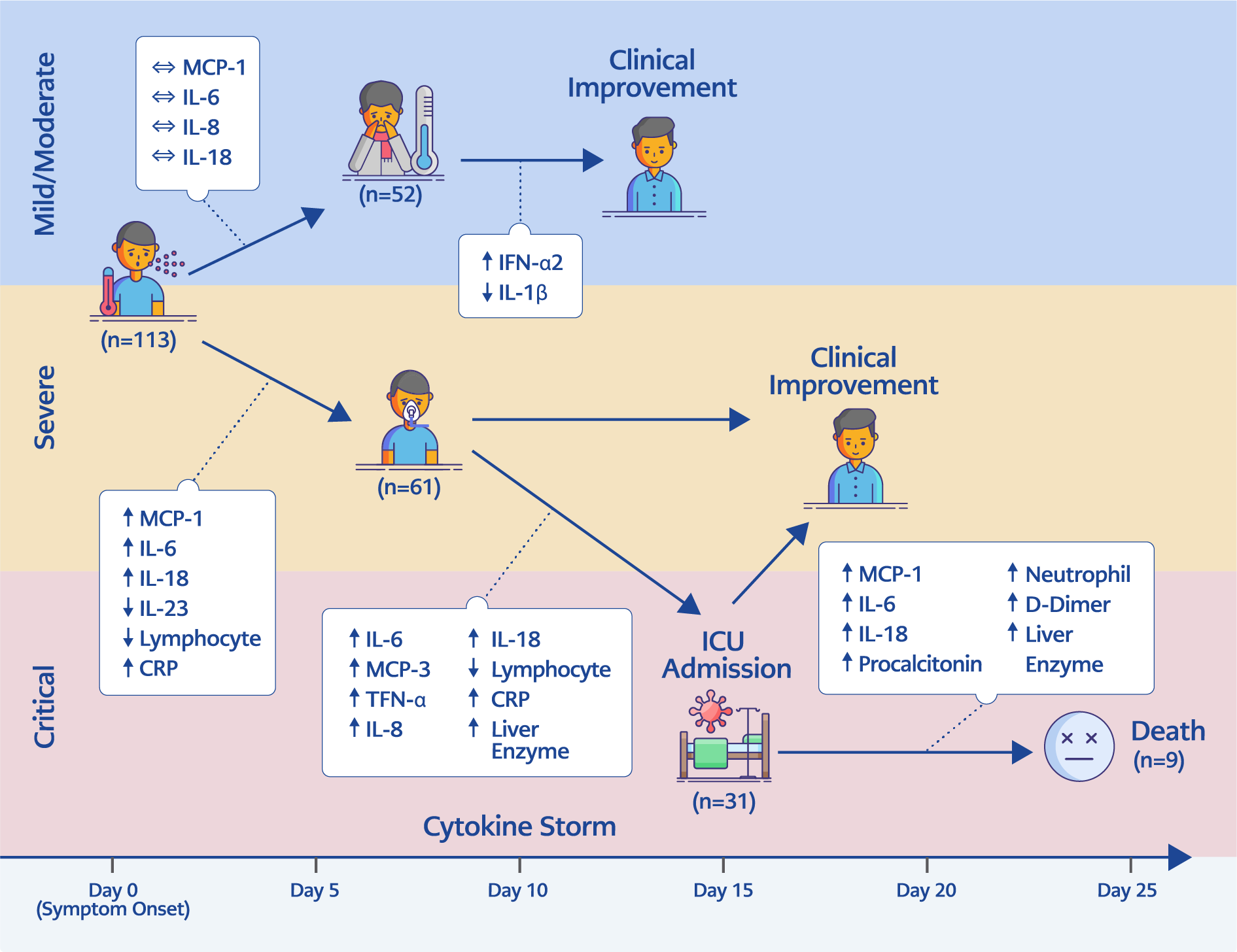
Figure 6. Proposed cytokine profiles during the milder and more severe disease course for 24 days after symptom onset.
We presented the clinical role of cytokines in COVID-19 and their early predictive potential for disease severity. In our study, we observed that serum levels of IFN-α2, TNF-α, MCP-1, IL-6, IL-8, IL-18, and IL-33 were increased in COVID-19 patients compared to healthy controls. In the first five days after symptom onset, increased IL-6, IL-18, and MCP-1 serum levels but decreased IL-23 serum levels are demonstrated in the critical disease group through the longitudinal analysis of serum cytokines levels (Figure 6). Likewise, IL-8 and TNF-α serum levels increased after the fifth day onwards.
IL-6, TNF- α, IL-1β, and IL-18 have been investigated as classically known pro-inflammatory cytokines. In the lungs of COVID-19 patients, higher immunoreactivity was observed for IL-1β, IL-6, MCP-1, and TNF- α (10). Similarly, clinical and in vitro studies have also reported elevated IL-1β levels (11, 12). We detected the early increase of serum IL-6 and IL-18 levels in severe and critical COVID-19 patients and relatively later increase in TNF-α serum levels in the patient groups on the fifth day after symptom onset. Although we observed increased levels of IL-6, TNF- α, and IL-18, we failed to detect IL-1β increase in any patient group. Elevation of IL-18 without IL-1β was also observed in other studies (13). On the contrary, IL-6 was found to be consistently elevated in the disease groups compared to controls, as well as in more severe patients compared to patients with mild COVID-19. Continuously high IL-6 levels for 24 days in the critical patient group in this study are suggestive of the clinical value of IL-6 inhibitors. Therefore, we hypothesize that IL-1β inhibiting drugs such as anakinra, rather than IL-6 inhibitors, might be reserved for smaller patient groups and used by monitoring the inflammatory markers.
MCP-1 (CCL2) and IL-8 (CXCL8) are responsible for leukocyte recruitment, later being more specific for neutrophils. We detected the early increase of MCP-1 in the critical patient group compared to control and other disease severity groups. Elevated MCP-1 levels were sustained during the 24-day follow-up period. However, IL-8 serum levels were elevated after the fifth day of symptoms in the severe and critical patient groups compared to control patients. Increased gene expression of MCP-1 was shown in monocyte-derived macrophages (12) and COVID-19 patients’ bronchoalveolar lavage fluid (14). MCP-1 is secreted in higher concentrations by the airway epithelium after SARS-CoV-2 infection (15). Other studies showed that MCP-1 was significantly higher in COVID-19 patients compared to healthy controls (4) and predictive of mechanical ventilation duration among COVID-19 patients (16). In a longitudinal study, MCP-1 was associated with mortality, although serum levels were increased on the sixth day of admission (17), later in the disease course compared to our observations.
IL-23, secreted by local macrophages and dendritic cells (DCs), has been known in autoimmune diseases because it maintains IL-17-producing T cells, suppresses Treg function, and causes chronic inflammation (18). Surprisingly, we observed early IL-23 suppression in critical COVID-19 patients compared to patients with milder disease. Our findings contradict the studies that report higher IL-23 serum levels in severe COVID-19 cases compared with mild/moderate disease (19). However, decreased levels of IL-17A have also been reported to be associated with mortality together with elevated levels of IL-10, IL-8, IL-6, and TNF-α (20). Therefore, either the pathogenic or the protective nature of IL-23-IL-17 immune pathway is controversial.
Elevated CRP levels and decreased lymphocyte count were the only two parameters that are predictive laboratory parameters for disease severity. In the first 24 hours of admission, CRP, neutrophil count, urea, creatinine, and troponin elevations were shown in the literature (11). However, the admission date, at the beginning of the infection, can impose a bias as symptoms might have started days before the hospital admission. We showed a persistent elevation of the liver enzymes and ferritin in the severe and critical disease groups starting with the fifth day after symptom onset and elevation of D-dimer after the 10th day in the critical group compared to the mild/moderate severity group. These time-dependent changes might be critical in predicting the prognosis.
Our study has some limitations. A total of 139 participants is the most limiting factor for this study as the predictive value of some of the cytokines might be masked due to interpersonal variations since consideration of the clinical context and data validation are the recommended strategies for interpreting cytokine measurements (21). Additionally, control group in the study had less comorbidities and lower median age which are the factors may be associated to over-representing the role of some cytokines such as IL-6. Besides, the number of patients distributed into disease severity groups was unequal. Although each of the mild/moderate and critical groups had at least 40 participants, the severe patient group had only 21 patients, which might have affected our ability to show statistical differences between severe and critical disease groups.
Serum cytokine levels can be used for the prediction of severity and follow-up for the prognosis of COVID-19 patients. IL-6 was always predictive of disease severity in the 24 days of the study period. MCP-1 and IL-18 showed the best predictive value in the first five days after the symptom onset. On the other hand, IL-8 and TNF- α were better predictors of severe disease from the fifth day onwards after symptom onset.
In conclusion, our findings support the rational usage of IL-6 inhibitors for the treatment of severe or critical patients; however, IL-1 inhibitors should be reserved before randomized controlled studies show their effectiveness. Early measurements of MCP-1, IL-6, and IL-18 serum levels might have clinical significance for severity prediction. Furthermore, IL-6, MCP-1, and IL-18 could also be used to predict disease progress.