Introduction
Percutaneous transhepatic cholangiography (PTC) is an invasive procedure used in patients with obstructive jaundice in the progress of some malignancies to reduce bilirubin levels, improve liver functions, prolong survival and enable other treatments. The procedure is critical because of its potential complications. The most common complications are bloodstream and biliary tract infections secondary to bacteremia. Different infection rates have been reported in previous studies, such as 67 of 343 patients (19.5%), 46 (30%) of 152 patients, and 83 (43%) of 193 patients (1, 2, 3).
Multiple mechanisms have been blamed for the development of infection, such as reduction in intestinal T-cells and natural killer cells in patients with obstructive jaundice, reduction in neutrophil count and function in mice with obstructive jaundice, and cellular membrane with various oxidative enzymes secreted from neutrophils (4, 5). In addition to cellular factors (such as the destruction of the bile), a marked decrease in the phagocytic functions of Kupffer cells despite the increase in their number was observed (6, 7). Relevantly, although the bile is sterile, in case of stasis, it provides an important basis for bacteria to live, feed and multiply, and accordingly, cases may be prone to infection (8). Furthermore, high serum bilirubin levels cause damage to the intestinal mucosa and predispose it to bacterial translocation (9). Exogenous planting directly into the biliary tract from a percutaneously placed catheter causes reaching the biliary tract by hematogenous route (10). Because the pressure of the bag that takes the bile out is lower than the intestinal lumen pressure, bacteria can reach the biliary tract more easily, and this paves the way for the development of infection in the bilioenteric anastomosis and previous instrumentation (3, 11).
Kaya et al., reported that Escherichia coli, Pseudomonas, Klebsiella spp., enterococci, and enterobacteria were the most common microorganisms in cholangitis and bacteremia developing after PTC (10). In another study, E. coli (36%), Klebsiella pneumoniae (13.5%), and Enterococcus faecalis (12%) were the most common (1). In the Tokyo Guidelines 2018, E. coli was found to be 23%, Klebsiella 16%, and Enterococcus spp. 20% in healthcare-associated cholangitis and bacteremia (12). In another study that followed patients with malignant obstructive jaundice, the Gram-negative enteric bacteria rate was 40% (3). Other studies stated that the most common causative organisms in cases of biliary sepsis after biliary intervention are E. coli, Clostridium, and enterococci (11, 13).
There is little consensus in the literature about optimal coverage for biliary procedures. However, for prophylaxis before PTC, an invasive procedure applied to the biliary tract, one gram of ceftriaxone, second-generation cephalosporins, or one and a half grams of ampicillin-sulbactam have been recommended intravenously in different studies (3, 14, 15). Another view is that prophylactic antibiotics are administered as a single dose only in cases where diagnostic imaging will be performed. In these cases, 3rd generation cephalosporins are often preferred. In the presence of comorbid disease, appropriate antibiotic therapy is administered after consultation with the clinician (3).
In the current study, patients who were followed up with different diagnoses of malignancy and underwent PTC in the medical oncology clinic of our hospital were evaluated in terms of fever, growths in blood and bile cultures, prophylaxis, and antibiotics used in treatment.
Materials and Methods
In our study, 93 patients who were followed up in the medical oncology clinic of Ankara Numune Education and Research Hospital between 2010 and 2017 and underwent PTC were evaluated retrospectively. Age, gender, primary diagnosis, and other detailed patient data were obtained from the epicrisis forms in the hospital electronic data system (FONET) and the patient follow-up files of the medical oncology clinic. In patients who underwent PTC, given prophylaxis, detected microorganisms in blood and bile cultures, and given treatments were evaluated. The criteria for diagnosing cholangitis were as follows: body temperature >38 °C, leukocyte count >10,000/mm3, right upper quadrant pain, and no infection in other parts of the body.
If a patient included in the study due to an infection attack developed another infection caused by the same type of bacteria with the same resistance pattern, the patient was not included in the study for the second time.
The Ethics Committee of Ankara Numune Education and Research Hospital approved our study on September 06, 2018, with the numbers E-18-2192. Our study was conducted in 2018, and since it is retrospective, it has been reported that the ethics committee does not require informed consent.
Statistical Analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) 20.0 program (IBM Corp., Armonk, NY, USA). Whether the quantitative variables were normally distributed was examined using visual (histogram and probability graphs) and analytical methods (Kolmogorov- Smirnov / Shapiro-Wilk tests). Descriptive analyses were reported using frequencies and percentages for categorical variables, mean ± standard deviation for normally distributed data, and median (min-max) for non-normally distributed data. The Mann-Whitney U test was used to compare the quantitative variables that were not normally distributed in two independent groups, and the Pearson Chi-Square test and Fisher’s Exact test were used to compare the categorical variables. The statistical significance was set as p<0.05.
Results
Among the cases, the mean age was 58.58 ±9.75, and 52% (n=48) were male. Prophylaxis was given to 50% (n=46) of the cases, and no prophylaxis was given to 50% (n=47) of the cases. Cephalosporin was used for prophylaxis before the intervention in 74% (n=69), and piperacillin-tazobactam in 26% (n=24). The complication rate in patients who received prophylaxis was 75% (n=35), and 82% (n=29) of these complications were fever. The complication rate in patients who did not receive prophylaxis was 59.5% (n=28), and 87% (n=24) of these complications were fever. In comparison, the growth in blood culture was detected at 34.3% (n=16) of the patients receiving prophylaxis and 29.1% (n=14) of those not receiving prophylaxis. There was no significant difference between the two groups regarding reproduction in blood culture (p=0.69).
After the intervention, complications such as cholangitis, bleeding, hemobilia, fever, and pancreatitis developed in 68% (n=63) of the cases, and all of them were consulted to the infectious diseases department. Antibiotherapy (53% [n=33] piperacillin-tazobactam, 24% [n=15] carbapenem, 23% [n=15] cephalosporin) was initiated in all consulted cases. The mean duration of antibiotic use was 9.74±4.54 days. Blood cultures were obtained in 89% (n=47) of patients with fever; however, the rate of bile culture was only 29% (n=15).
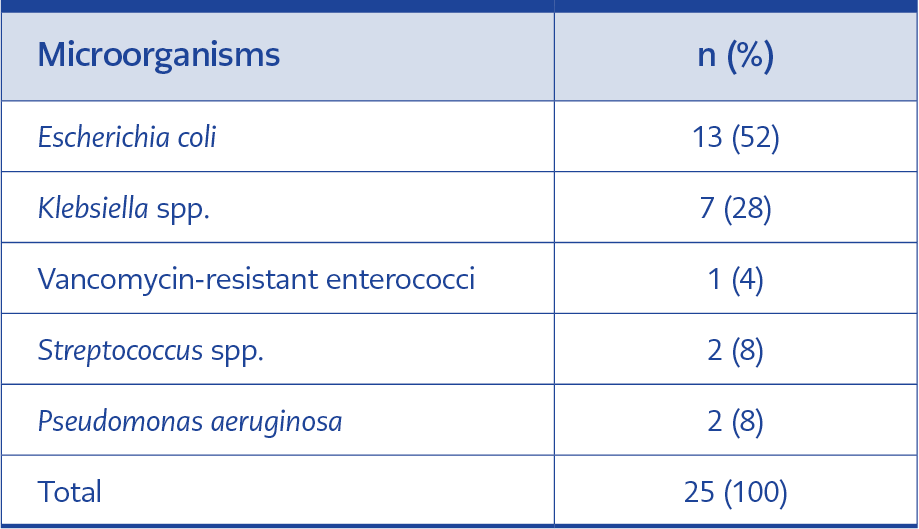
The growth was detected in 40% (n=19) of the blood cultures and 17% (n=3) of the bile cultures. We detected that 53.8% (7/13) of E. coli isolates and 85.7% (6/7) of Klebsiella spp. isolates were multidrug-resistant (extended-spectrum beta-lactamase-producing [ESBL+]). In addition, vancomycin-resistant enterococci were %4 (n=1), and Pseudomonas was 8% (n=4) (Table 1). We determined that 65% (n=15) of the empirical treatments initiated were appropriate for the detected microorganisms.
It was observed that the median length of hospital stays of patients who received antibiotic treatment for fever after PTC was 9 (min=1-max=31) days, and the median duration of hospitalization for patients without fever was 6 (min=1-max=21) days. The duration of hospitalization was significantly longer in patients with fever (p=0.003).
Discussion
One of the complications of the PTC procedure performed in oncology patients is infection (16). Infection prolongs the hospital stay and decreases the patient’s life quality (17). Oncology patients are frequently hospitalized, and they use antibiotics for various reasons. Microorganisms found in the flora of patients, colonized in the body, and being a source of infection generally have multidrug resistance (18). In our study, which detected 87% of the complications were fever, blood cultures were taken from 89% of the patients with fever. The growth was detected in 40% of the blood cultures, and 52% of the detected microorganisms were resistant.
We gave prophylaxis to 50% of the cases. Before the intervention, cephalosporin was used in 74% of the cases and piperacillin-tazobactam in 26%. Complications such as cholangitis, bleeding, hemobilia, fever, and pancreatitis developed in 68% of all cases after the intervention, and they were consulted with the department of infectious diseases. There are no randomized controlled studies and no consensus on prophylaxis. Therefore, either 1 g ceftriaxone or 1.5 g ampicillin-sulbactam was recommended based on surgical prophylaxis recommendations, and if there was biliary stasis, it was recommended to continue antibiotics until the obstruction ended (19). Our study found no significant differences regarding the growth rates and the resistance of the microorganisms. Therefore, we think giving antibiotics as treatment rather than prophylaxis is more appropriate.
We took blood cultures from 89% of the patients with fever and detected growth in 40%. Resistant microorganisms were detected in 52% (Table 1). In a study that retrospectively evaluated 409 patients who underwent PTC between January 2008 and December 2010, cholangitis was detected in 106 patients (25.9%), and sepsis was detected in 45 (42.5%) of them (20). Ginat et al., reported the overall incidence of cholangitis and sepsis after PTC as 2.1% (n=19/910 change) and 0.4% (n=4/910 change) (21). In another study of 833 patients in the United Kingdom, the rate of sepsis was 3.5% (22). Therefore, our rate of 40% was found to be quite high considering these studies.
In our study, the bile culture rate was only 29%, and a growth rate of 17% was found in these cultures. Xu et al., reported that in 193 patients with malignant biliary obstruction, biliary infection developed in 83 (43%) patients after percutaneous biliary drainage (3). In the study of Suk et al., the rate of cholecystitis was 9.7% (23). In another study, including 694 patients, growth in bile culture was 42.9% (24). Kaya et al., found the growth rate in bile culture as 50.5% (10). A study conducted in 2017 reported that biliary infection developed at a rate of 19.5% after PTC (1). Although the rate of growth in bile culture in our study was similar to the one conducted in 2017, the lower rate compared to other studies was attributed to our low rate of taking bile cultures.
We detected that 53.8% (7/13) of E. coli isolates and 85.7% (6/7) of Klebsiella spp. isolates were multidrug-resistant (extended-spectrum beta-lactamase-producing [ESBL+]). Furthermore, vancomycin-resistant enterococci were %4 (n=1), and Pseudomonas was 8% (n=4) in our study (Table 1). In the study by Kaya et al., the most frequently encountered organisms were Gram-negative bacteria, including E. coli (28.2%), Pseudomonas (17.3%), and Stenotrophomonas maltophilia (15.2%) (10). In the Tokyo Guidelines 2018, causative agents of healthcare-associated bacteremic biliary tract infections are E. coli (23%), Pseudomonas (17%), Klebsiella spp. (16%), Enterococcus spp. (20%) (12). In a study with 110 patients, 6.3% sensitive E. coli, 1.8% E. coli (ESBL+), 11% Enterococcus spp., 3.6% susceptible Klebsiella spp., 3.6% Klebsiella spp. (ESBL+) reproduced (3). Considering these studies, although the first three bacteria are common among the bacteria that usually reproduce, the ESBL rate is decisively high in our study.
Our study has some limitations. The most important one is that the patients could not be followed one by one after PTC because of the study’s retrospective nature. In addition, the parameters were obtained from the patient files, and the data reliability was lower compared to a prospective study.
In our study, the growth rate was significantly higher in blood cultures than in bile cultures. The lower growth rate in bile culture was attributed to the low number of bile cultures. There was no significant difference regarding the growth rate and drug resistance of the microorganisms. Therefore, we think giving antibiotics as treatment rather than prophylaxis is more appropriate. Taking cultures will ensure that patients receive appropriate antibiotic therapy for the causative agent.