Introduction
Hepatitis B is an important global infectious disease. With its high prevalence and serious complications, such as liver cirrhosis, hepatocellular cancer, and death, controlling and monitoring hepatitis B is of paramount importance (1). In this context, the Global Burden of Disease (GBD) study dataset is an important resource for analyzing the prevalence and incidence of the disease, mortality rates and factors affecting changes in these parameters over time, both locally and globally.
The World Health Organization (WHO) 2021 report stated that in 2019, 296 million people had chronic hepatitis B disease, 1.5 million [1.1 million-2.6 million] people were diagnosed with chronic hepatitis B infection and 820,000 [450,000-950,000] people died from causes related to hepatitis B infection (2). The global HBsAg positivity rate is estimated to be around 3.6%, but this varies significantly across regions due to differences in factors like vaccination rates, socio-economic conditions, and healthcare access, which all influence the natural course of hepatitis B infection (3). In Türkiye, HBsAg positivity was reported as 4% (0.8-5.7%) and antiHBc total positivity as 30% in different reports published between 2014-2023 (1, 4).
The hepatitis B vaccine, which was introduced to the childhood vaccination calendar in Türkiye in 1998, was administered in a total of three doses at 3, 4 and 9th months between 1998-2002, three doses at 0 (birth), 1st, and 9th months between 2003-2006, and three doses at 0 (birth), 1st and 6th months after October 2006 (1). In addition, the catch-up vaccine was administered to children attending secondary education between 2005 and 2009. Vaccination rates started at 77% in 2002 and reached 99% in 2019 (5).
This study analyzed the change in hepatitis B incidence, prevalence, and mortality rates in Türkiye and worldwide between 1990 and 2019 and vaccination rates of one-year-olds by year.
Materials and Methods
Data Source
Hepatitis B incidence, prevalence and mortality rates were derived from the GBD dataset, which includes epidemiological indicators of 369 diseases and injuries for 204 countries and territories worldwide from 1990 to 2019, based on the GBD study age-standardized world population (6, 7). “Our World in Data” (https://ourworldindata.org/) dataset was used to evaluate immunization rates of one-year-olds by years (8). Only anonymous, publicly open data was used, and animals and humans were not included in the study. The ethical approval was not obtained due to the nature of the research, which did not necessitate ethical clearance for privacy and human subject considerations.
Statistical Analysis
Data were presented as age-standardized incidence rates, mortality rates and prevalence per thousand. Joinpoint regression analysis (JRA) was used to assess changes in hepatitis B incidence, prevalence, and mortality over time (1990-2019). In this study, logarithmic transformation was performed for rates and confidence intervals (CIs) were used to calculate the standard error (SE) (9). This analysis method was used to identify changes in trends over significant periods. Kmax was calculated to test whether the two regression mean functions between cohorts were parallel (parallelism test), and statistical significance was tested with permutation distribution (10). Annual percentage change (APC) and average annual percentage change (AAPC) were calculated. The JRA study was also used to identify breakpoints for immunization rates of one-year-olds. The JRA analysis was conducted using the Joinpoint Regression Program, version 5.0.2, provided by the United States National Cancer Institute (12). In addition, comparative analyses were performed using the R statistical programming language and RStudio and related packages.
Socio-Demographic Index
The Socio-Demographic Index (SDI), a recently introduced composite indicator, measures the level of development and its impact on health. It combines factors such as per capita income, education level for those over 15, and fertility rates for individuals under 25 (12). An SDI value of 0 signifies the lowest level of development affecting health, whereas an SDI value of 1 indicates the highest level. SDI was calculated as a geometric mean and roughly summarized by the following formula:
During the study period, the GBD study group categorized Türkiye as belonging to the “low-middle SDI group” from 1990 to 2002, the “middle SDI group” from 2003 to 2009, and the “high-middle SDI group” from 2010 to 2019 (13).
Results
The age-standardized incidence rates and prevalence trends of hepatitis B, along with age-standardized mortality rates, spanning from 1990 to 2019, are visually depicted in Figure 1.
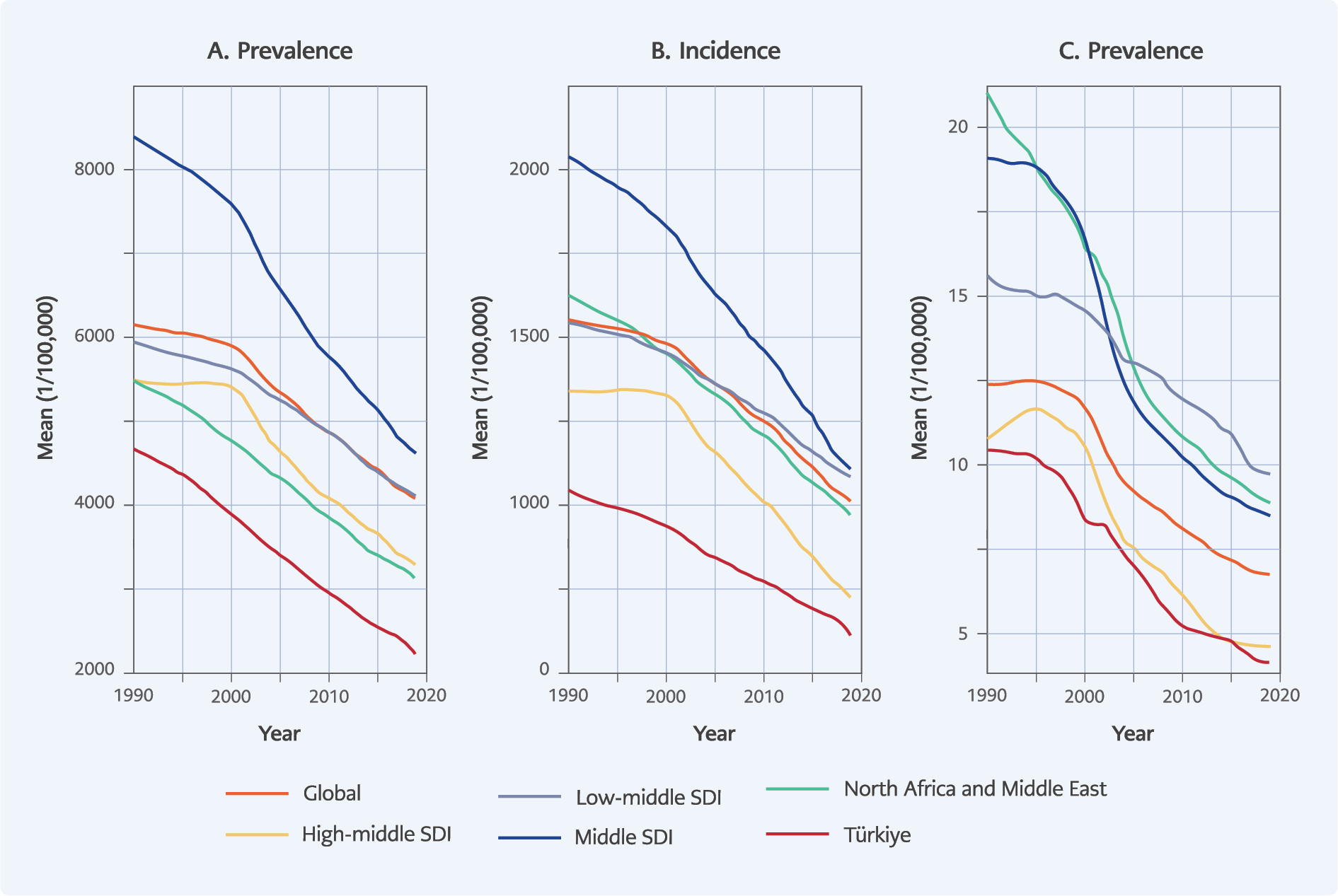
Figure 1. Comparative temporal trends in prevalence (A), incidence (B) and mortality (C) of hepatitis B rates (The Global Burden of Disease [GBD] dataset).
According to GBD data, the prevalence and incidence of hepatitis B in Türkiye were on a downward trend over the years. This trend was also observed worldwide (Figure 1). Between 2002 and 2021, Türkiye fell within the middle and high-middle SDI group based on the GBD data assessment (14). Geographically, Türkiye was part of the North African and Middle Eastern countries group. As depicted in Figure 1, the prevalence and incidence of hepatitis B in Türkiye were lower compared to its economic and geographical counterparts in the region.
As illustrated in Figure 1, hepatitis B mortality rates in Türkiye decreased consistently, mirroring the global trend and high-middle SDI countries. Notably, the slowest decline in mortality rates occurred in low- and low-middle-income countries, with rates ranging between 10 and 13 per 100,000 in 2019.
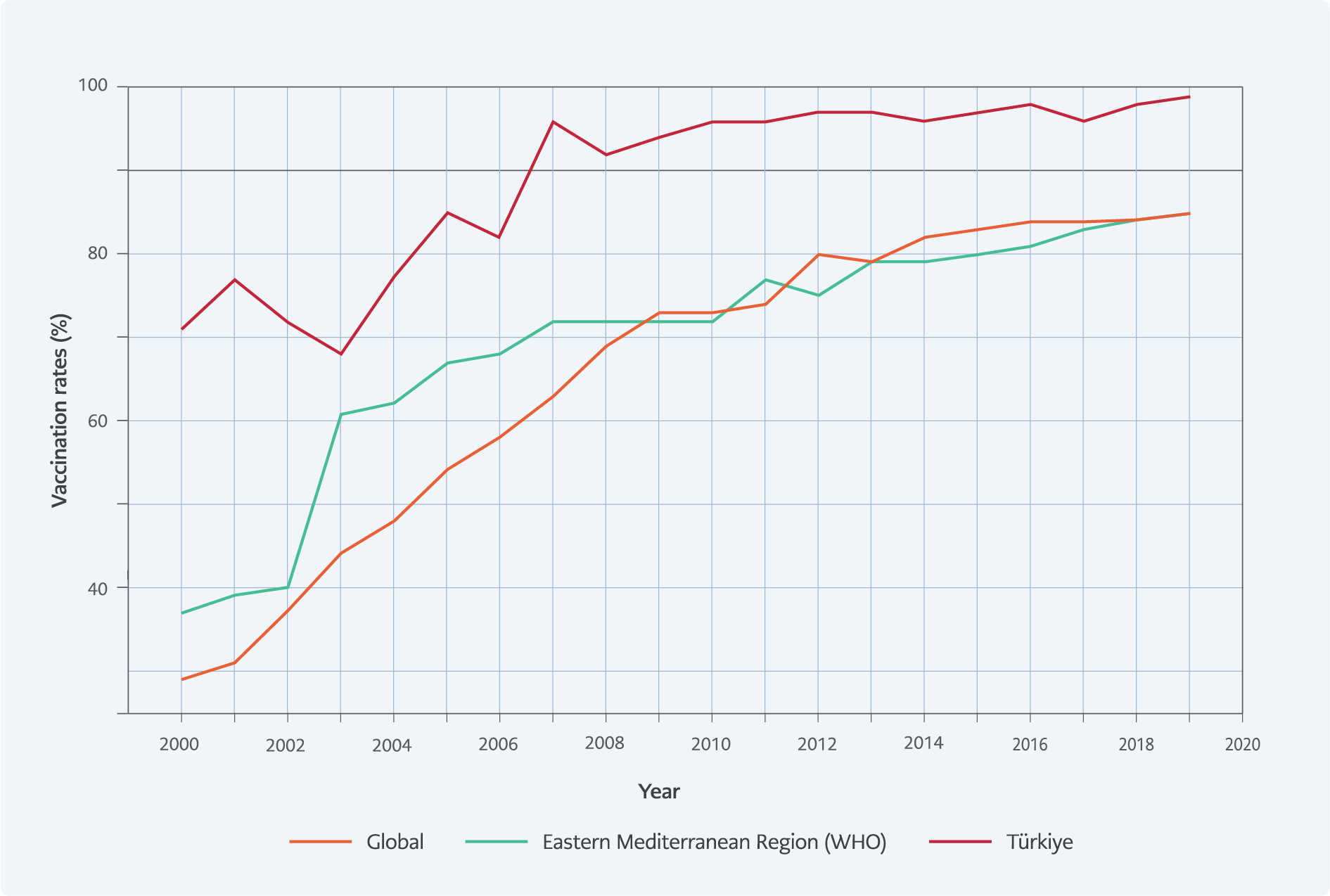
Figure 2. The temporal trends in hepatitis B vaccination coverage among one-year-olds, data-(“Our World in Data” dataset).
The temporal trends in hepatitis B vaccination coverage among one-year-olds are depicted in Figure 2. While childhood vaccination for hepatitis B in Türkiye commenced in 1998, available data begins from the year 2000 onward. The vaccination rate data source classified Türkiye within the Eastern Mediterranean countries group, and this classification was utilized for comparative purposes in the study.
In the first cohort (2000-2003), vaccination rates decreased by 1.43% annually, which was not statistically significant (95% CI: -5.91 to 1.32). In the second cohort (2003-2007), vaccination rates increased by 7.29% annually (95% CI: 4.93 to 10.52). In the third cohort (2007-2019), no significant change in vaccination rates was observed (APC=0.43, 95% CI: -0.12 to 0.88).
In the evaluation of Türkiye’s vaccination efforts, the analysis revealed marked differences in vaccination rates among children under one year of age across the three different cohort periods identified. Between 2000 and 2003, a slight but statistically insignificant decline in vaccination rates was observed; APC=-1.43% (95% CI: -5.91 to 1.32). This was followed by a significant increase between 2003 and 2007 when the APC for vaccination rates was 7.29% (95% CI: 4.93 to 10.52). However, no significant change in vaccination rates was observed between 2007 and 2019; APC=0.43% (95% CI: -0.12 to 0.88).
In the WHO Regional Office for Eastern Mediterranean, immunization rates of the one-year-old cohort experienced a noteworthy annual increase of 58.25% (APC) during the initial segment spanning from 1990 to 1995, with a 95% CI of 44.31 to 84.00. Subsequently, in the second segment, from 1995 to 2006, the annual rate of increase was 10.04% (95% CI: 6.47 to 18.62). Interestingly, during the third segment, from 2006 to 2019, there was no significant change in the vaccination rate of one-year-olds (APC=1.58; 95% CI: -4.91 to 3.86).
In the first cohort (1990-1995), vaccination rates increased by 65.64% annually, which was statistically significant (95% CI: 53.94 to 81.79). In the second cohort (1995-2006), vaccination rates increased by 17.80% annually (95% CI: 14.83 to 21.26). In the third cohort (2006-2019), no significant change in vaccination rates was observed (APC=2.36; 95% CI: 0.05 to 4.24).
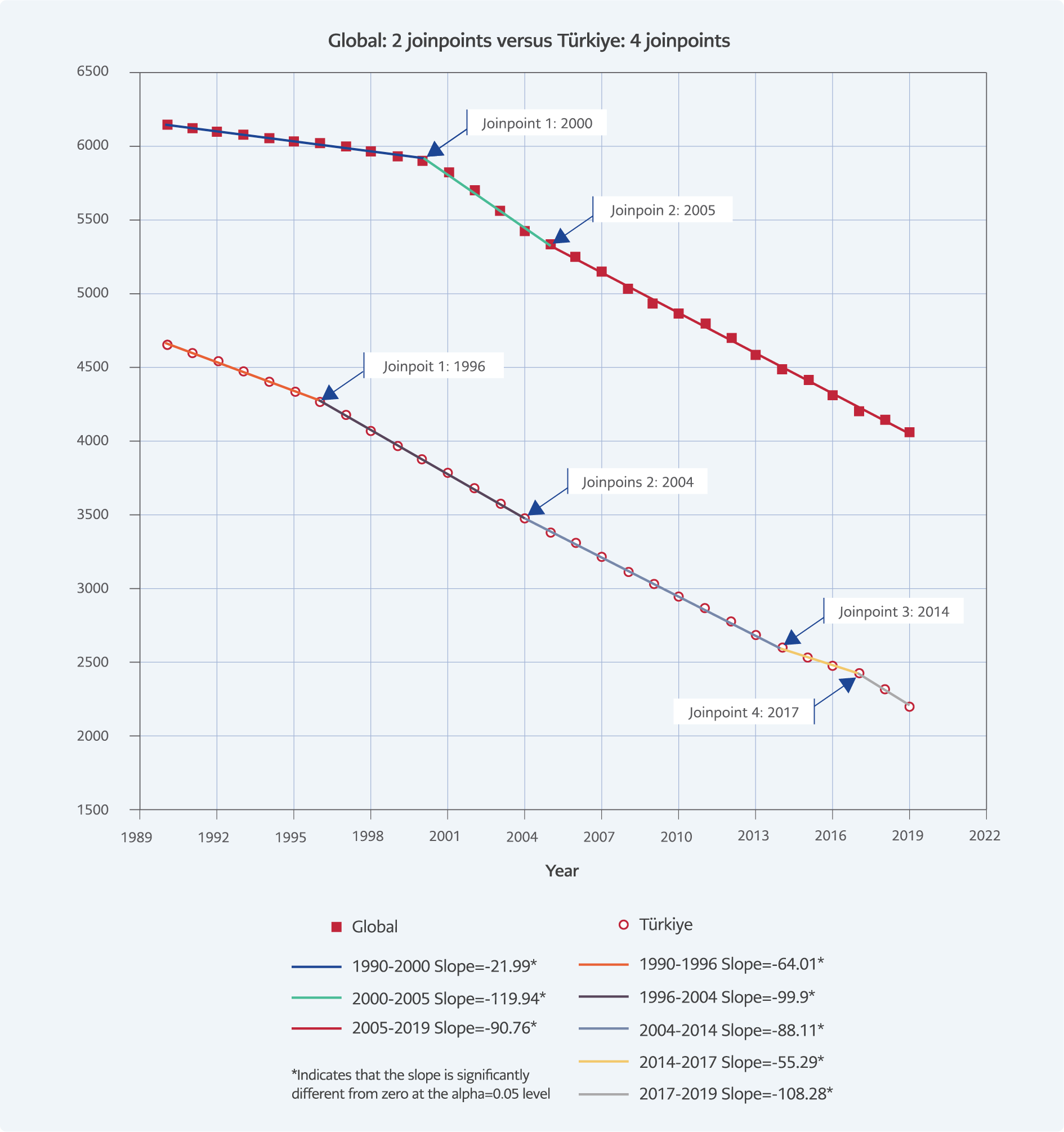
Figure 3. Comparison of trends in hepatitis B prevalence in Türkiye and worldwide with joinpoint regression analysis.
In JRA, both cohorts show clear downward trends for prevalence over the study period (Figure 3). In the global cohort, AAPC=-1.4104 (95% CI: -1.44 to -1.37). Similarly, a downward trend was observed in the Türkiye cohort with AAPC=-2.5244* (95% CI: -2.62 to -2.43). Comparison of Türkiye and global cohorts revealed an AAPC difference=1.1141 (95% CI: 1.0155 to 1.2126) between the observed trends (p<0.001).
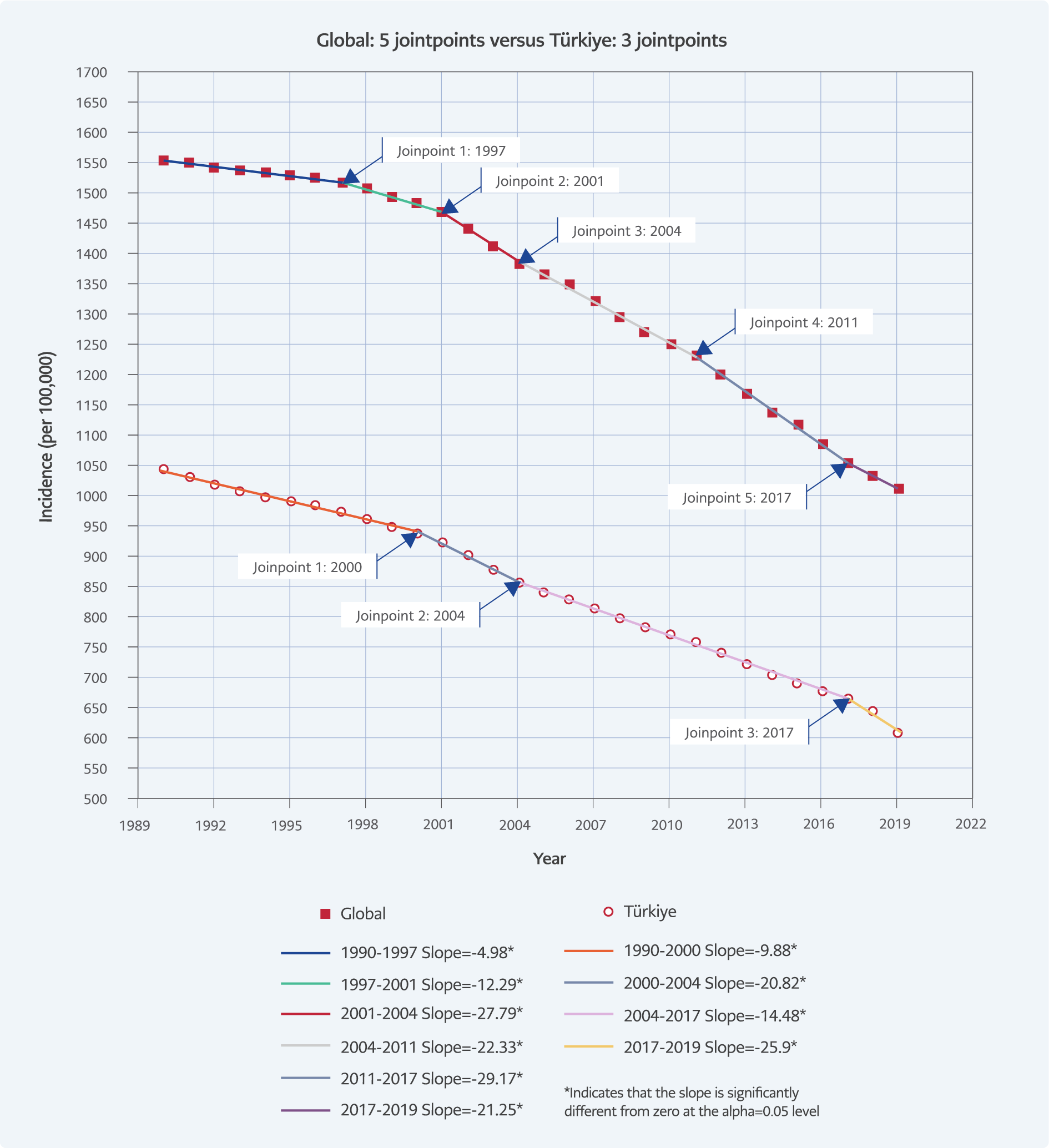
Figure 4. Comparison of the trends in hepatitis B incidence in Türkiye and worldwide with joinpoint regression analysis.
Significant decreasing trends of incidence were found for both cohorts over the period 1990-2019 (Figure 4). The AAPC value was -1.4810 (95% CI: -1.54 to -1.41) in the global cohort and -1.81 (95% CI: -1.91 to -1.70) in the Türkiye cohort. When the cohorts were compared, the AAPC difference was 0.32 (95% CI: 0.20 to 0.45) (p<0.001).
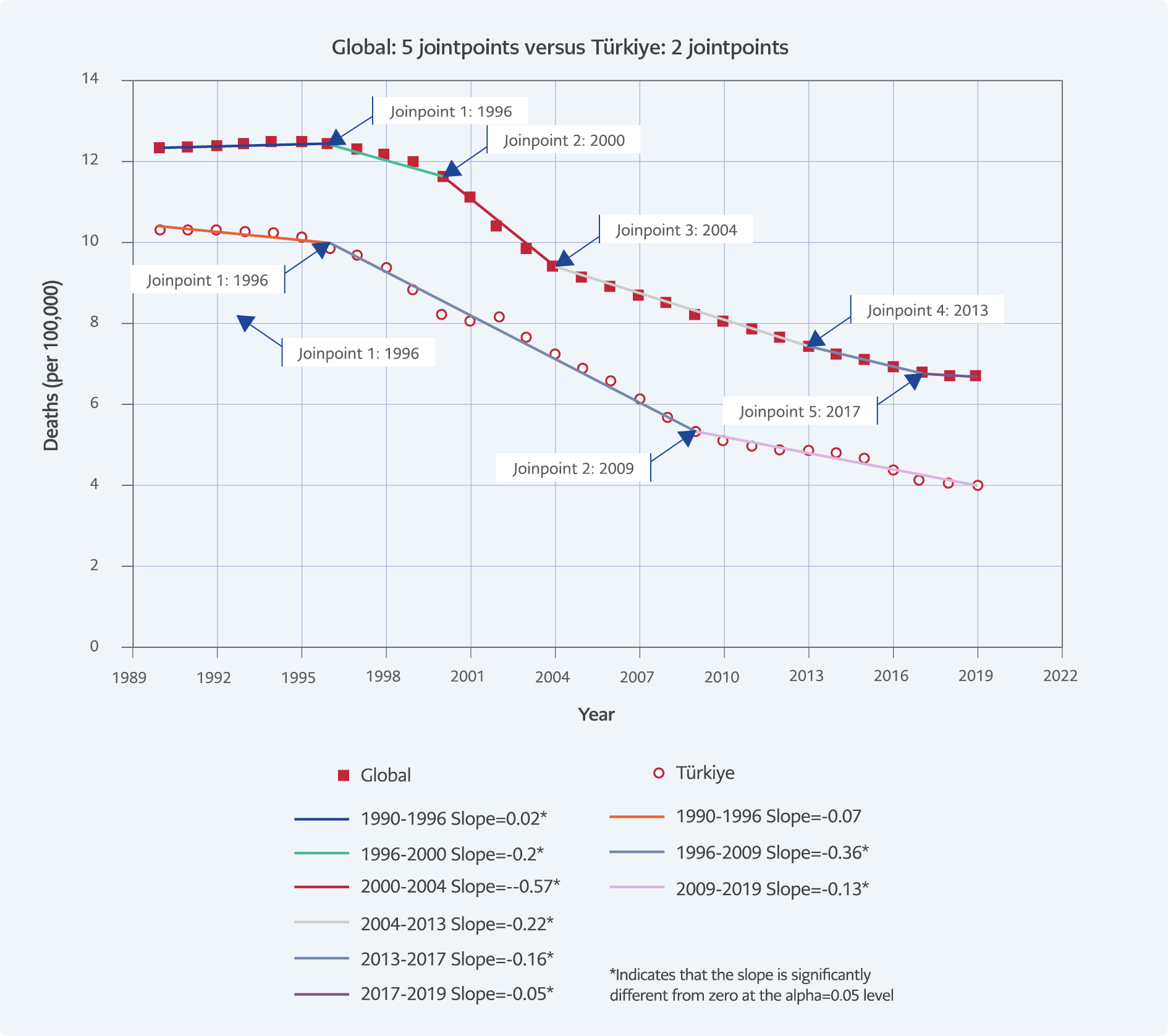
Figure 5. Comparison of the trends of hepatitis B Mortality in Türkiye and worldwide with joinpoint regression analysis.
Chronic hepatitis B mortality trends global and Türkiye are depicted in Figure 5. The AAPC was -2.07 (95% CI: -2.20 to -1.94) in the global cohort and -3.19 (95% CI: -3.58 to -2.80) in the Türkiye cohort. When the cohorts were compared, an AAPC difference of 1.12 (95% CI: 0.70 to 1.53) was observed (p<0.001).
Hepatitis B vaccination rates analyzed with JRA revealed the following:
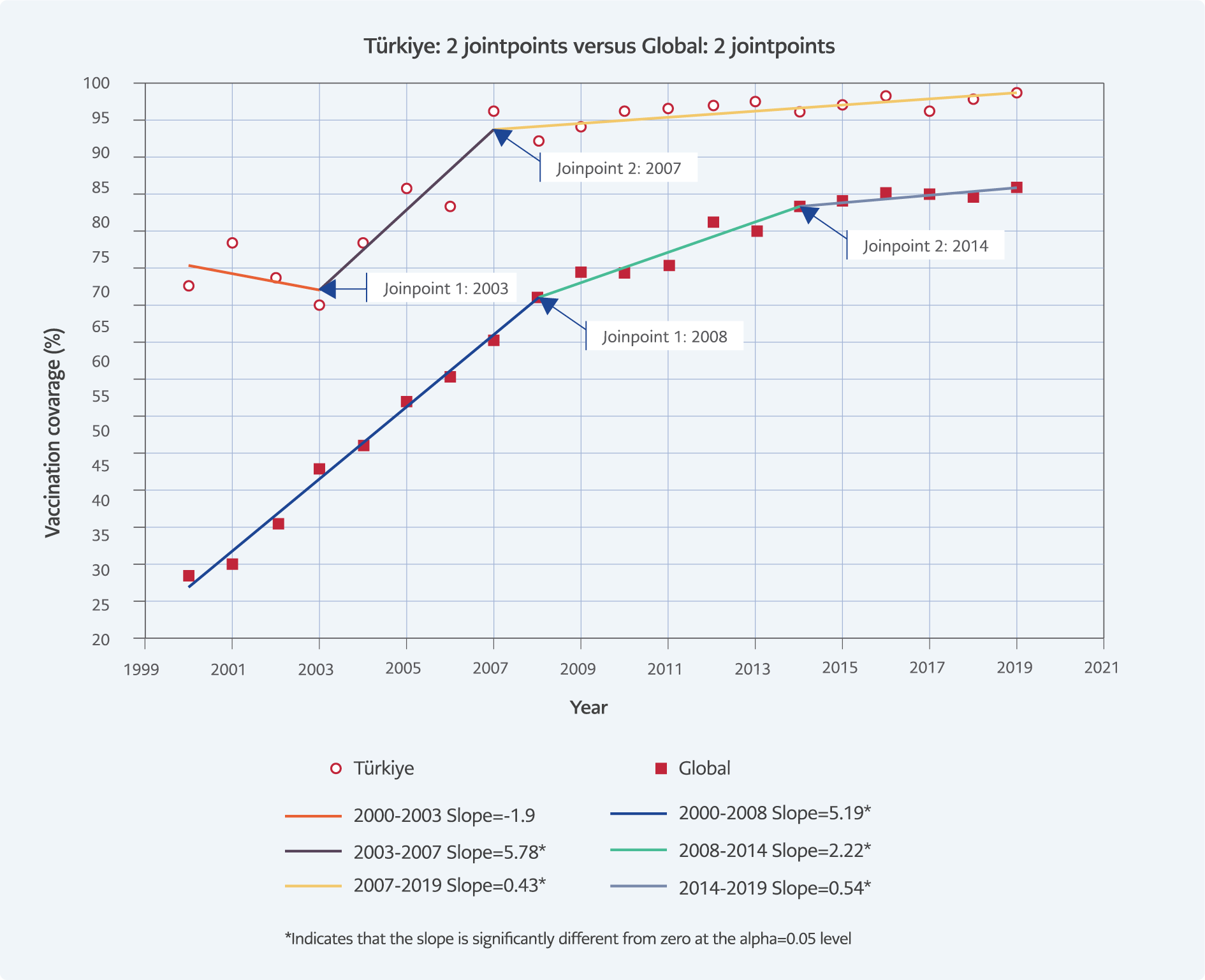
Figure 6. Comparison of trends in hepatitis B immunization under one year of age in Türkiye and worldwide with joinpoint regression analysis.
Significant differences in immunization rates of one-year-olds were observed between Türkiye and the global cohorts in the period 2000-2019 (Figure 6). In Türkiye, AAPC=1.5378 (95% CI: 0.5429 to 2.5426) and worldwide AAPC=6.0980 (95% CI: 5.2241 to 6.9791). Cohort comparison found an AAPC difference of -4.5602* (95% CI: -5.8905 to -3.2299) between observed trends (p<0.001).
Discussion
Since the late 20th century, a deeper understanding of hepatitis B transmission and progression has led to global health policies for its control. Key milestones include the introduction of passive immunization with hepatitis B immunoglobulin in 1974 and the development of the first plasma-derived vaccine in 1981 (14), followed by the recombinant hepatitis B vaccine in 1986 (15). The WHO’s recommendation published in 1991 for universal hepatitis B vaccination led to the inclusion of the vaccine in childhood vaccination programs across 177 countries by 2008 (16, 17). Hepatitis B prevalence, incidence and mortality rates due to hepatitis B are on a downward trend both in Türkiye and worldwide (18, 19).
For a decrease in prevalence, either a decrease in incidence or an increase in mortality or both are expected as presented simply in the following formula where P(t) is the prevalence at time t, P(t−1) is the prevalence at the previous time period t−1, I(t) is the incidence rate at time t, D(t) is the death rate due to the disease at time t:
P(t)=P(t-1)+I(t)-D(t)
The study showed that the decrease in incidence was accompanied by a decrease in mortality. Hence, prioritizing vaccination for children under 1 year of age, where the risk of chronic infection is anticipated to reach 90%, and for children aged 1-5 years, where the likelihood of chronicity is expected to range from 30-50%, holds particular significance in diminishing the overall prevalence of the disease (20). Using the Joinpoint Regression Program allowed us to pinpoint the periods during which these significant reductions occurred, particularly following the introduction and expansion of childhood vaccination programs. This statistical evidence reinforced the hypothesis that high vaccination coverage was critical for the observed declines in hepatitis B prevalence. A prominent illustration of the success of childhood vaccination programs was found in Taiwan, where the earliest initiative resulted in a remarkable reduction of HBsAg carriage among individuals under 20 years of age—from 10% to less than 1%—over a span of 20 years (14).
The introduction of the hepatitis B vaccine in Türkiye’s childhood immunization program in 1998 led to a significant increase in vaccination rates, which consistently remained above 95% since 2007, despite a brief dip in the early 2000s. According to the study findings, the prevalence of chronic hepatitis B in Türkiye has shown a noteworthy decline from 5% to 2% over a span of 30 years. This study confirmed the effectiveness of these vaccination efforts, showing a notable decline in hepatitis B incidence, prevalence, and mortality rates both in Türkiye and globally, as depicted in Figures 1, 3, and 5. In comparison, high SDI countries typically exhibited a prevalence rate of around 1%. Notably, Türkiye, positioned within the high-middle SDI group and geographically situated between North Africa and the Middle East, maintained hepatitis B incidence and prevalence levels below those observed in these regions (Figure 1). This indicates that Türkiye achieved statistically significant and commendable success in the battle against hepatitis B when compared with countries within its socio-economic and geographical regions. Nevertheless, studies in Türkiye reported HBsAg positivity rates ranging between 0.8% and 5.7% across various epidemiologic groups. Consequently, it would be beneficial to formulate targeted policies by identifying and addressing specific groups with these distinctive epidemiologic characteristics (21, 22).
The Joinpoint Regression Program (12) was employed in this study to analyze the trends in hepatitis B incidence, prevalence, and mortality rates over time. This statistical tool allowed us to identify significant changes in trend data by fitting a series of joined straight lines to the log-transformed data. The program identifies the points where there is a significant change in the trend (called “joinpoints”) and calculates the annual APC for each segment. This analysis was crucial in detecting the periods during which significant changes occurred in hepatitis B rates, particularly in response to public health interventions like vaccination programs. Significant decreasing trends in both prevalence and incidence were observed (Figure 3 and Figure 4), with the APC reflecting these reductions in the global cohort. Similarly, the analysis of mortality trends (Figure 5) showed a consistent decline, underscoring the success of global health strategies in combating hepatitis B. The temporal trends in hepatitis B vaccination coverage among one-year-olds, as shown in Figure 2 and Figure 6, further support the impact of these vaccination programs. The significant increase in vaccination rates from 2003 to 2007 correlated with a substantial reduction in hepatitis B incidence and prevalence during the same period.
Tosun and colleagues performed a population-based study with a large pregnant women cohort to evaluate the hepatitis B screening program (4). The authors observed that while the rates of HBsAg testing in pregnant women increased, the rates of HBsAg positivity significantly decreased over the years. They concluded that the existing vaccination programs may have been effective in reducing the prevalence of hepatitis B in the general population. Our study supported this finding. However, the authors argued that to reduce further the risk of mother-to-child transmission, a new vaccination program specifically targeting pregnant women should be implemented. In addition to this, they advocated for making HBsAg testing mandatory for all pregnant women, which would enable early identification and management of hepatitis B infection, thereby minimizing the risk of vertical transmission. If implemented, the authors believed these measures would contribute significantly to the national goal of reducing the prevalence of hepatitis B infection in Türkiye. Obviously, in addition to the success achieved with vaccination, preventive health services such as screening of blood donors, family screenings in people with chronic hepatitis B, and close monitoring of pregnant women are important in hepatitis B control. However, these issues are beyond the scope of the study.
In conclusion, the consistent declines in prevalence, incidence, and mortality underscored the effectiveness of childhood vaccination programs. The data strongly indicate that these programs significantly reduced new infections, thereby lowering the overall burden of hepatitis B. This highlights the critical need to maintain high vaccination coverage to sustain these reductions and move toward eradication.