Introduction
Nosocomial infections (NIs) constitute a major health issue in terms of morbidity, high mortality, prolonged hospitalization, and increased costs of direct patient care (1). While beds in intensive care units (ICUs) constitute less than 10% of all hospital beds, more than 20% of all NIs develop in the ICU (2). The human lifespan has been prolonged as a result of developments in medicine. It is well known that the body’s resistance to infectious diseases decreases with age. There are many reasons for this condition decrease. For example, the leading dysfunction is observed in the immune system, which begins to respond more slowly and weakly to the antigens it encounters. Organ dysfunctions such as diabetes mellitus, atherosclerosis, prostate hypertrophy, degenerative joint disorders, dementia, chronic pulmonary disease, and heart disease appear more commonly in advanced ages as microorganisms enter the body more easily and illness occurs. Prostheses replaced in regions like the heart and joints may cause infection in older people. Urine and stool incontinence and pressure sores developing in bedridden patients are other factors facilitating infections in older people (3, 4).
Therefore, the geriatric age group will require ICU admission more frequently, and serious challenges will occur during treatment (5). Although many studies are investigating NIs in the ICU, a few studies investigate NIs in geriatric ICU patients. Therefore, the primary endpoint of this study was to evaluate NIs in geriatric patients followed in the ICU. The secondary endpoint is the evaluation of factors affecting mortality in geriatric patients with NI.
Materials and Methods
The study was performed in the third-level general intensive care units of two hospitals (a research and education hospital in Kütahya and a state hospital in Kocaeli) between April 2018 and April 2019. Two ICUs with 10 and 13 beds were investigated in both hospitals. The study was approved by the Ethics Committee of Kocaeli University School of Medicine with research project number of KÜGOKAEK 2018/100 (07.03.2018).
Patients over 65 years of age admitted to the ICU for more than 48 hours were included in the study. NI was diagnosed according to the Centers for Disease Control and Prevention (CDC) criteria (6). The patient’s demographic characteristics, underlying diseases, possible risk factors, treatment, treatment responses, and mortality data were prospectively recorded along with clinical and laboratory findings of NIs in the forms prepared for daily ICU visits.
The statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) 17.0 program (IBM Corp., Armonk, NY, USA). The Mann-Whitney U test was used for intergroup comparisons of non-normally distributed parameters, while the Pearson chi-square test and Fisher’s exact test were used to compare data. The logistic regression analysis was used to evaluate independent variables. Statistical significance was set as p<0.05. therapy for the causative agent.
Results
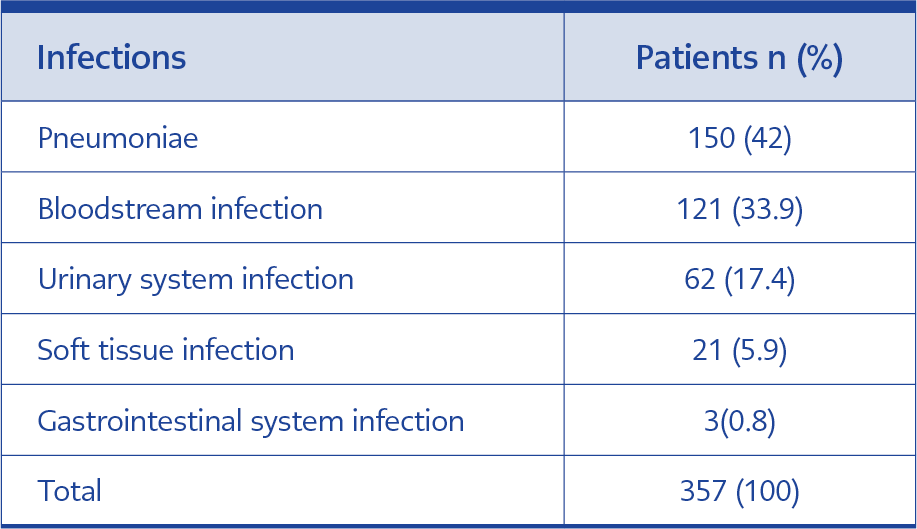
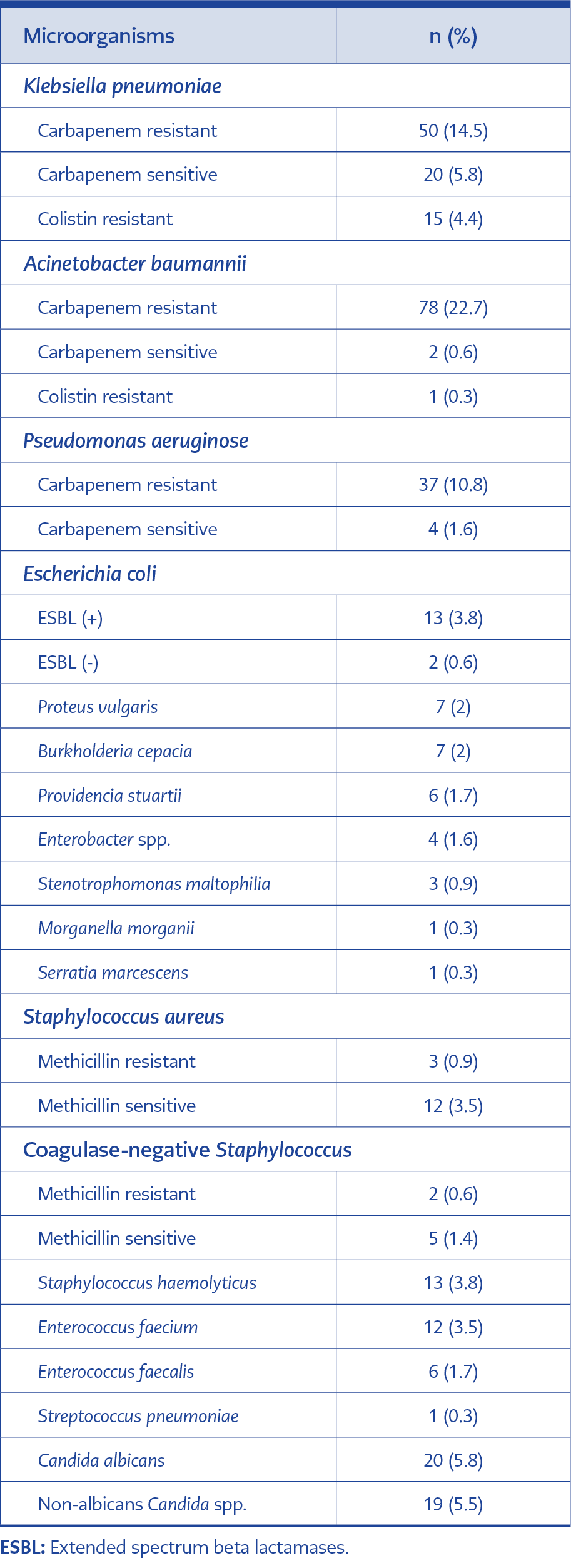
Four hundred and forty-six patients were included in the study. Three hundred and fifty-seven of the patients developed infections (80%). Pneumonia developed in 150 patients (42%), bloodstream infections (BSIs) in 121 patients (33.9%), urinary system infections (UTIs) in 62 patients (17.4%), soft tissue infections (STIs) in 21 patients (5.9%), and gastrointestinal system infections (GSIs) in 3 patients (0.8%) (Table 1). The causative agents of infections were isolated in 92.7% (331/357) of patients. The most frequently detected microorganisms were as follows: Klebsiella pneumoniae in 85 patients (24.7%); Acinetobacter baumannii in 81 patients (23.5%); Pseudomonas aeruginosa in 41 patients (11.9%); Candida albicans in 20 patients (5.8%); Escherichia coli in 15 patients (4.4%); and Staphylococcus aureus in 15 patients (4.4%) (Table 2).
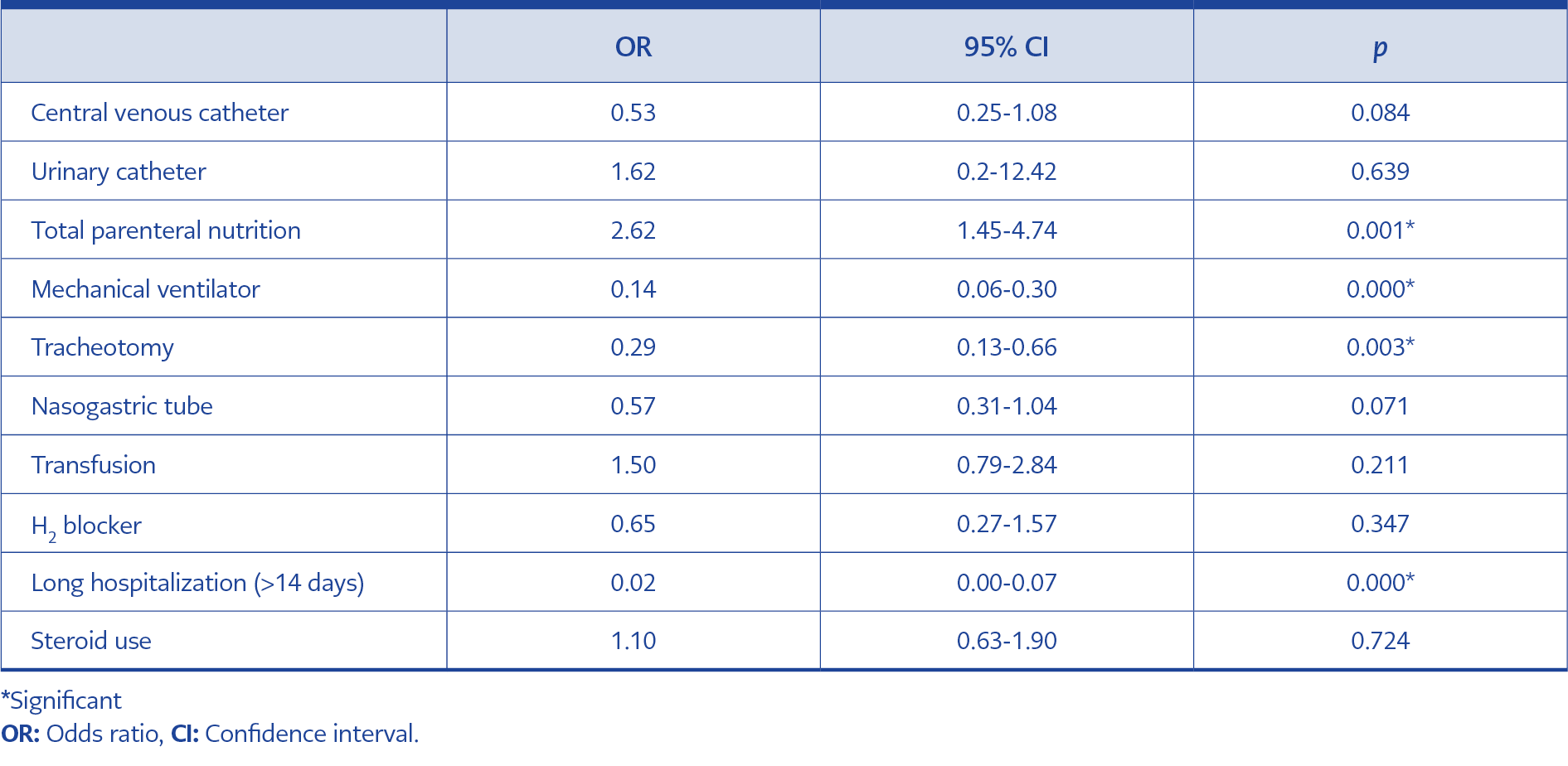
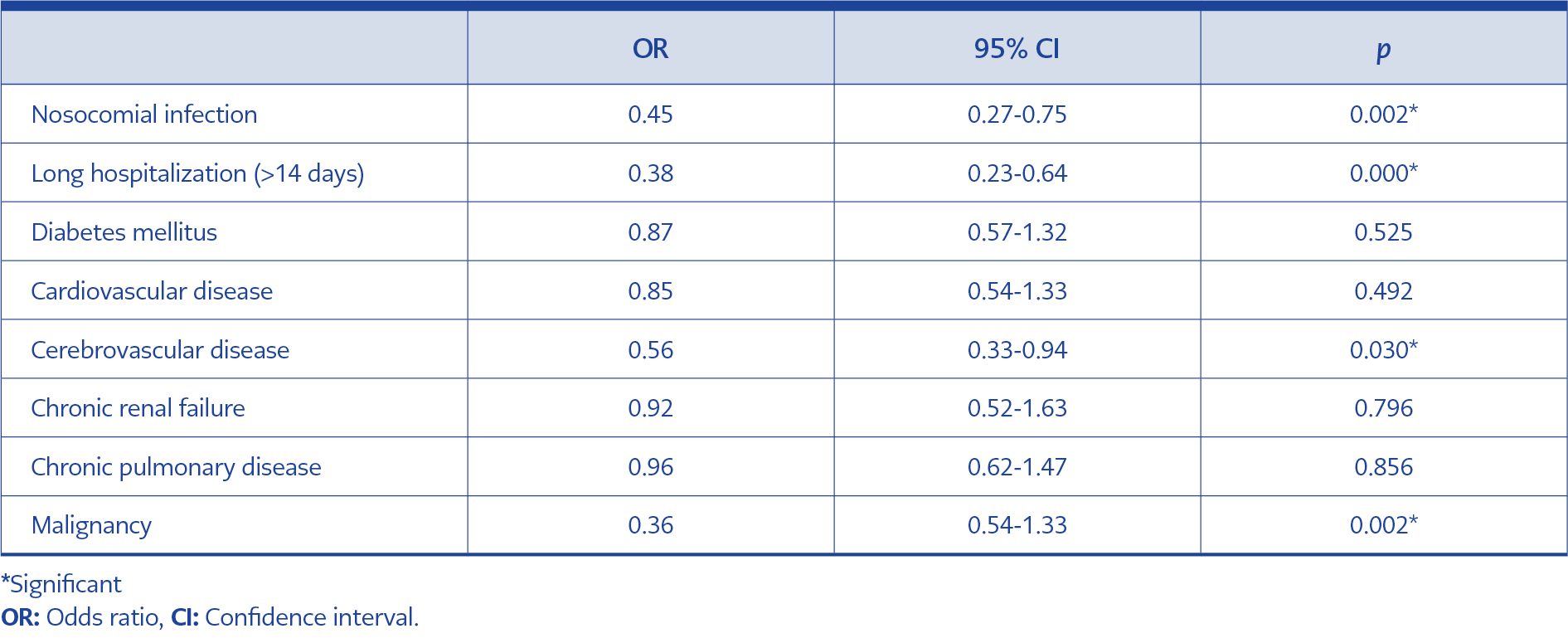
When the risk factors for the ICU were investigated in patients, mechanical ventilation (MV) support (p=0.000), prolonged hospital stays (>14 days) (p=0.000), total parenteral nutrition (TPN) (p=0.001), and tracheostomy (p=0.003) were found statistically significantly higher in patients developing ICU infections compared to the rest (Table 3). The overall mortality rate was 53.6% (239/446) in the geriatric patient group and 39%. The mortality rate was statistically significantly higher in the geriatric patient group compared to the nongeriatric adult patient group (p=0.002). When the risk factors for mortality were investigated in the geriatric patient group, prolonged hospital stays (>14 days) (p=0.000), NI development (p=0.002), malignancy (p=0.002), and cardiovascular disease (CVD) (p=0.030) were statistically significantly higher in patients developing mortality compared to the others (Table 4).
Discussion
The characteristics of NIs may vary among countries, in different cities, and even from hospital to hospital (7). A significant portion of patients admitted to adult ICUs was comprised of patients 65 years of age and older (8, 9). In our study, the NI rate in geriatric patients was determined to be as high as 80%. Another study investigating NIs in the geriatric age group in our country found a similarly high NI rate (8). The cause of this situation may be the susceptibility of the geriatric age group to infectious diseases and the prolongation of life expectancies of the elderly population in the ICU as new treatments have been developed (3, 4).
In an EPIC-II study investigating NIs of 13,796 adult ICU patients in 75 countries, a multicenter study including eight centers, and another two studies performed in our country investigating geriatric NIs, pneumonia was established as the most common type of NI, similar to our findings (8-11). NIs caused by multidrug-resistant organisms (MDRO) lead to serious problems in ICUs. NIs caused by carbapenem- or colistin-resistant organisms were frequently observed in our units. Therefore, early detection of carriers by active surveillance of MDRO, immediate isolation of patients, effective use of personal protective equipment (PPE), and adherence to hand hygiene are necessary (12).
NI develops because of underlying diseases, acute diseases causing hospitalization, the impairment of host defense mechanisms due to invasive interventions or treatments, and colonization by pathogens (12, 13). Emergency surgery at the time of hospitalization, admission after trauma, a referral from another hospital, the presence of underlying chronic obstructive pulmonary disease, cancer, HIV, immunosuppression, MV support, renal replacement treatment, and higher simplified-acute-physiology-scores (SAPSs) were associated with a higher risk of NI development in an EPIC-II study (10). In other studies investigating NIs in the geriatric age group, the use of antimicrobial agents or an invasive device, surgical procedures, acute or chronic renal failure, neurological disorders, MV support, a central venous catheter (CVC), and the duration of hospitalization were determined as risk factors for NI development (8, 14, 15). In our study, MV, prolonged hospital stay (>14 days), TPN, and tracheostomies were statistically significantly higher risk factors in patients developing NI compared to patients not developing NI. In many developed countries, NIs are among the parameters used to assess the quality of healthcare services, and they develop policies to prevent them. Determining NI risk factors will aid the development of new strategies to prevent NIs in the ICU (16).
Depending on the populations investigated and the definitions used, hospital infection-associated mortality rates varied between 12% and 80% (13). The study investigating adult patients in the ICUs found advanced age, NI, MV, SAPS II, renal replacement treatment, cancer, cirrhosis, immunosuppression, and emergency surgery as risk factors for mortality (10). In the study investigating the geriatric ICU group, advanced age, the presence of NI, chronic disease, malignancy, MV, CVC, and the duration of hospitalization were determined as risk factors for mortality (8). In another study investigating the results of elderly patients in the ICU, it was determined that their mortality was higher than that of younger patients; the severity of the disease, deterioration in consciousness, and NI were risk factors (17). Similarly, in our study, the mortality rate was statistically significantly high. When the risk factors for mortality were investigated in the geriatric patients, prolonged hospital stays (>14 days), the development of ICU infection, malignancy, and cerebrovascular accident (CVA) were statistically significantly higher in patients who developed ICU infection compared to those who did not.
Our study has some limitations. Firstly, it is including low number of patients and conducted in only two centers with general ICU. Secondly, we evaluated only the data of geriatric patients and made no comparison among different age groups in adults.
Due to higher life expectancies of the elderly population in the ICU thanks to new diagnoses and treatments, geriatric patients make up an important part of patients admitted to adult ICUs. However, the weakening of their immune systems and organ functions with age and the development of comorbid diseases make them more susceptible to NIs and mortality. Therefore, strategies should be further developed by determining ICU risk factors to prevent nosocomial infections.