Introduction
Peritonitis presents an inflammation of the peritoneal cavity that can develop because of infectious (bacteria, viruses, parasites, etc.) and non-infectious (chemical agents, foreign substances, etc.) causes (1). Infectious peritonitis is divided into three classes based on the source and nature of microbial contamination. Primary (spontaneous) peritonitis is the spontaneous infection of the peritoneal cavity with microorganisms without any intra-abdominal surgical focus. Secondary peritonitis is the most common form of peritonitis encountered clinically and has high morbidity and mortality rates (2). It usually occurs after the loss of integrity of an organ in the peritoneal cavity or due to a penetrating infectious process in these organs. Tertiary peritonitis is a late stage of the disease. It is defined as the persistence of signs and symptoms of peritonitis despite medical and surgical treatment of secondary peritonitis (3). Almost all of these cases occur in patients with ascites due to cirrhosis or in patients receiving peritoneal dialysis (4).
Spontaneous bacterial peritonitis (SBP), presenting with fever, abdominal pain, and mental status change, is usually seen in cirrhotic patients with a high model for end-stage liver disease (MELD) score (5). A recent systematic review reported that the prevalence of SBP in cirrhotic patients was approximately 17%, varying between regions (6). Perforation peritonitis is one of the most common emergency surgical conditions and has a mortality rate of up to 20% (7). Treatment is based on surgical treatment of the underlying pathological process, appropriate antibiotic therapy, and supportive care (8).
Early diagnosis and prompt appropriate antibiotic therapy have been shown to reduce in-hospital mortality by 20-90% in one review (9). Therefore, the local epidemiological resistance pattern should also be considered when choosing empiric antimicrobial therapy for patients with peritonitis (10). In the population-based study of Ratnasekara et al. (11), the frequencies of Gram-negative and Gram-positive bacteria isolated from SBP cases were similar, and Escherichia coli (29.7%) was the most common microorganism. The rate of multi-drug resistance among the isolated pathogens was 6.09% (11). Another meta-analysis reported that the multi-drug resistance rate among microorganisms in SBP was 11.7% (6). However, our country has limited studies on the clinical prognosis (12, 13) and microbiological profile (14) of bacterial peritonitis. Therefore, there is a gap in the distribution of pathogenic microorganisms in peritonitis cases, empirical treatment options, and clinical prognostic markers.
This study aimed to determine the clinical outcomes and mortality-related risk factors in patients with culture-confirmed peritonitis. In addition, pathogenic microorganisms and their resistance profiles were determined. The findings of this study will facilitate the selection of empirical antibiotics in peritonitis cases and provide awareness regarding prognosis in the clinical follow-up.
Materials and Methods
This single-center, retrospective study included patients aged ≥18 years who were followed up in Bakırköy Dr. Sadi Konuk Training Research Hospital with a culture-confirmed diagnosis of peritonitis between August 2015 and December 2023. Patients younger than 18 years of age, with incomplete file data, and whose pathogenic microorganisms were not isolated despite clinically suspected peritonitis were excluded. Only the first peritonitis attack of each patient was included. Patients were classified as primary or secondary peritonitis according to their etiology. Demographic characteristics (age, gender, comorbid conditions, operation status), laboratory parameters (leukocyte count, neutrophil count, lymphocyte count, albumin, C-reactive protein [CRP], creatinine, alanine aminotransferase [ALT], aspartate aminotransferase [AST]) and microbiological results of the patients were obtained from the hospital data-recording system.
Definition
Spontaneous bacterial peritonitis was diagnosed by positive ascitic fluid bacterial culture, increased neutrophil count in ascitic fluid (≥250 cells/mm³), and exclusion of secondary causes of bacterial peritonitis (15). Peritoneal dialysis-associated peritonitis was diagnosed by positive ascitic fluid bacterial culture and increased leukocyte count in ascitic fluid (≥100 cells/mm3) (16). Secondary bacterial peritonitis was diagnosed by a positive bacterial culture of ascitic fluid and an increased neutrophil count in ascitic fluid (≥250 cells/mm³) in the presence of an intraperitoneal focus. Mortality was defined as a 30-day all-cause death.
Microbiological Data
All peritoneal aspiration samples were cultivated on 5% sheep blood agar, eosine methylene blue (EMB) agar, Sabouraud dextrose agar, chocolate agar and incubated at 37°C for 24-48 hours. If there was no growth in routine cultures or if anaerobic growth was suspected during this procedure, an anaerobic culture was performed for further identification. Species-level typing of the isolated microorganisms was performed using conventional methods and the VITEK 2 Compact automated system (bioMérieux, France). Antimicrobial susceptibility testing was performed and evaluated according to the criteria of the European Committee on Antimicrobial Susceptibility Testing (EUCAST) using the VITEK 2 Compact automated system (bioMérieux, France) (17).
The Bakırköy Dr. Sadi Konuk Training Research Hospital Clinical Research Ethics Committee approved the study on December 11, 2024, with the decision number 2024-14-05. Written informed consent was waived from the participants because of the study’s retrospective design.
Statistical Analysis
Statistical Package for Social Sciences (SPSS) 21.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis. Continuous variables were expressed as mean ± standard deviation, while categorical variables were expressed as number (n) and percentage (%). When comparing continuous variables, Student’s t-test was used for normally distributed parameters and the Mann-Whitney U test for non-normally distributed parameters. Chi-square and Fisher’s exact tests were used to compare categorical parameters. A p-value of <0.05 was considered statistically significant.
Results
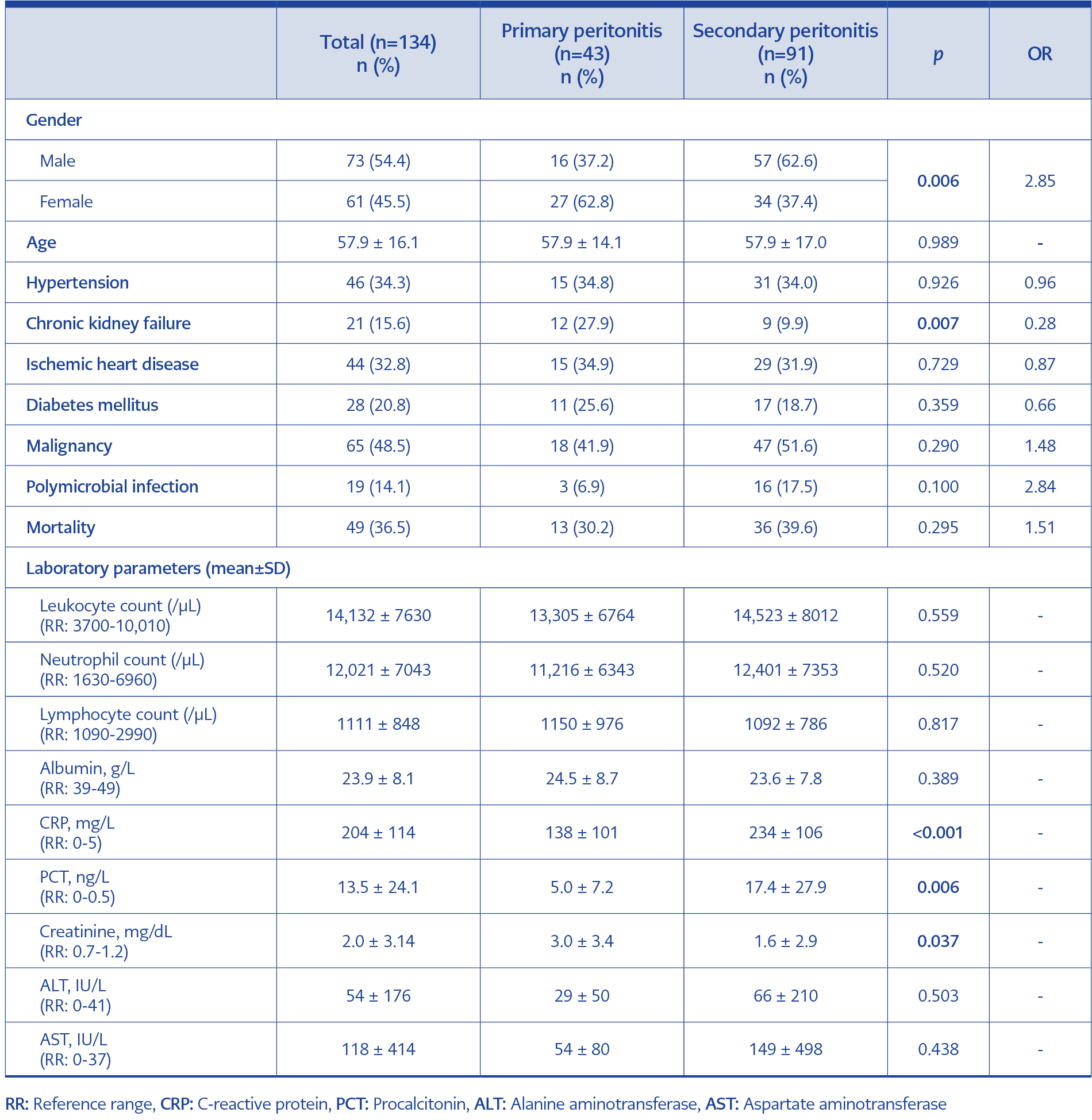
Table 1. Comparison of demographic characteristics and laboratory parameters of patients with primary and secondary peritonitis.
A total of 134 patients were included in the study. Of these patients, 54.5% (n=73) were male, and the mean age was 57.9 ± 16.1 years. Of the patients, 49.2% (n=66) had malignancy, 34.3% (n=46) had hypertension, 32.8% (n=44) had ischemic heart disease, 20.9% (n=28) had diabetes, 15.6% (n=21) had chronic renal failure, and 12.6% (n=17) had cirrhosis. Forty-three patients (32.1%) had primary peritonitis and 91 patients (67.9%) had secondary peritonitis. Of the primary peritonitis cases, 34.8% (n=15) were cirrhosis-related SBP, 25.6% (n=11) were peritoneal dialysis-related peritonitis, and 39.5% (n=17) were ascites-related peritonitis due to malignancy. Of the secondary peritonitis cases, 30.8% (n=28) were primary perforation-related, 12.1% (n=11) were post-operative perforation-related, and 57.1% (n=52) were post-operative peritonitis due to other causes. Laboratory parameters of the patients are shown in Table 1. Primary peritonitis was more common in females (62.8% vs. 37.4%, p=0.006) and in patients with chronic renal failure (27.9% vs. 9.9%, p=0.007). In addition, creatinine (3.0 ± 3.4 vs. 1.6 ± 2.9, p=0.037) was higher, CRP (138 ± 101 vs. 234 ± 106, p<0.001) and procalcitonin (5.0 ± 7.2 vs. 17.4 ± 27.9, p=0.006) were lower in primary peritonitis cases (Table 1).
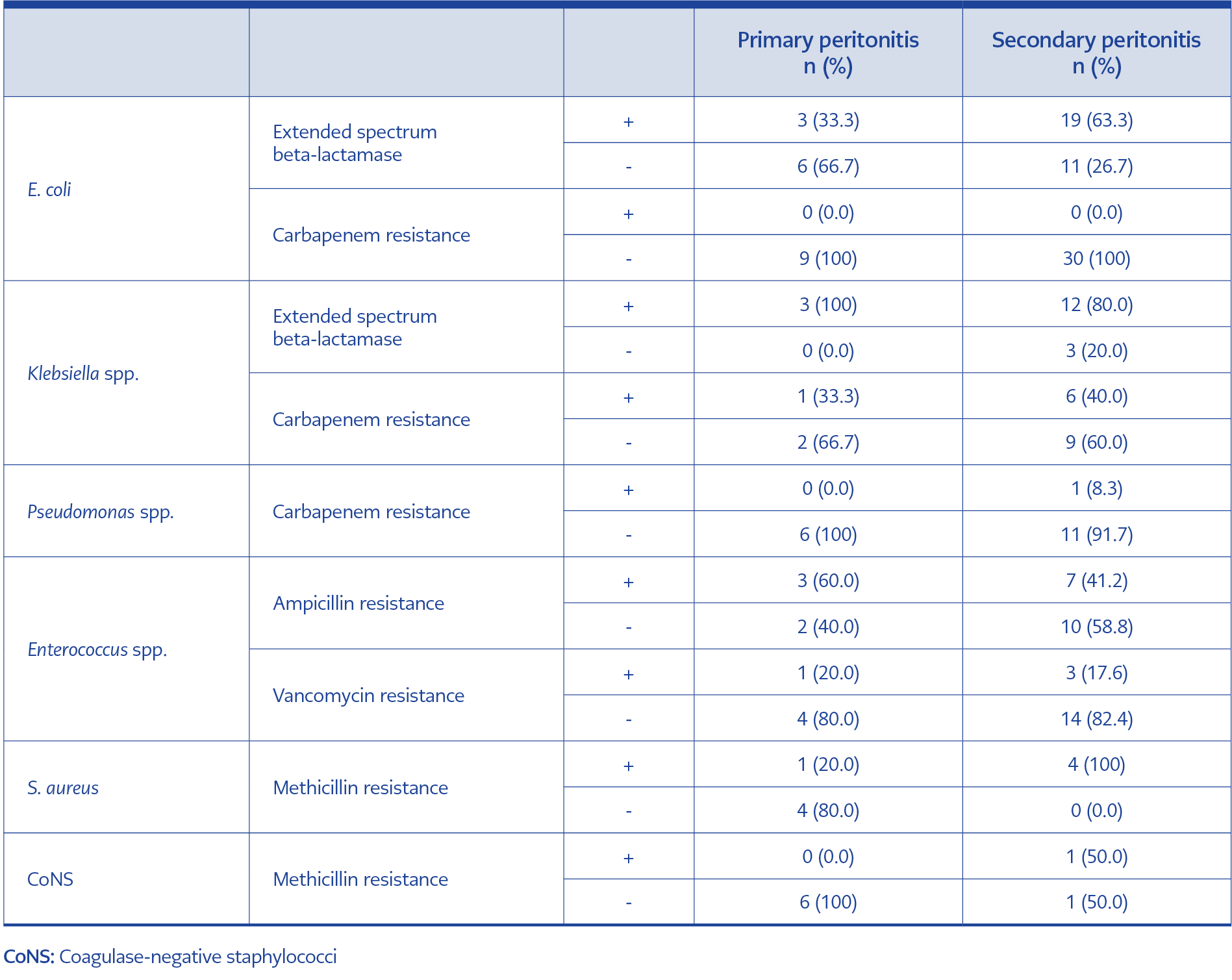
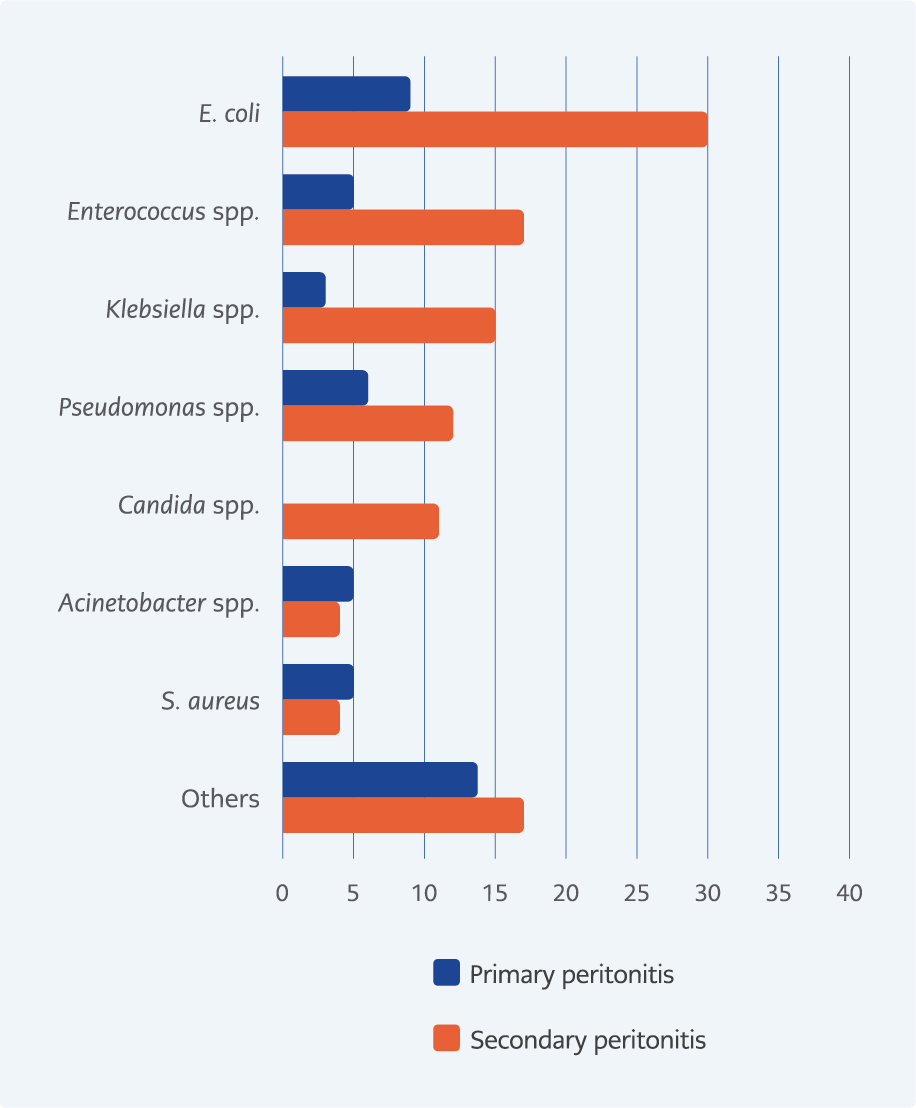
A total of 157 pathogens were isolated from 134 cases. Seven percent of primary peritonitis and 17.6% of secondary peritonitis were polymicrobial (p=0.100). The most common microorganisms detected in primary peritonitis were E. coli (19.1%, n=9/47), coagulase-negative staphylococci (CoNS) (12.7%, n=6/47), Pseudomonas spp. (12.7%, n=6/47), Enterococcus spp. (10.6%, n=5/47), and Staphylococcus aureus (10.6%, n=5/47). Thirty-three percent (n=3/9) of E. coli had extended-spectrum beta-lactamase (ESBL) production but no carbapenem resistance. All Klebsiella spp. had ESBL production, while 33% (n=1/3) had carbapenem resistance. There was no carbapenem resistance in any of the Pseudomonas spp. Sixty percent (n=3/5) of Enterococcus spp. were resistant to ampicillin and 20% (n=1/5) to vancomycin. While 20% (n=1/5) of S. aureus were resistant to methicillin, none of the CoNS were resistant to methicillin (Table 2).
The most common microorganisms detected in secondary peritonitis were E. coli (27.3%, n=30/110), Enterococcus spp. (15.4%, n=17/110), Klebsiella pneumoniae (13.6%, n=15/110), Pseudomonas spp. (10.9%, n=12/110), and Candida spp. (%10.0, n=11/110) (Figure 1). Sixty-three percent (n=19/30) of E. coli had ESBL production but no carbapenem resistance. Eighty percent (n=12/15) of Klebsiella spp. had ESBL production, and 40% (n=6/15) had carbapenem resistance. Carbapenem resistance was present in 8.3% (n=1/12) of Pseudomonas spp. Forty-one percent (n=7/17) of Enterococcus spp. were resistant to ampicillin and 17.6% (n=3/17) to vancomycin. While all S. aureus (n=4/4) were methicillin-resistant, 50% (n=1/2) of CoNS were methicillin-resistant (Table 2).
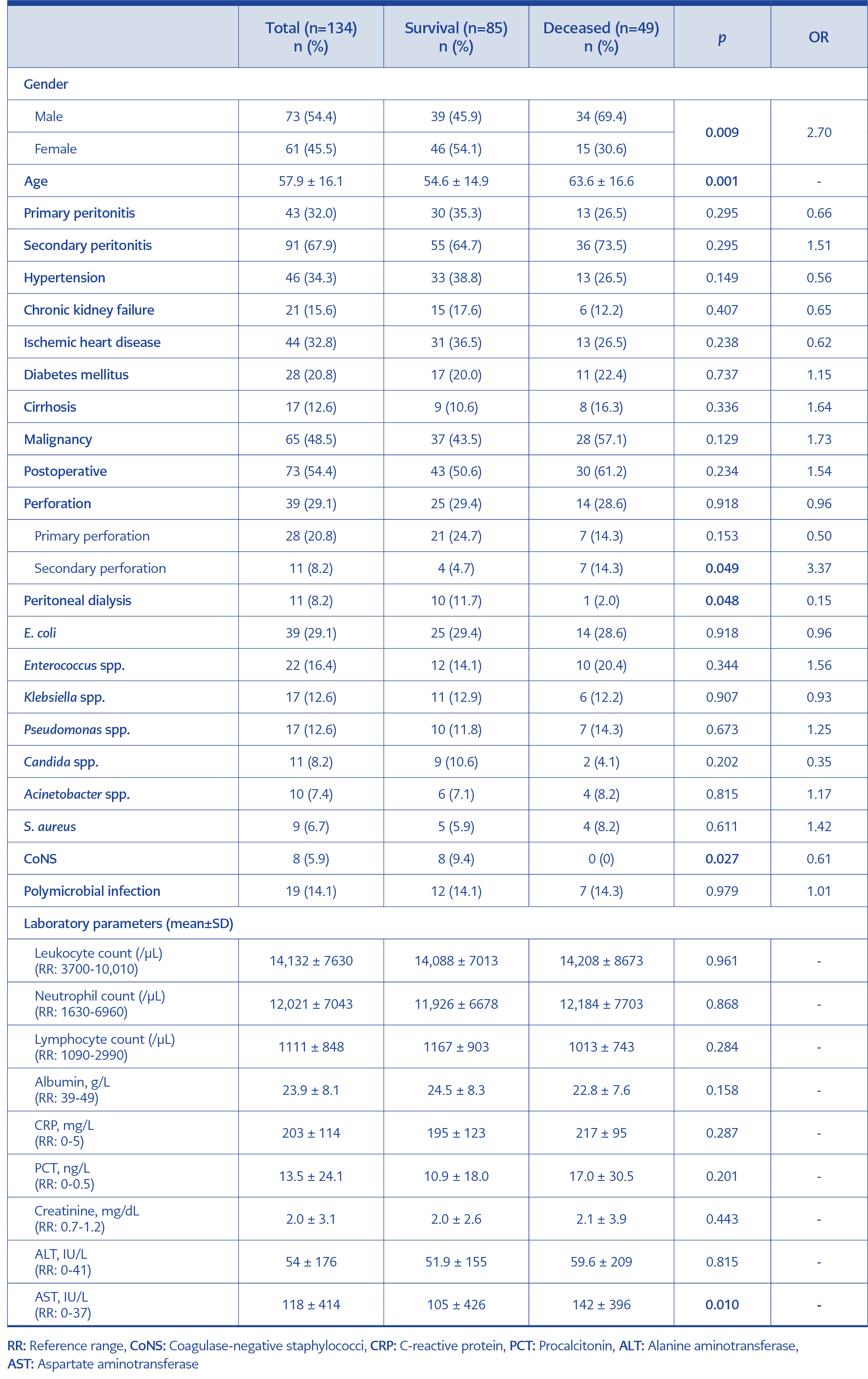
The 30-day mortality rate was 36.5% (n=49/134). Although the mortality rate in secondary peritonitis (39.5%, n=36/91) was higher than in primary peritonitis (30.2%, n=13/43), this difference was not statistically significant (p=0.295). Male gender (69.4% vs. 45.9%, p=0.009) and secondary perforation (14.3% vs. 4.7%, p=0.049) were more common in deceased patients, while peritonitis associated with peritoneal dialysis (2.0% vs. 11.7%, p=0.048) and peritonitis because of CoNS (0.0% vs. 9.4%, p=0.027) were less common in deceased patients than survivors. In addition, advanced age (63.6 ± 16.6 vs. 54.7 ± 14.9, p=0.001) and high AST levels (147 ± 412 vs. 135 ± 501, p=0.010) were associated with mortality (Table 3).
Discussion
In this study, we presented the clinical features, laboratory parameters, microbiological profile, and clinical outcomes of cases with primary and secondary peritonitis in detail. Peritonitis resulting from secondary perforation was associated with a poor prognosis, while peritonitis associated with peritoneal dialysis tended to have a favorable outcome. In addition, advanced age, male gender, and increased AST level were also indicators of poor prognosis. Enteric pathogens were the dominant microorganisms in the etiology of both types of peritonitis, while Candida spp. also had an important place (10%) in the etiology of secondary peritonitis. In addition, ESBL production was present in half of the primary peritonitis cases and two-thirds of secondary peritonitis cases due to enteric Gram-negative bacteria.
Microorganisms that cause bacterial peritonitis are generally members of the commensal intestinal microbiota (18). However, endogenous flora may change, and resistant microorganisms may be encountered more frequently because of factors such as increased use of health services, increased medical interventions, and extended life expectancy (19). Several recent studies have reported an increase in the frequency of peritonitis caused by extensively drug-resistant (XDR) bacteria (20-22). These changes in the microbiological profile and antibiotic resistance also raise concerns about the effectiveness of empirically recommended antibiotics. Therefore, knowing the possible etiological profile becomes important in choosing an empirical treatment (23).
In the study by Pimental et al. (19), the most common etiological agents of SBP were found to be E. coli (33.8%), K. pneumoniae (13.8%), Streptococcus viridans (12.3%), and S. aureus (7.7%), respectively. In addition, ESBL production was reported as 18.2% for E. coli and 33.3% for K. pneumonia. Carbapenem resistance was reported at a rate of 11% in K. pneumoniae. Liu et al. (24) reported that the most common microorganisms causing SBP were E. coli (26.2%), Staphylococcus spp. (17.1%), Enterococcus spp. (12.7%), and Streptococcus spp. (10.1%), respectively. They also reported that the frequency of Gram-positive bacteria has increased in recent years. Godefroy et al. (25) investigated the bacterial profile in secondary peritonitis and found that two-thirds of the cases were due to Gram-negative bacteria. The most frequently detected microorganisms were reported as E. coli (35.8%), Klebsiella spp. (17.0%), S. aureus (13.2%) and Citrobacter spp. (9.4%), respectively. As expected, the most common microorganism detected in primary peritonitis in our study was E. coli (20%). It was also noteworthy that one in four cases was due to Pseudomonas spp. or Acinetobacter spp. Similar to Liu et al.’s (24) study, Klebsiella spp. was less prevalent in our study, while Gram-positive bacteria came to the forefront. In secondary peritonitis cases, Gram-positive microorganisms were less common, and more than half of the cases were caused by E. coli, Klebsiella spp., and Pseudomonas spp. It was also noteworthy that Candida spp. constituted 10% of the peritonitis cases. Additionally, ESBL production in enteric bacilli was higher than in previous studies (19, 24). This situation could be caused by high antibiotic resistance rates in our country.
Mortality rates in bacterial peritonitis attacks can reach up to 30% (1). Therefore, studies investigating prognostic factors in peritonitis attacks have been conducted (24, 26-28). In the study by Liu et al. (24), the presence of upper gastrointestinal bleeding (hazard ratio [HR]=2.67, p=0.003) and increased leukocyte (HR:1.05, p=0.001), ALT (HR=1.00, p=0.025), creatinine (HR=1.50, p<0.001), total bilirubin (HR=1.06, p<0.001) and international normalized ratio (INR) (HR=1.29, p<0.001) levels were identified as mortality risk factors. Additionally, peritonitis due to XDR Acinetobacter baumannii and XDR Gram-negative bacteria has been associated with high mortality rates. Alexopoulou et al. (27) showed that the presence of infection with XDR microorganisms (HR=2.26, p=0.049), increased levels of creatinine (HR=1.12, p=0.015), and INR (HR=1.55, p=0.011) were associated with poor prognosis. In another study, the presence of septic shock (odds ratio [OR]=20.2, p<0.001), advanced age (OR=1.08, p=0.001), elevated INR (OR=9.50, p=0.007), and long-standing signs of peritonitis (OR=3.56, p=0.020) were associated with mortality (28). In our study, 30% of primary peritonitis cases and 39% of secondary peritonitis cases died within 30 days. This relatively low mortality rate in primary peritonitis was because of the higher survival rates of peritoneal dialysis-related peritonitis (90.9%, n=10/11). However, the presence of secondary perforation, advanced age, male gender, and high AST level were associated with poor prognosis.
Our study has some limitations. First, the results cannot be generalized because it was conducted in a single center. Second, there are limitations inherent to its retrospective design. Third, patient symptoms and results of biochemical analysis of peritoneal fluid were not evaluated because of incomplete patient data. Nevertheless, we analyzed the laboratory parameters and microbiological profile in detail, along with the resistance patterns.
This study highlights the importance of demographic characteristics, clinical features, and laboratory parameters for clinical outcomes in patients with peritonitis. Patients with secondary perforation-related peritonitis require close monitoring for clinical changes. Gram-positive bacteria and sensitive enteric bacilli for primary peritonitis and ESBL-producing Gram-negative bacteria for secondary peritonitis should be included in empirical treatment selection. Additionally, we recommend considering antifungal agents for severely ill patients with secondary peritonitis. In conclusion, an individualized treatment approach is essential for the clinical management of peritonitis. Prospective studies with larger patient groups will contribute to our findings and lead to more precise treatment strategies.