Introduction
The novel coronavirus (SARS-CoV-2) started in December 2019 in China, has infected over 4.2 million people worldwide, resulting in a death toll of 290 000 as of 13 May 2020 (1). It causes a multi-systemic infection named Coronavirus Disease 2019 (COVID-19) (2). The symptoms reported are non-specific and usually comprise fever, cough, dyspnea, and fatigue (3). The virus predominantly attacks the respiratory system, rendering some of the patients with respiratory distress (4). Even though some treatment guidelines exist and many randomized controlled trials are being conducted, no consensus on effective treatment modalities exists (5).
With a population of nearly 85 million people, Turkey is the 17th most populated country in the World. The Ministry of Health has been working to control the disease since the first confirmed case was declared in the country on 11 March 2020 (6, 7). A preliminary national COVID-19 guideline was released on 24 January, and it has been updated regularly according to emerging evidence. (8) As of May 5, Turkey ranks nineth among the countries in the world in terms of total cases. (9)
Istanbul, with its 15 million inhabitants, emerged as an epicentre for the COVID-19 pandemic. (10) Over 60% of the COVID-19 cases in Turkey were situated in İstanbul. (11) The risk of disease transmission is high, being the most populated city in Europe and hosting nearly 200,000 domestic and international passengers daily. (12)
New local outbreaks are expected in the course of the pandemic, and thus, COVID-19 will continue to be a threat to the healthcare system. Matching with the clinical evidence, the bottleneck of managing this disease is the Intensive Care Units (ICU) capacity. One of the major determining factors on mortality for critically ill patients is the availability of the ICUs. (13) Therefore, a strategic approach is necessary to help identify patients on their first admission who will most likely be in an ICU.
In this observational study, our objective was to describe demographic and clinical characteristics and outcomes of patients hospitalised with COVID-19 in a tertiary hospital in Istanbul. We compared patients who required ICU admission with those who did not require it and intended to inform clinicians and hospitals about the need for ICU admission among hospitalised patients.
Materials and Methods
Study design
We performed a retrospective cross-sectional study at a large tertiary hospital in İstanbul. The hospital is designated as a pandemic centre throughout the COVID-19 outbreak, accepting all patients and serving free-of-charge as per the Turkish Ministry of Health regulations using the national COVID-19 treatment algorithm.
The hospital capacity and COVID-19 adjustments
The hospital serves around 20 000 patients per month with 50 ICU and 200 inpatient beds. Following the first confirmed COVID-19 case in Turkey on 11 March 2020, all attending staff were alerted and a 24-bed isolation ward for suspected and confirmed COVID-19 cases and 25 ICU beds with droplet and contact isolations were prepared. Another 24 beds were made available for the isolation ward afterwards. Against full ICU bed occupancy, 9 beds in the cardiac intensive care unit were also prepared. At the peak point of the COVID-19 outbreak, 48 beds in the wards and 25 beds in ICU were fully occupied. The hospital has not reached 100% occupancy throughout the pandemic period and all patients requiring any level of care were taken care of.
Participants
We enrolled all adult patients who fulfilled confirmed or suspect COVID-19 case criteria according to the Ministry of Health Guidelines admitted to our hospital between 9 March 2020 and 30 April 2020.
Data collection
Data were collected from the electronic health record system of the hospital and the national COVID-19 surveillance system. During the COVID-19 outbreak, the national system was used in real-time for daily data collection of suspected or confirmed cases and contact tracing by the Ministry of Health.
Data included patients’ sex, age, current smoking status, body mass index (BMI), comorbidities, presenting clinical signs and symptoms, initial laboratory tests, assessments of chest computed tomography (CT), final outcome (length of stay, discharge, mortality), prognoses on day 5, 10, 14, 21, and test result of real-time reverse transcription (RT)-polymerase chain reaction (PCR) from nasopharyngeal specimens.
Presenting clinical and laboratory parameters included temperature, respiratory rate, oxygen saturation, and heart rate; comorbidities included hypertension, diabetes mellitus, cardiovascular disease, chronic obstructive pulmonary disease (COPD), and asthma. Initial laboratory tests comprised complete blood count, C-reactive protein (CRP), ferritin, lactate dehydrogenase (LDH), d-dimer, interleukin-6, and CD4/8. Chest CT scan was defined as positive if the radiologist marked any sign of COVID-19 based on the existence of features consistent with pneumonia such as ground-glass opacities, consolidation, interlobular septal thickening. PCR test was regarded as positive if the patient had at least one positive result on consecutive tests.
The main outcome measures were the following: COVID-19 ward or ICU hospitalisation, the requirement of invasive mechanical ventilation, discharge or death. Mortality data were quite low (4.4%), therefore not used as an endpoint in the analysis, but presented separately. A numeric scale ranging from 1 to 4 was developed to assess prognosis as follows: discharged, COVID-19 ward stay, ICU admission, ICU admission plus intubation.
The clinical outcome was evaluated on days 5, 10, 14, and 21 of the hospitalisation. The selection of these dates was based on the 5-day and 10-day regimens of treatment protocols and 14- and 21-days follow-up days recommended by the Turkish Ministry of Health COVID-19 treatment guideline. As of April 30, 2020, 26 patients were still hospitalised (12% of the cases).
Statistical Analysis
Data were collected and aggregated on Microsoft Excel, and statistical analysis was performed on Stata. Continuous variables are presented as median (IQR), categorical variables are expressed as percentages (%). For continuous variables, the difference in two groups (ICU and non-ICU patients) was analysed with a t-test if the distribution was normal and a Mann-Whitney test for non-normal distribution. Variables with small sample sizes were disregarded. In the analyses, a p-value less than 0.05 is used as the cut-off for significance for univariate analysis. For multivariable analysis logistic models with clinically and statistically significant variables (from univariate analysis) were used and known confounders were added. Iterative logistic modeling was used to produce the final model.
Results
A total of 215 patients were included in the study. Among these, 186 had an outcome (death or discharge) at the end of the study period. For the remaining 29 patients, their current place of hospitalization (ICU with or without intubation or COVID-19 ward) was used. Of the 186 patients with an outcome, eight patients died (4.4%), 32 patients (17%) required ICU admission. Among ICU patients, 26 (15% of the total population) were intubated. Twenty-nine people were still hospitalised at the time of analysis. Mortality was not used for outcome analysis because of a low number of events.
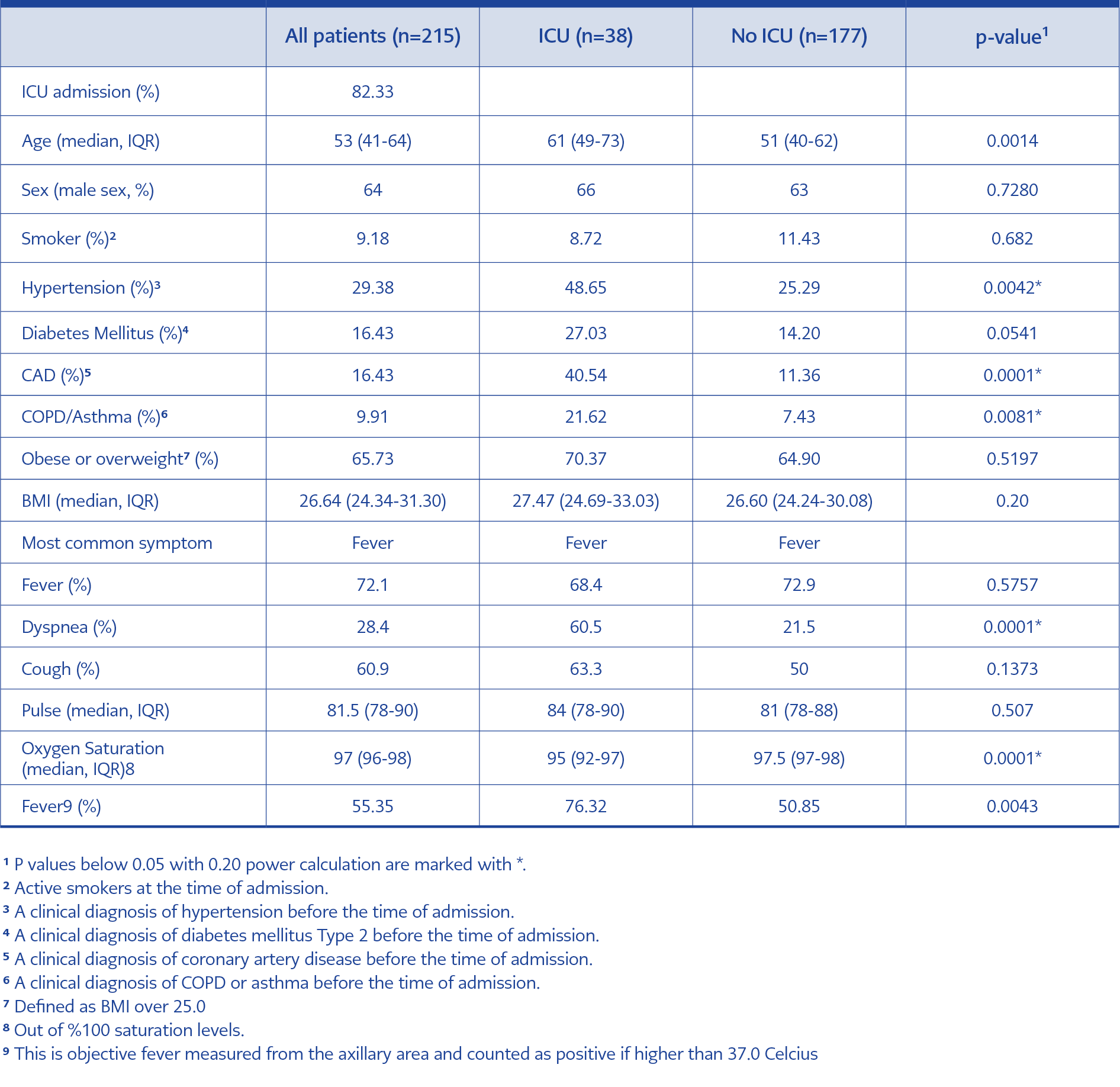
The median age was 53 (IQR: 41-64). Sixty-three per cent of the patients were male. The most prevalent comorbidity was hypertension (29.38%), followed by coronary artery disease (16.43%). The most common symptom was fever, with more than two out of three patients presenting with the symptom (Table 1).
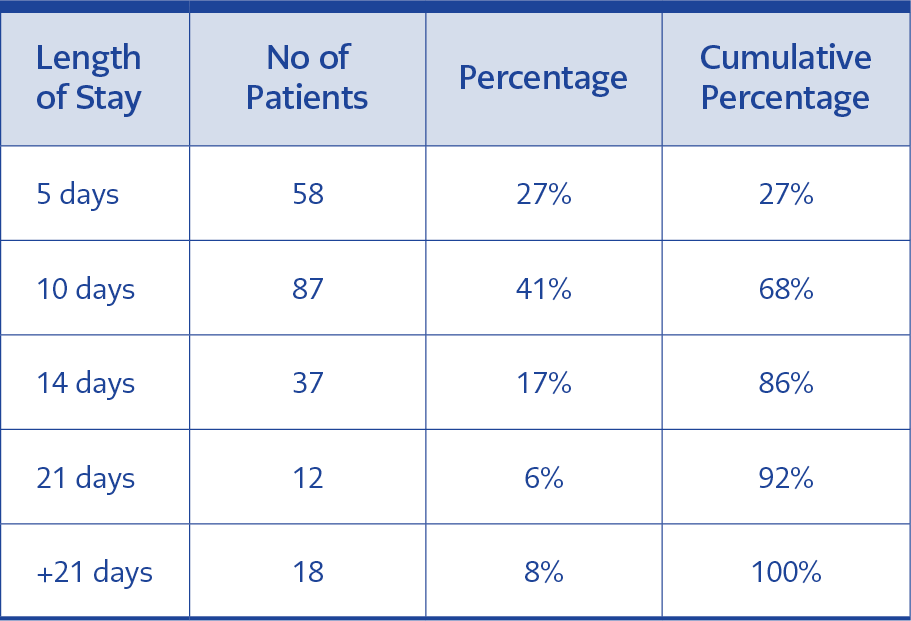
The majority of patients had an outcome within ten days of their stay (68%). The median day for ICU admission was 2.5 days (IQR=2-5 days, mean=3.4). The median day for intubation was 4 (IQR=3-7 days, mean=5.1) (Table 2).
Comparison baseline characteristics and symptoms of ICU and non-ICU patients
The median age of patients who did not require ICU admission was 51 (IQR: 40-62), while the median age of patients who required ICU admission was 61 (IQR: 49-73), with a statistically significant difference. The proportion of men was 66% and 63% in ICU patients and non-ICU patients, respectively. However, no significant difference was found.
ICU patients’ all parameters were higher than non-ICU patients, except a fever higher than 37.0 Celsius. Besides, having coronary artery disease, hypertension, COPD or asthma were statistically significant. Diabetes mellitus was marginally insignificant (p=0.0541). In terms of presenting symptoms, ICU patients were significantly more likely to have dyspnea as compared to non-ICU patients (Table 1).
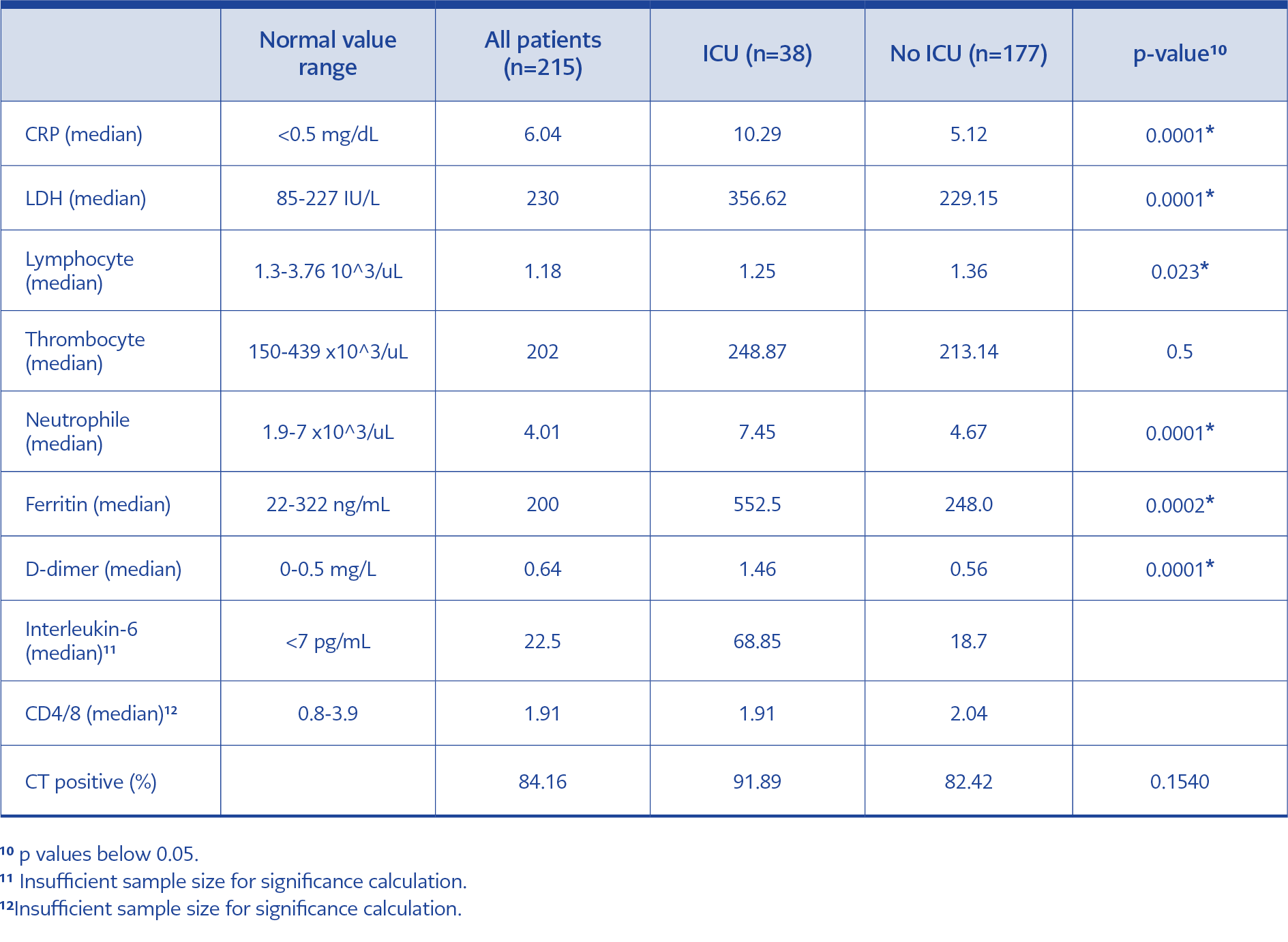
Laboratory variables and radiology
Computed tomography was the main modality of radiography, with 94% of all admissions receiving at least once. Eighty-five per cent of all patients had some sort of sign in their CT, as evaluated by at least one radiologist. No further analysis of the difference in signs (e.g. the number of lobes involved) was done. Patients admitted to ICU were more likely to have a CT suggestive of COVID-19 or viral pneumonia than non-ICU patients with proportions of CT signs 92% and 82%, respectively; however, the difference was not statistically significant.
In univariable testing for laboratory parameters, all but thrombocyte count had a significant difference between ICU and non-ICU patients. Interleukin-6 and CD4/8 values had too small a sample size for calculation (Table 3).
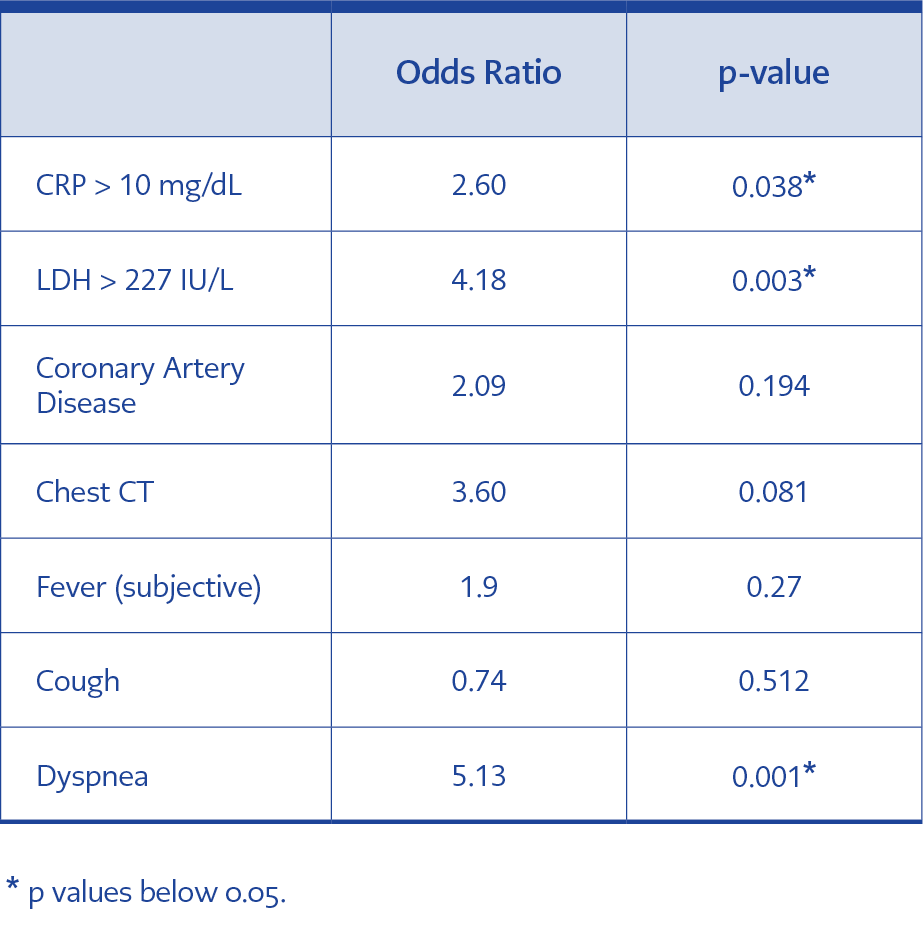
Multivariate analysis of variables (Table 4)
After adjusting for other values, significant variables were categorized with clinical evidence and previous literature. Having a CRP value of over 10 mg/dL was related to 2.6 times the odds of being admitted to ICU. Similarly, having an LDH value of over 227 IU/L (normal value limit used in our hospital) was associated with 4.3 times the odds of being admitted to ICU. Only dyspnea among presenting symptoms was associated with a significant increase in odds of being admitted to ICU (OR:5.13).
PCR results
Serial PCR tests for the patient population revealed only three of them stayed PCR(-), 0.13% of the sample.
Mortality
Only eight patients have died during the follow-up (4.4%). The median age of patients who died was 72 (IQR: 65-88). Six patients had hypertension as comorbidity, five were overweight, and all were admitted to ICU and intubated during hospitalization.
Discussion
The main objective of this observational study is to describe the baseline and clinical characteristics of hospitalized COVID-19 patients in our hospital. Further, we describe the differences in variables between patients who required ICU admission and those who did not at any time during their hospitalization.
Patients who required ICU admission were significantly more likely to be older, have hypertension, COPD or asthma, and coronary artery disease than those who did not require ICU. Even though almost two-thirds of our patients were men, the proportion of women and men in the two groups were similar. The effects of age and having coronary artery disease remained statistically significant in multivariate analysis. Among the presenting symptoms, dyspnea emerged as significant in both univariate and multivariate analysis.
These findings corroborate with other published evidence from different countries. For example, studies from China (3) and the United States (14) have shown the effects of older age and comorbidities in deteriorating outcomes in COVID-19 patients. Similar to our findings, an independent association of coronary heart disease was found in a study in Wuhan, China, although with a different outcome, mortality (2).
Laboratory markers on admission also differed between the two groups of patients. Patients admitted to ICU had statistically significantly higher levels of CRP, LDH, neutrophil, D-dimer, and ferritin and low levels of lymphocyte. Multivariate analysis showed independent and significant effects of LDH and CRP after adjustment with age and sex. High levels of LDH and CRP on admission may be a useful marker to predict ICU admission. Other studies have reported the predictive value of varying factors for disease progression. CRP, along with male sex, comorbidity, and lymphopenia, was shown as predicting severe outcomes in a study from China. (15) In our group, lymphocyte count was significantly lower in the ICU patients. While this relationship did not hold in the multivariate analysis, it is an important parameter used by clinicians in our hospital for decision making and prognostic value.
Our study has several limitations. First, it is a descriptive analysis of patients who were hospitalized for COVID-19, and thus, the characteristics of patients who were isolated at home are not included. Second, this study was designed to investigate baseline characteristics and present clinical, laboratory, and radiological differences of ICU and non-ICU patients. Therefore, analysis of changes in clinical and laboratory parameters in the disease course was not carried out. It should, however, be noted that although the progression of the disease can be quite different between patients, severe outcomes are usually seen in those who have a more serious clinical presentation on admission. (16) Third, for some of the characteristics known to be a risk factor for deterioration of the disease, such as diabetes mellitus, we could not show statistical significance, most likely because of sampling size limitations.
However, the study has several strengths. We included all patients admitted with both suspect and confirmed COVID-19 infection to our hospital, decreasing the likelihood of missing cases which may be PCR (-) at the beginning of the infection. Indeed, results of follow-up tests among PCR (-) patients revealed that only three of them stayed PCR (-). Third, in terms of important comorbidities such as hypertension and diabetes mellitus, our study sample reflected the high levels seen in Turkey. This may have helped to increase the statistical power of our study despite the relatively small sample size. In addition, we used electronic records combining two databases to ensure completeness and accuracy of the records analysed.
This is among the first studies from Turkey analysing the baseline and clinical characteristics and outcomes of hospitalised COVID-19 patients. Although our findings are similar to those described in previous studies from other countries, our patient population was younger than seen in other country settings (17), reflecting the relatively young age structure of the country.
Conclusion
COVID-19 pandemic is evolving worldwide while information on the virus, disease, and epidemiology of the disease is constantly changing. During a global pandemic, predictive values to anticipate the progress of the disease and triage accordingly are important to relieve the burden of the disease. This study presents and compares baseline characteristics of COVID-19 infected patients in ICU and non- ICU settings. In this rapidly evolving crisis, descriptive studies are of value to create more intervention side hypotheses. Our study found that having a coronary artery disease in the baseline, presenting with dyspnea, having high CRP and LDH levels in the first laboratory results upon admission were associated with a higher probability of being admitted to ICU because of COVID-19 anytime during the hospital admission.