Introduction
Influenza-like illness (ILI) can be caused by a range of respiratory viruses in adults (1). Influenza is one of the most important respiratory viruses that affects all age groups and can lead to hospitalizations. Severe influenza and complications can cause significant morbidity and mortality during pandemics, epidemics, and sporadic outbreaks (2-3). Therefore, influenza is monitored by surveillance systems to monitor virus activity, diagnose the circulating viruses effectively, and inform society about epidemics or pandemics (4). In several countries, including Turkey, influenza is monitored with active ILI and severe acute respiratory infections surveillance systems (5).
It is difficult to distinguish influenza from other respiratory viruses with clinical and laboratory findings alone (6). Molecular tests are required to make a definitive diagnosis, but these tests are not available in every center. Clinical and laboratory findings may be useful in predicting influenza and initiating early treatment in these conditions.
In this study, we carried out an active, hospital-based ILI surveillance during the 2015-2017 influenza seasons. We aimed to determine the frequency of influenza infections among acute admissions with ILI and evaluate the demographics, clinical findings, and outcomes of patients with influenza admitted to a university hospital.
Materials and Methods
This single-center, prospective, active surveillance study was carried out in Hacettepe University Hospital between 2015 and 2017. The Ethics Committee of Hacettepe University School of Medicine approved the study on December 16, 2015, with the decision number 15/809-39. The first season started on December 21, 2015, and ended on April 1, 2016; the second season started on December 16, 2016, and ended on April 14, 2017. Data were collected following the basic reference protocol of the Global Influenza Hospital Surveillance Network (GIHSN) coordinating center.
Global Influenza Hospital Surveillance Network (GIHSN)
GIHSN was established in Spain in 2012 to contribute to hospital-based influenza surveillance by focusing on severe influenza cases. GIHSN was based on a public-private partnership between research institutes, hospitals, and various laboratories around the world and aimed to investigate the epidemiology of seasonal influenza in different countries (7). The main aim is to evaluate the burden of severe influenza cases and the distribution of influenza virus types and to determine the protective effects of seasonal influenza vaccines on patients. A total of 29 hospitals in nine countries (Russia, Czech Republic, France, Turkey, China, India, Spain, Mexico, and Brazil) participated in the 2015-2016 season, and more than 40 hospitals in 14 countries (Czech Republic, Romania, Spain, Kazakhstan, Turkey, Russian Federation, India, Tunisia, Ivory Coast, South Africa, China, Canada, Mexico, Peru) participated in the 2016-2017 season (8, 9).
Patient Groups and Follow-Up
Patients with community-acquired ILI who were hospitalized for at least 24 h in the Adult Emergency Services, Hematology Services, Bone Marrow Transplant Services, Internal Medicine Intensive Care Unit, and Hematology Intensive Care Unit in Hacettepe University Hospital were screened according to certain influenza-predicting ICD-10 codes at the time of hospital admission. Adult patients who were ≥ 18 years old and met the European Centre for Disease Prevention and Control (ECDC) criteria for ILI (the presence of at least one of the systemic symptoms, including acute onset fever, malaise, headache, and myalgia, and at least one of respiratory symptoms such as cough, sore throat, and dyspnea within seven days before admission) were included. Patients who refused to provide consent, were institutionalized, had a history of hospitalization in the previous 30 days, and were admitted to the hospital for more than 48 hours were excluded from the study. Nasopharyngeal and pharyngeal swab samples were taken from patients who were eligible for the study and gave written consent by filling out a questionnaire within 24 hours of admission.
Data Collection and Sampling
Patients’ data were obtained by interviewing them or their relatives through a GIHSN form, which included ILI symptoms, demographic characteristics, comorbidities, and vaccination status. Data on laboratory results, chest X-rays, hospitalization and discharge ICD-10 codes, intensive care unit admission, death or discharge status, and mechanical ventilation were obtained from the hospital management information system. The presence of pneumonia was determined according to clinical findings and chest radiography. Patients who were vaccinated at least 14 days before the onset of ILI symptoms were considered vaccinated.
Nasopharyngeal or pharyngeal samples were collected in a VIROCULT® transport medium (Medical Wire & Equipment, Corsham, United Kingdom) and transported daily to the laboratory. The samples that could not be sent to the laboratory on the day of collection were stored at 4-8 °C and sent to the laboratory within three days.
Laboratory Procedures
A virological examination of the samples was performed at a reference accredited laboratory designated by the study. All eligible patients who consented were swabbed and tested for influenza with real-time (RT) polymerase chain reaction (PCR) based Multiplex Influenza A, B, C Kit (TibMolbiol, Berlin, Germany) for the detection of influenza pathogens on the CFX96 platform (Bio-Rad, Hercules, USA).
Statistical Analysis
The descriptive data were stated as frequency and percentage for categorical variables and median (IQR=25-75%) or mean± standard deviation for continuous variables. The conformity of the data to normal distribution was evaluated with the Shapiro-Wilk test. Comparisons between groups were achieved using the chi-square test for categorical variables. For non-categorical variables, Mann-Whitney U and Student’s t-test were used.
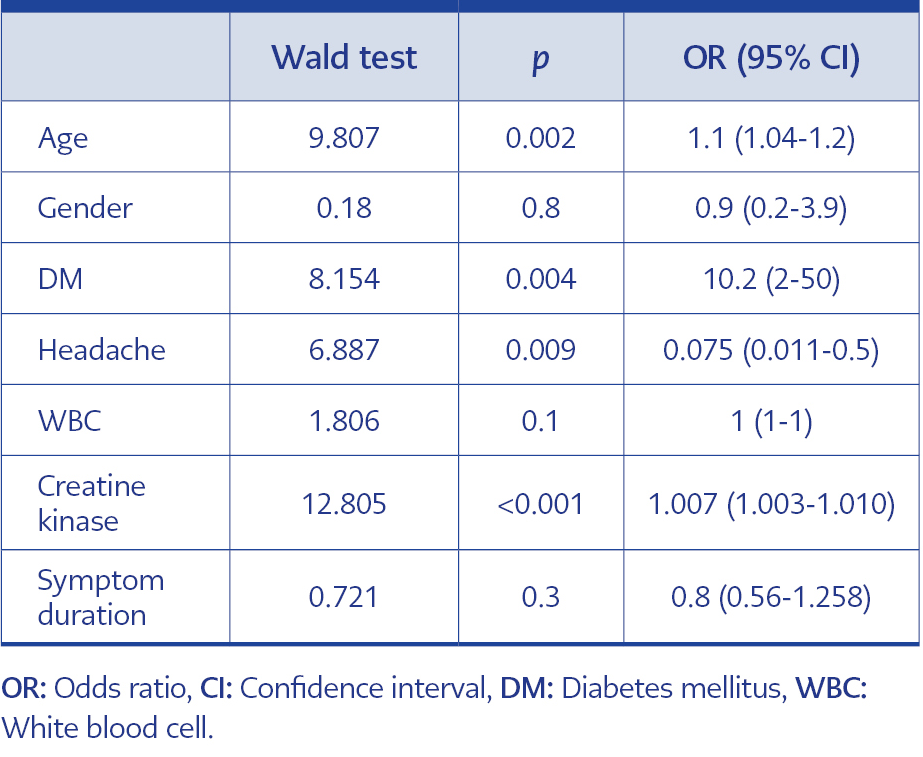
First, univariate analyses were performed for influenza-positive and -negative groups. Clinically important variables such as age and gender, and also variables with a p-value ≤0.2 from univariate analyses (headache, presence of diabetes mellitus (DM), symptom duration, white blood cells, alanine transaminase [ALT], aspartate transaminase [AST] and creatine kinase [CK]) were included in the logistic regression models. AST and ALT were removed from the model, as there was a continuous correlation between these variables and creatine kinase. Influenza-positive patients with and without pneumonia were compared with univariate analysis in terms of clinical and laboratory findings. A p-value <0.05 was considered statistically significant in the statistical analysis. The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 20.0 (IBM Corp., Armonk, NY, USA).
Results
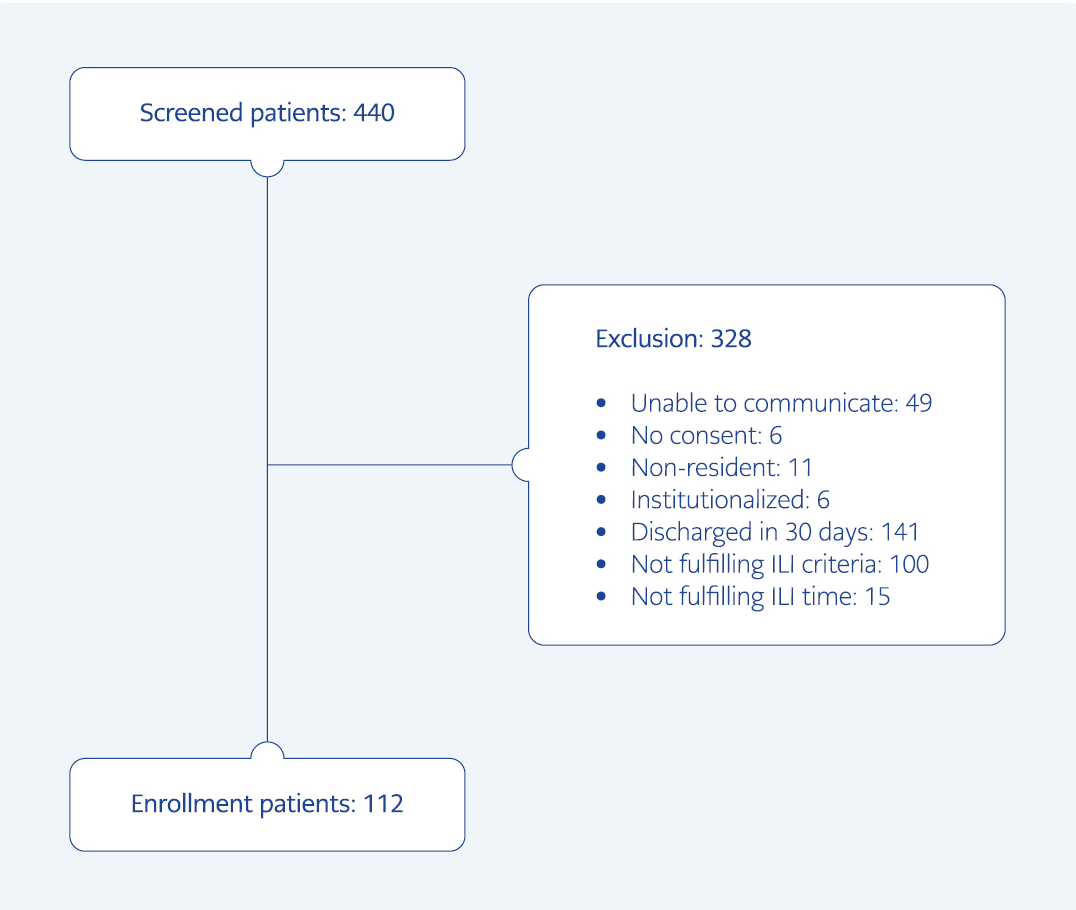
In the 2015-2016 and 2016-2017 influenza seasons, 440 patients were screened according to influenza-related ICD-10 diagnostic codes. Of these patients, 328 were excluded from the study, and 112 patients whose clinical findings were compatible with ILI were included. The flowchart and exclusion criteria of the study are presented in Figure 1.
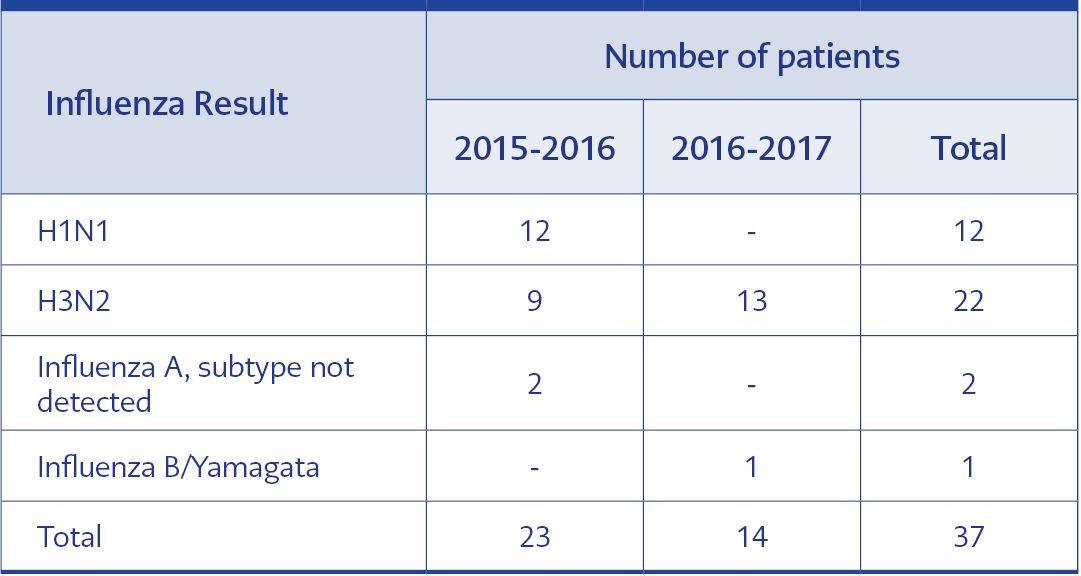
Influenza positivity was detected in 37 of the 112 patients. Influenza subtypes according to the seasons are presented in Table 1. In 2015-2016, the first case was detected on December 22, 2015 (51st week), and the last case was detected on February 19, 2016 (8th week). In 2016-2017, the first case was detected on December 19, 2016 (51st week), and the last case was detected on February 27, 2017 (9th week).
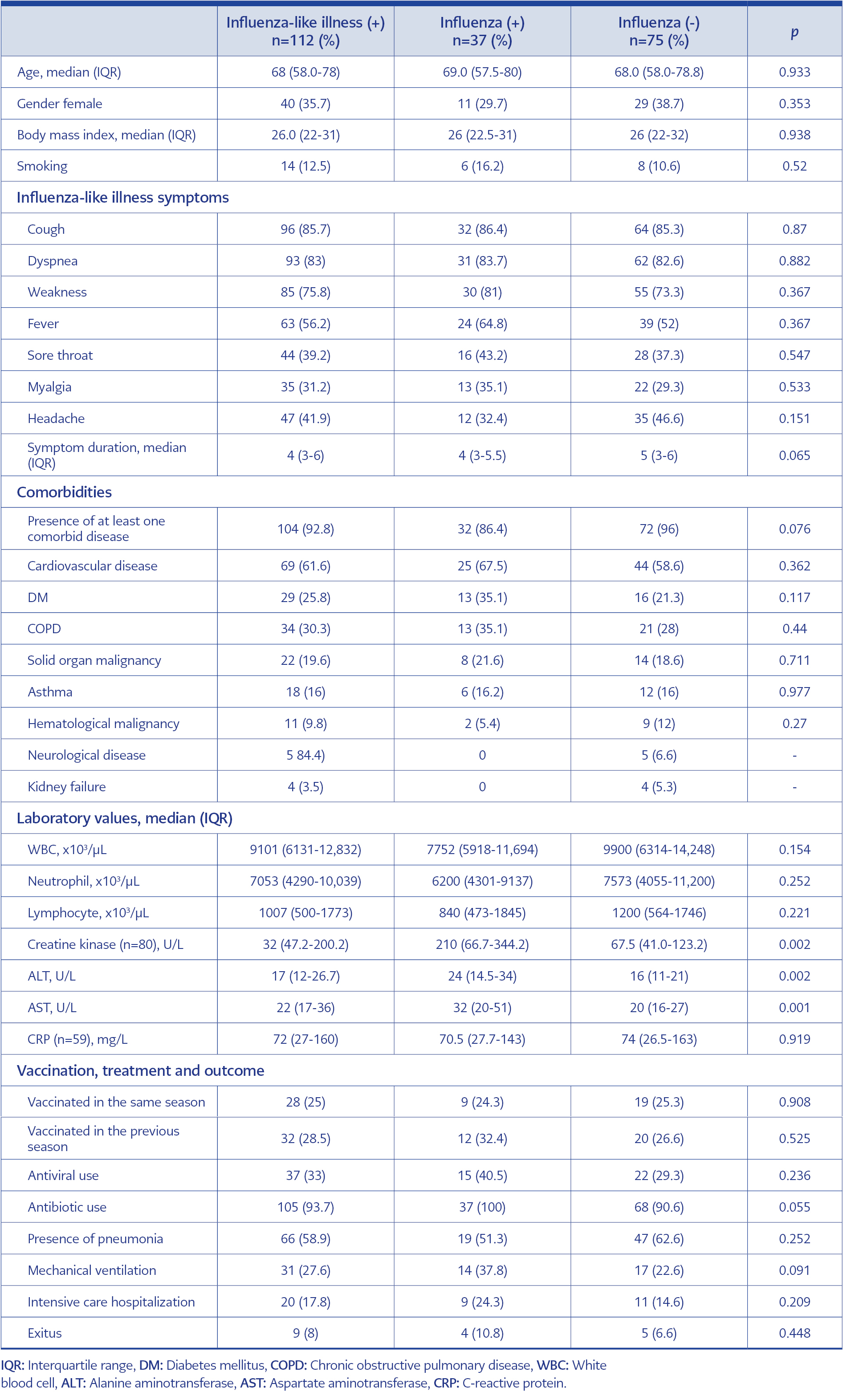
Table 2. Comparison of influenza-like illness positive, influenza-positive and influenza- negative patients.
Demographic characteristics, comorbidities, clinical and laboratory findings, and mortality status of ILI-positive, influenza-positive, and influenza-negative patients are presented in Table 2. When influenza-positive and -negative groups were compared, ALT, AST, and CK elevations were found to be significantly higher in the influenza-positive group. In multivariate analysis, a significant association was found between age, DM, headache, CK elevation, and influenza positivity (Table 3).
Differences between influenza subtypes were also investigated in our study. When the symptoms, comorbidities, laboratory results, and outcome of H1N1 positive (n=12) and H3N2 positive (n=22) patients were compared, only sore throat was more common in the H1N1 group than in the H3N2-positive group (66.7%, 27.3%; p=0.025, respectively), there was no difference in other parameters (Supplement Table 1).
When influenza-positive patients with and without pneumonia were compared, the rate of vaccination in the same season was higher in patients without pneumonia than in patients with pneumonia (38.8%, 10.5%; p=0.04). Apart from this, there was no difference in demographic and clinical characteristics between the two groups. (Supplement Table 2).
Discussion
In this study, we evaluated influenza surveillance results in community-acquired ILI patients who required hospitalization and evaluated the characteristics of influenza patients and different influenza subtypes. Influenza positivity among ILI patients was 31.5% and 35.8% in the 2015-2016 and 2016-2017 seasons, respectively. Our national influenza surveillance data reported influenza positivity rates of 43.3% and 23.7% in similar seasons (5, 10). The dominant influenza subtype was influenza A(H1N1) in the first season and influenza A(H3N2) in the second season, which is compatible with national and world data (5, 10-12). Refaey et al. and Tadesse et al.’s surveillance studies showed that influenza positivity among ILI cases was 13% and 25%, respectively. The results of a literature review and meta-analysis demonstrated the influenza positivity rates of 36% in outpatients, 24% in inpatients, and 33% in total patients in the WHO European Region between 2004 and 2017 (13-15). The influenza positivity rate among all ILI cases in our study and surveillance reports is generally low. Nearly two-thirds of patients in our study were influenza-negative, although their clinical findings were compatible with ILI. Other respiratory viruses presenting with similar symptoms and other non-infectious conditions can also contribute to ILI cases (5, 10). Therefore, the integration of molecular tests detecting both influenza and other respiratory viruses into influenza surveillance programs can raise the efficacy and quality of these programs.
The most common symptoms of influenza are sudden onset of fever, headache, myalgia, and fatigue. A sore throat, dry cough, and runny nose may accompany it. Especially in older people, symptoms such as weakness, fatigue, loss of appetite, and dizziness can be seen without typical respiratory symptoms (16). In this study, the most common symptoms in influenza-positive patients were cough (86.4%), dyspnea (83.7%), fatigue (81%) and fever (64.8%). Although the frequency of symptoms differs between studies, fever, cough, and dyspnea are the most frequently reported symptoms in influenza-positive patients (17-19). The frequency of symptoms was similar between influenza-positive and negative patients except for headache, which was more prevalent in the influenza-negative group. Wansaula et al. found that headache was the only symptom that was more prevalent in influenza patients than other respiratory viruses. However, there was no difference between influenza-positive and negative patients in terms of symptoms (19). In contrast to our findings, some studies showed that patients with influenza were more likely to present with fever and cough than those who tested negative (17, 18). According to our results and the literature, clinical findings alone are not sufficient to predict influenza positivity.
Different ILI case definitions are used in influenza surveillance programs. While there is a requirement for fever in the ILI case definition of the WHO, U.S. the Centers for Disease Control and Prevention (CDC), and the Republic of Turkey Ministry of Health, fever is not required in the ECDC definitions (20, 21). In our study, we used the ECDC case definition and found that more than one-third of influenza patients did not have a fever. Considering the high number of elderly patients with absent or blunted fever responses or patients who have medication that suppresses fever, it is beneficial to use the ECDC case definition to capture more influenza-positive patients.
In this study, influenza-positive patients exhibited higher AST, ALT, and CK levels than influenza-negative patients. However, white blood cell counts, neutrophile and lymphocyte counts, and C-reactive protein levels were similar between groups. Influenza is known as the most common cause of virus-associated rhabdomyolysis; therefore, elevations of CK, aldolase, lactate dehydrogenase, ALT, and AST are frequent (22). Similarly, in Güner et al.’s study, mean levels of CK and AST were significantly higher in influenza patients. In Shlomai et al.’s study, CK levels were significantly higher in influenza patients (23, 24). These laboratory findings can help distinguish influenza-positive cases from influenza-negative ones in clinical practice.
Studies comparing clinical findings and outcomes among patients infected with different influenza virus subtypes show different results. Many studies could not demonstrate any difference between influenza subtypes (25-27). In our study, the clinical findings, comorbidities, and outcomes between patients with H1N1 and H3N2 were also similar, except for sore throat, which was more common in the H1N1 group. Since none of the findings lead to definitive results in predicting influenza subtype, confirmation by molecular tests is required.
The interaction between advanced age, chronic diseases, and the risk of influenza virus infection has been frequently described (17). In this study, 59.4% of influenza-positive patients were ≥65 years old, and 86.4% had comorbid diseases. The high comorbidity rate in our study is probably related to the inclusion of only severe influenza cases requiring hospital admission. The most common comorbid diseases were cardiovascular disease, DM, chronic obstructive pulmonary disease (COPD), solid organ malignancy, asthma, and hematological malignancy, in the order of frequency. According to multivariate analysis, DM increased influenza risk by 10.2 fold and advanced age by 1.1 fold. Similarly, in Allard et al.’s study, patients with diabetes have a three-fold increased risk for hospitalization due to influenza virus-induced complications (28).
Pneumonia is one of the serious complications of influenza and an independent risk factor for mortality (29). Pneumonia was present in half of the patients in this study. 63% of patients with pneumonia were ≥65 years old, and the most prevalent underlying diseases were cardiovascular disease, DM, and COPD. Demographics, clinical findings, and outcomes were similar between influenza-positive patients with and without pneumonia. The only difference was the vaccination status in the same season, which was higher in patients without pneumonia, as expected. According to our results, vaccination in the same season reduced the risk of pneumonia; however, vaccination in the previous season had no protective effect. Although vaccination is the major route of preventing influenza and related complications, the vaccination rate in our study population was very low. Twenty-five percent of patients had influenza vaccination in the same season, and 28.5% had had it in the previous season. Adult vaccination programs should be improved to reach wider target populations.
Antibiotic resistance is a significant threat to health and is mainly the consequence of inappropriate use of antibiotics in several indications. Respiratory tract infections are among the most common indications in which antibiotics are overused and misused (30). Our study findings supported this fact; antibiotic use in ILI cases and influenza-positive patients was 94% and 100%, respectively. In contrast, antiviral drugs were used only in 40% of influenza-positive patients. Implementing rapid molecular tests in clinical practice may decrease antibiotic misuse and increase the appropriate use of antiviral drugs.
The main limitation of our study is that we had a relatively small sample size for such a common disease. Another limitation is that we could not screen non-influenza respiratory viruses, such as adenovirus, parainfluenza viruses, and human coronaviruses. These viruses can cause clinical findings similar to influenza, and their inclusion in ILI and severe acute respiratory infection surveillance will significantly contribute to the surveillance programs. Nevertheless, the main strength of this study depends on the prospective and active surveillance design. Although many surveillance studies include outpatients, we focused on severe influenza cases requiring hospital admission.
In conclusion, conditions other than influenza contribute to ILI cases more than influenza. Therefore, the integration of molecular tests detecting both influenza and other respiratory viruses into influenza surveillance programs can increase the efficacy and quality of these programs. Clinical features in influenza-positive patients were not mainly different from those in influenza-negative patients; however, laboratory parameters may be helpful. The elevation of AST, ALT, and CK in influenza cases can be considered in distinguishing influenza from other ILI cases. Vaccination in the same season can reduce the risk of pneumonia in influenza-positive patients.