Introduction
Invasive Candida infections have increased significantly in recent years due to various risk factors, including invasive procedures, vascular catheterization, intra-abdominal surgery, prolonged use of broad-spectrum antibiotics, immunosuppressive medications, hemodialysis, total parenteral nutrition (TPN), and extended intensive care unit (ICU) stays (1, 2). Candida, one of the top three nosocomial bloodstream infections, is particularly common in ICUs and is associated with high mortality rates (3). A multicenter study across 23 ICUs in nine European countries reported a 30-day mortality rate of 42% for candidemia (4, 5).
Candidemia is a critical condition often encountered in ICUs, with high rates of morbidity and mortality (4-7). Candida species colonize many ICU patients, and candidemia can develop in approximately one-third of them, particularly those with progressive colonization or who have undergone major abdominal surgery (1, 8). Early detection of candidemia is challenging, as microbiological documentation frequently arrives late, leading to delays in diagnosis and treatment, which are associated with increased mortality (9). Prolonged hospital stays and significant healthcare costs further underscore the importance of timely intervention (7, 10).
Blood cultures are the gold standard for diagnosing candidemia but have significant limitations (11). They require at least three days to detect growth and an additional two days for identification, making them too slow to manage critically ill ICU patients effectively. Candida is isolated from blood cultures at a rate of 50-70% and late (12). Invasive candidiasis diagnosis is easily made in patients with positive blood cultures, but the low sensitivity of blood cultures means that some patients with systemic infections may be missed. Faster detection of yeasts in blood cultures and the development of new non-culture-based techniques are two of the most important research areas in the literature. Recent guidelines recommend using Candida scoring systems for early detection of infections and prompt initiation of antifungal treatment (13). The ‘Candida score’ developed by León et al. is commonly applied to non-neutropenic ICU patients, demonstrating a sensitivity of 81% and specificity of 74% for scores above 2.5 (14). However, while this score is effective for surgical ICU patients, it may not adequately identify candidemia in patients with non-surgical issues, highlighting a significant limitation of the existing score.
Early diagnosis and treatment of candidemia are crucial for improving survival rates in ICU patients (1, 7). Because of the low sensitivity of serological tests, there is an urgent need for faster molecular diagnostic techniques to provide results within hours or minutes (15). However, the lack of a well-established molecular diagnostic method complicates the effective management of candidemia, leading to significant clinical and economic burdens (10).
This prospective observational study aimed to evaluate risk factors in critically ill ICU patients, create a unique Cerrahpaşa Candida score, and develop a Candida real-time polymerase chain reaction (PCR) assay for the early diagnosis of candidemia in ICU settings.
Materials and Methods
Patients and Study Design
Retrospective case-control study
This study was conducted in three phases. In the first phase, we performed a retrospective case-control study involving 100 ICU patients, including 50 candidemia cases and 50 controls (patients without candidemia) at Cerrahpaşa Medical Faculty between January 2017 and December 2018. Cases and controls were matched in a 1:1 ratio based on age, sex, and candidemia risk factors to minimize confounding variables. Patients younger than 18 years of age or with neutropenia were excluded from the study. We assessed each patient for the following risk factors: recent hospitalization within the last three months, prolonged antibiotic therapy (more than one week), immunosuppressive drug use, malignancy, sepsis, intra-abdominal infections, Candida colonization at two or more sites, extended ICU stay, elevated C-reactive protein (CRP) and procalcitonin levels, TPN, mechanical ventilation, open decubitus ulcers, history of transplantation, acute kidney injury (AKI), central venous catheter (CVC) placement, and major surgery. Following ethical committee approval, patient data were extracted from hospital records, and informed consent was waived.
The İstanbul University-Cerrahpaşa Institutional Review Board approved the study on September 10, 2018 with the decision number 64414572-604.01.01-53634.
Prospective cross-sectional study
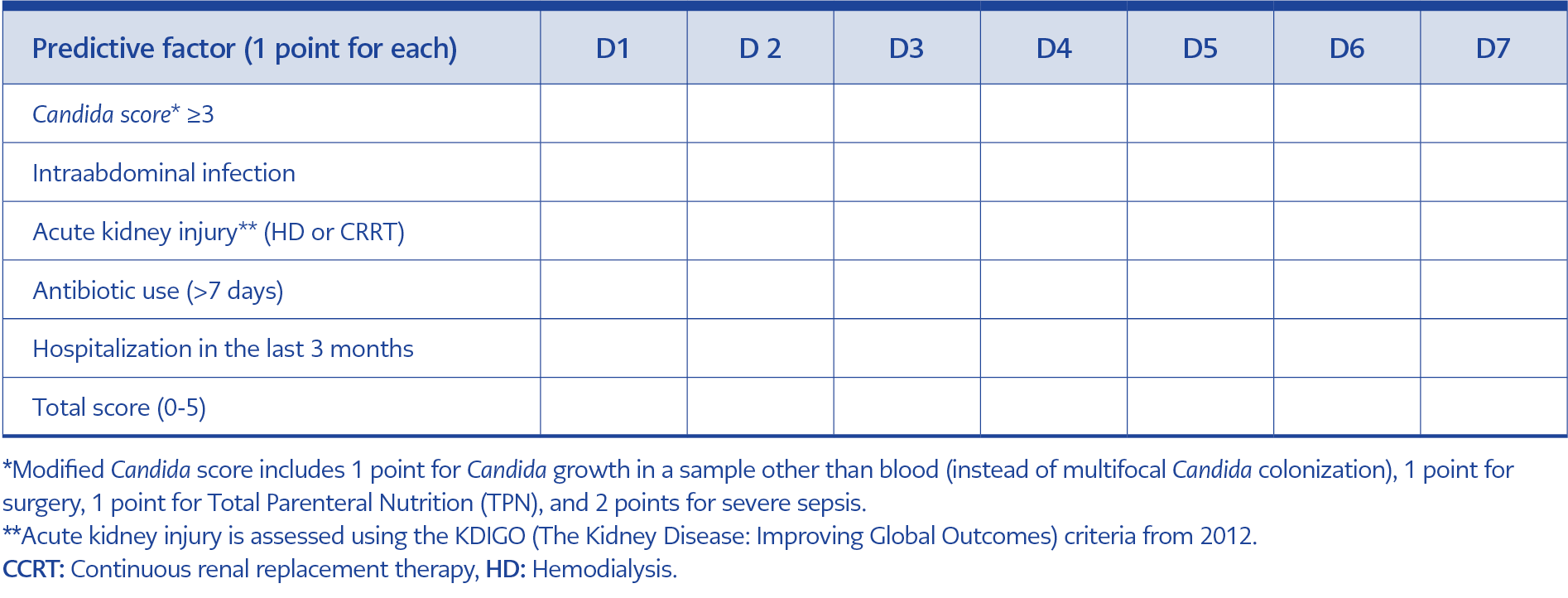
In the second phase, data from the retrospective case-control study were used to develop the Cerrahpaşa Candida score, a predictive tool for candidemia risk in ICU patients. This prospective cross-sectional study was conducted at İstanbul University-Cerrahpaşa between December 2020 and January 2021 to evaluate the clinical efficacy of this scoring system (Table 1). Informed consent was obtained from the patients or their legal representatives before enrollment. Seventy-five ICU patients hospitalized for more than 72 hours were included. Upon ICU admission, patients were monitored for the first 72 hours and then daily after that. Patients were followed until ICU discharge or until the development of candidemia. The Cerrahpaşa Candida score was recorded daily, and the highest score during follow-up was used for patients who did not develop candidemia. The score on the day of diagnosis was recorded for patients who developed candidemia.
Real-Time PCR Assay Development
In the third phase, we developed and tested a real-time PCR assay targeting specific Candida gene regions from whole blood samples. This molecular diagnostic tool was designed to allow early detection of candidemia in high-risk ICU patients.
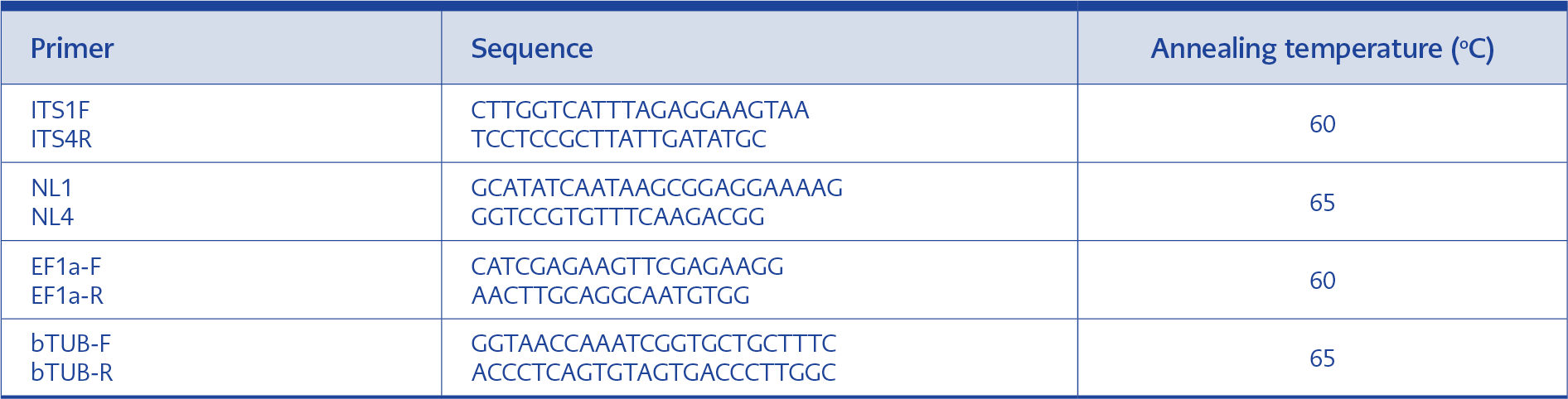
Candida DNA in whole blood was detected using a single EvaGreen-based real-time PCR assay, targeting the internal transcribed spacer (ITS), D1/D2, EF1α, and tubulin gene regions. The PCR analysis was performed at the Molecular Microbiology Laboratory at İstanbul University-Cerrahpaşa.
Blood culture isolates of Candida albicans and Candida parapsilosis were identified by conventional methods (germ tube test, CHROMagar, cornmeal agar, API 20C tests) and confirmed by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS). The isolates were prepared in sterile saline with concentrations adjusted to 1 McFarland, using 24-hour cultures on Sabouraud dextrose agar (SDA). Serial 1:10 dilutions were prepared, and cell counts were determined using Thoma slides. Standard blood samples were prepared by mixing Candida dilutions with ethylenediaminetetraacetic acid (EDTA) blood samples, producing concentrations of 10,000, 1000, 100, and 10 cells per mL.
Blood samples were mixed with the buffer EL (erythrocyte lysis buffer) (Qiagen GmbH, Germany) at a 1:3 ratio, and erythrocytes were lysed by gentle shaking for five minutes at room temperature. Cell debris was removed by centrifugation at 14,000 rpm for two minutes, and the pellet was washed with 1 mL of DNase/RNase-free water, resuspended in 400 µL of resuspension buffer, and extracted using a commercial kit (Ribospin, GeneAll Biotechnology Co., Ltd., South Korea).
DNA extraction involved incubation at 65°C for 15 minutes, followed by lysis at 90°C for 10 minutes, according to the manufacturer’s instructions. Candida DNA was then detected using the EvaGreen-based real-time PCR targeting the ITS, D1/D2, EF1α, and tubulin regions. Primer pairs for the real-time PCR assays are detailed in Table 2. Real-time PCR was performed using a CFX96 Touch Real-Time PCR Detection System (BioRad Laboratories Inc., USA).
Melting Curve Analysis
Post-amplification, melting curve analysis was used to assess the specificity of the amplicons, focusing on the ITS and D1/D2 gene regions. This analysis distinguished different Candida species based on their unique DNA melting points.
Definitions
Candidemia was defined as a bloodstream infection caused by Candida species, diagnosed by positive blood culture.
The classical Candida score was modified by replacing the multifocal Candida colonization criterion with Candida growth in non-blood specimens. In this modified Candida score, 1 point was assigned for Candida growth in any non-blood sample, 1 point for surgical intervention, 1 point for TPN administration, and 2 points for severe sepsis.
Cerrahpaşa Candida score is defined as a clinical scoring system designed to predict the risk of candidemia in ICU patients. It assigned 1 point for each of the following criteria: a modified Candida score greater than 3, the presence of intra-abdominal infection, AKI requiring continuous renal replacement therapy (CRRT) or hemodialysis, antibiotic use for more than seven days, and a history of hospitalization within the past three months (Table 1).
The detection limit was defined as the lowest quantity of fungal cells reliably detected by the PCR assay, set at 10 CFU/mL in this study.
Statistical Analysis
Descriptive statistics were used to summarize the data, including mean, standard deviation, median, minimum, maximum, frequency, and ratio values. The distribution of variables was assessed using the Kolmogorov-Smirnov test. Quantitative independent data were analyzed using the independent sample t-test and the Mann-Whitney U test. For qualitative independent data, the Chi-square test was employed, and the Fisher’s exact test was used when the conditions for the Chi-square test were not met. The effect levels were examined through univariate and multivariate logistic regression analysis. The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 26.0 (IBM Corp., Armonk, NY, USA).
Results
Retrospective Case-Control Study
Between January 2017 and December 2018, a retrospective analysis was conducted on 100 ICU patients, including 50 patients with candidemia (cases) and 50 patients without candidemia (controls). The median age of these patients was 63 years (interquartile range [IQR]=19-96 years). Among them, 70 were in the general ICU, 22 in the emergency ICU, and 8 in the cardiovascular surgery ICU. The mortality rate in this group was 70%.
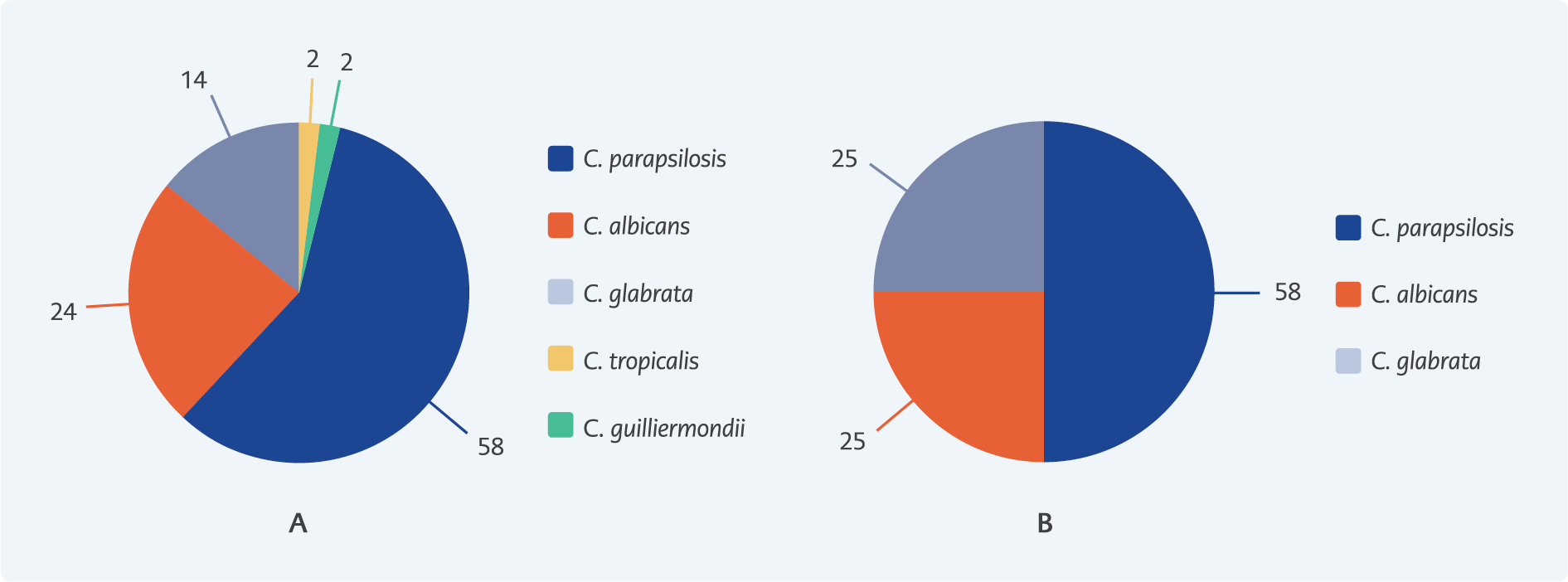
Figure 1. Distribution of Candida species detected in blood cultures (%). (A) Retrospective analysis and (B) Prospective analysis.
In 50 cases of ICU candidemia, the distribution of Candida species was as follows: C. parapsilosis in 58% (29 patients), C. albicans in 24% (12 patients), Candida glabrata in 14% (7 patients), Candida tropicalis in 2% (1 patient), and Candida guilliermondii in 2% (1 patient). Notably, non-albicans Candida species were more prevalent, representing 76% of the cases, as shown in Figure 1A.
Among the 50 candidemia cases, 49 patients (98%) had sepsis, 48 (96%) had a history of hospitalization in the last three months, 48 (96%) had used antibiotics for more than one week, 31 (62%) had undergone major surgery, 29 (58%) were on TPN, and 23 (46%) had intra-abdominal infections.
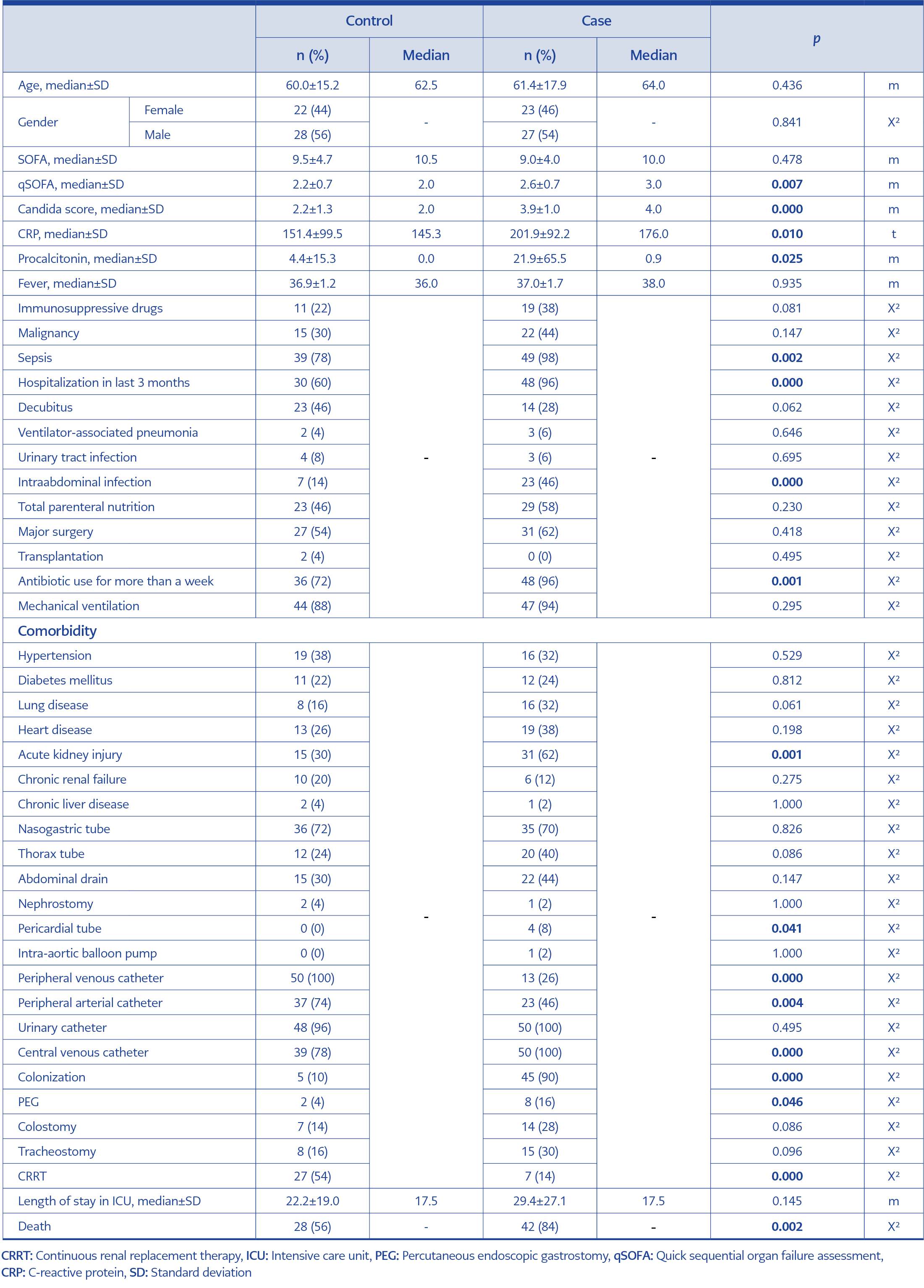
When comparing the case and control groups, the case group had significantly higher rates of sepsis, hospitalization in the last three months, elevated CRP and procalcitonin levels, prolonged antibiotic use (over one week), AKI, CVC use, pericardial tube placement, percutaneous endoscopic gastrostomy (PEG) rate, colonization, and mortality (p<0.05) (Table 3).
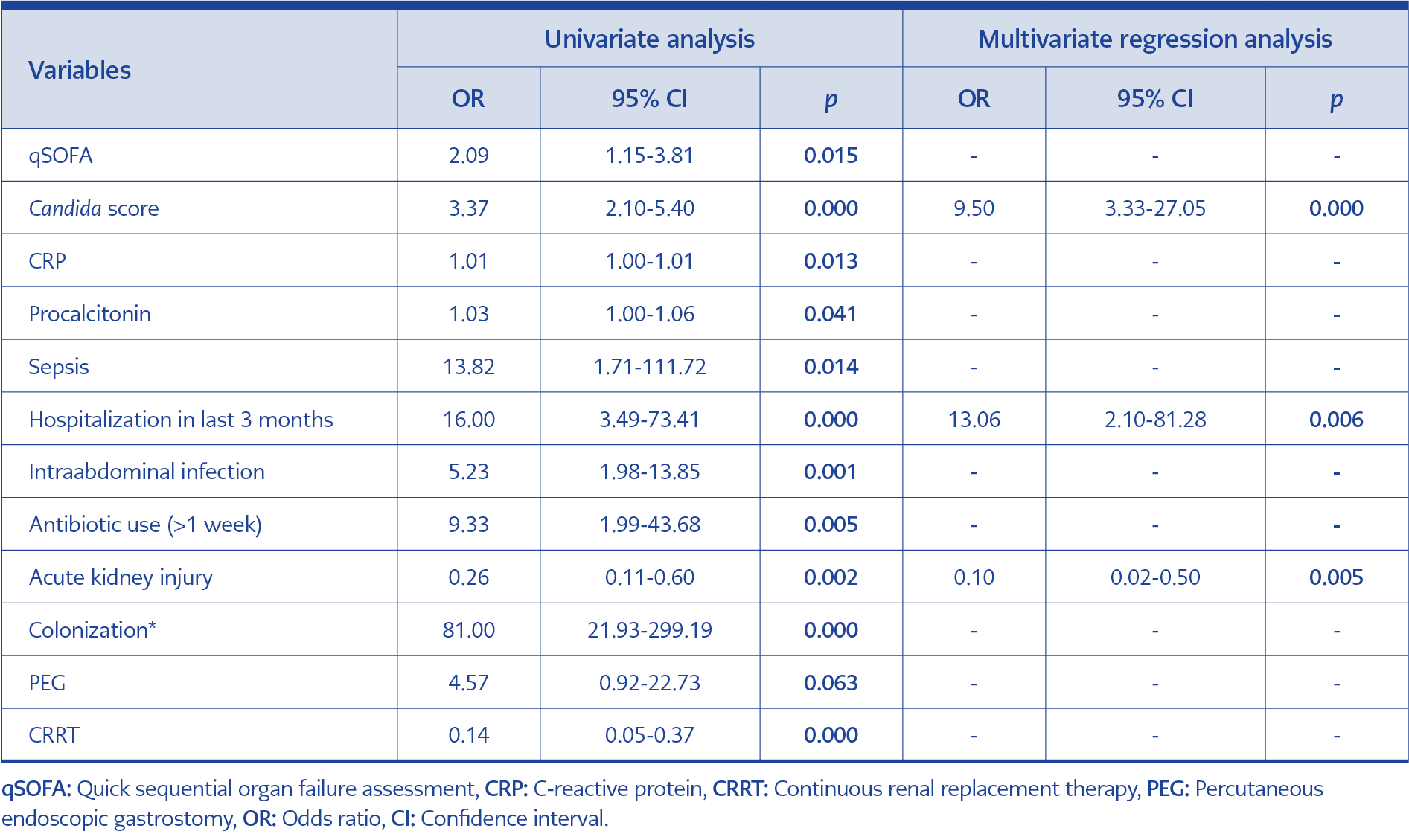
Table 4. Univariate and multivariate logistic regression analysis for independent risk factors of candidemia.
In the univariate analysis, quick Sequential Organ Failure Assessment (qSOFA), “modified Candida score,” CRP, procalcitonin, sepsis, recent hospitalization (within the last three months), history of intra-abdominal infection, prolonged antibiotic use, AKI, peripheral venous catheter use, colonization, PEG, and CRRT significantly differentiated between case and control groups (p<0.05) (Table 4). In the multivariate reduced model, the “modified Candida score,” hospitalization within the last three months, and AKI were identified as significant independent predictors of candidemia (p<0.05) (Table 4).
Prospective Cross-Sectional Study
Between December 1, 2020, and January 10, 2021, 75 ICU patients who had been hospitalized for more than 72 hours were prospectively monitored. The median age in this group was 68 years (IQR=35-97 years). Of these patients, 53 were in the general ICU, 11 in the emergency ICU, and 11 in the neurosurgery ICU. The mortality rate was 57.3%, with a median follow-up period of 9.1 days (IQR=4-37 days).
Four cases of candidemia were observed among the 75 ICU patients. The distribution of Candida species in these cases was as follows: C. parapsilosis in 50% (2 patients), C. albicans in 25% (1 patient), C. glabrata in 25% (1 patient). Notably, non-albicans Candida species were more prevalent, accounting for 75% of the cases, as shown in Figure 1B.
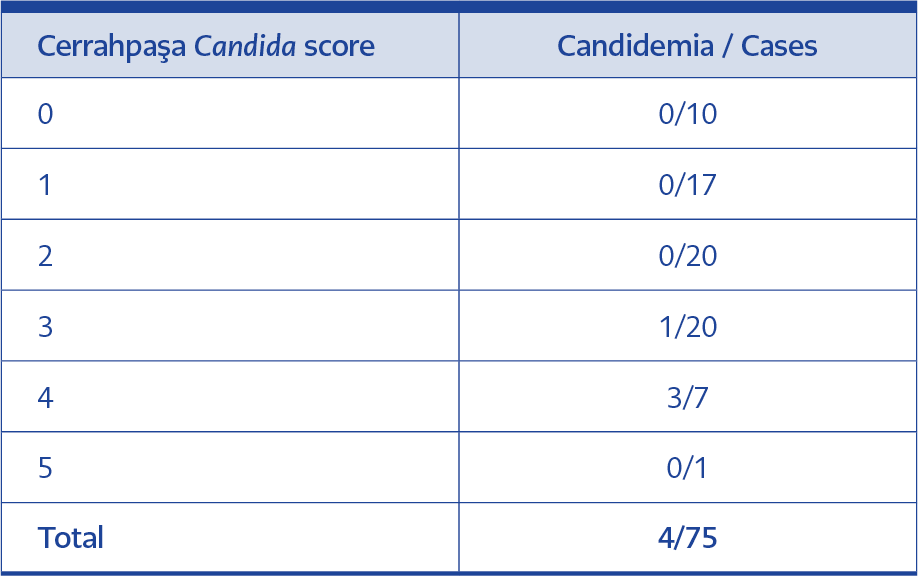
A Candida scoring system specific to our hospital was developed using risk factors identified in logistic regression analysis, such as intra-abdominal infection and antibiotic use for over seven days, frequently observed in ICU candidemia cases. The Candida score was modified to include the detection of Candida growth in any non-blood sample as 1 point, severe sepsis as 2 points, surgery as 1 point, and TPN administration as 1 point. The “Cerrahpaşa Candida score” and the number of candidemia cases are presented in Table 5.
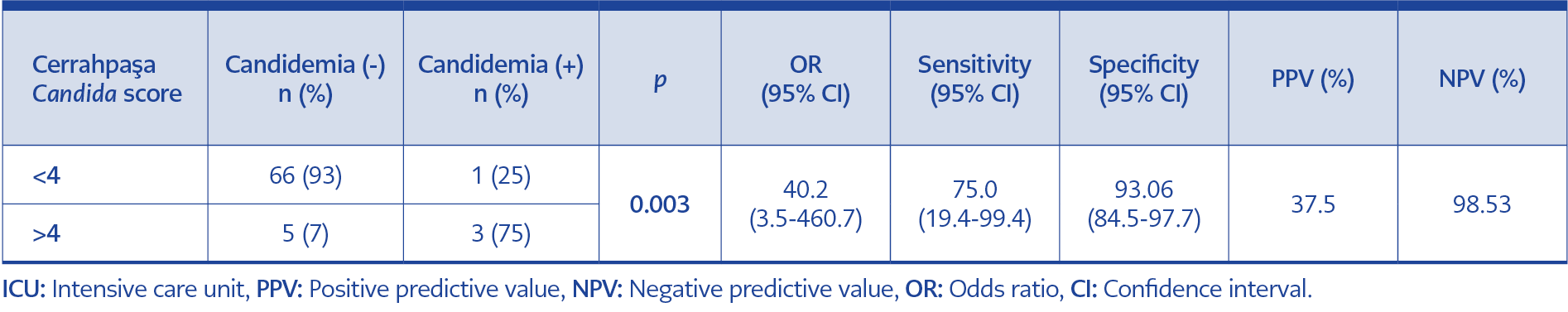
Table 6. Candidemia risk in ICU patients with a Cerrahpaşa Candida score of 4 or higher in the prospective cohort.
During prospective follow-up, no invasive candidiasis was detected in patients with a Cerrahpaşa Candida score below 3 points. A score of 4 or above was determined to indicate a significant risk for candidemia, with a statistically significant correlation between the Cerrahpaşa Candida score and candidemia (Fisher’s exact p<0.05). The risk of developing candidemia was shown to be 40.2 times higher in patients with a Cerrahpaşa Candida score of 4 or above. The sensitivity and specificity of the Cerrahpaşa Candida score for >4 points were 75% and 93%, respectively. The negative predictive value (NPV) and positive predictive value (PPV) for a score of 4 or more were 98.53% and 37.5%, respectively (Table 6).
Development of an experimental PCR-based rapid diagnostic test
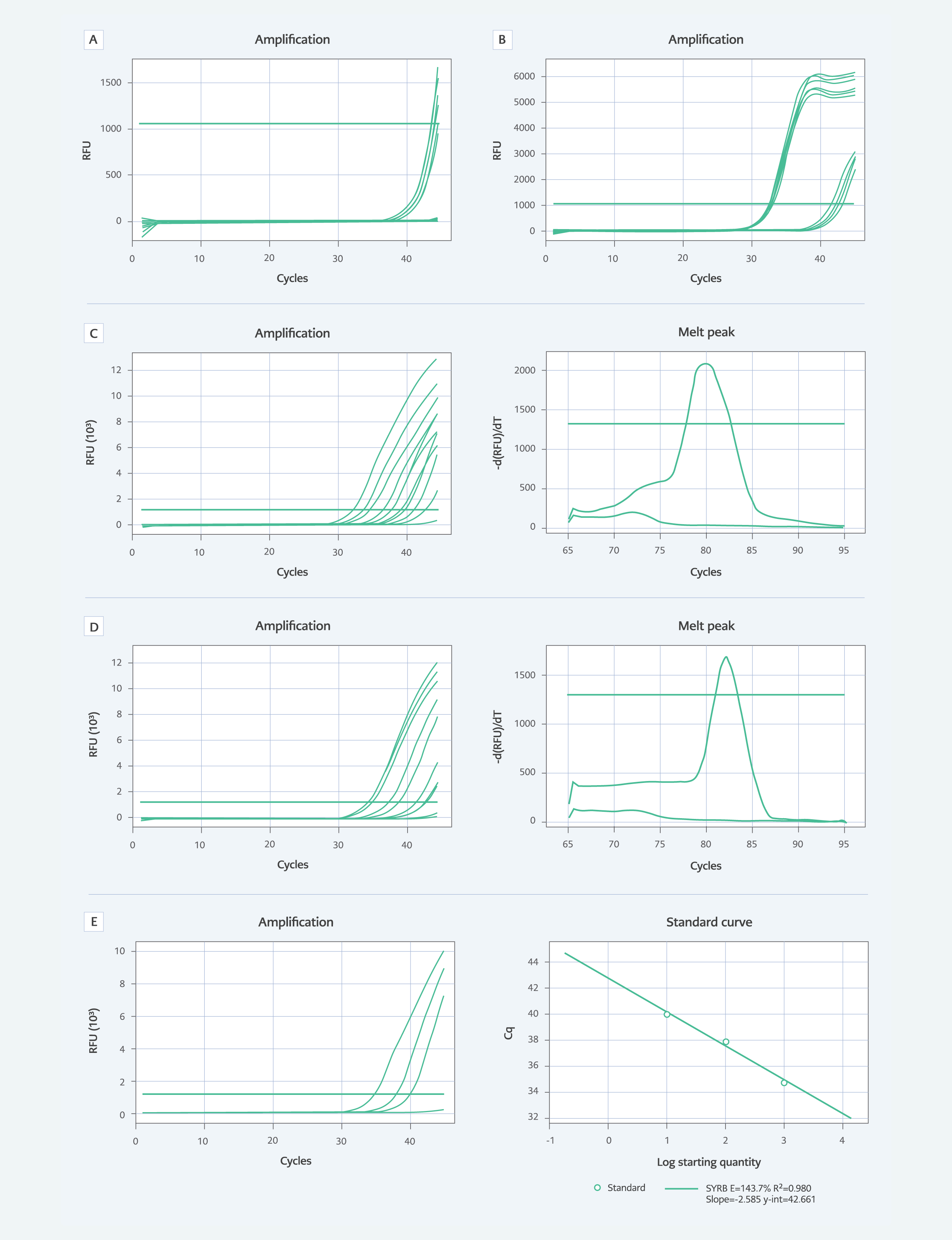
Figure 2.1. Amplification and melting curve analyses. Non-specific and inadequate amplification curves for (A) Tubulin and (B) EF1a gene regions; Amplification and melting curve analyses for the ITS (C) and D1/D2 (D) regions; Amplification curves for ITS with samples containing 1000, 100, 10, and 1 Candida cells, along with the standard curve for C. albicans (E).
The PCR assay was part of the experimental study and was not used for scoring or clinical diagnostic evaluation. Specific primer pairs and EvaGreen® dye (Biotium Inc., USA) were used to differentiate between C. albicans and C. parapsilosis isolates through melting curve analysis of real-time PCR amplicons. The PCR test demonstrated a detection limit of 10 colony-forming units (CFU)/mL. When examining the real-time PCR amplification curves, it was observed that the curves for the tubulin and EF1a gene regions were unsuitable for the study due to non-specific and insufficient amplifications, requiring further optimization. These amplification curves for tubulin and EF1a are shown in Figure 2 (A and B).
Positive amplification was detected in blood samples containing 1000, 100, and 10 Candida cells with primers targeting the ITS region, but no amplification was detected in blood containing 1 Candida cell. Thus, the detection limit of the test was determined to be 10 cells/mL. The specificity of the amplicon was confirmed by melting curve analysis, as shown in Figure 2 (C and E).
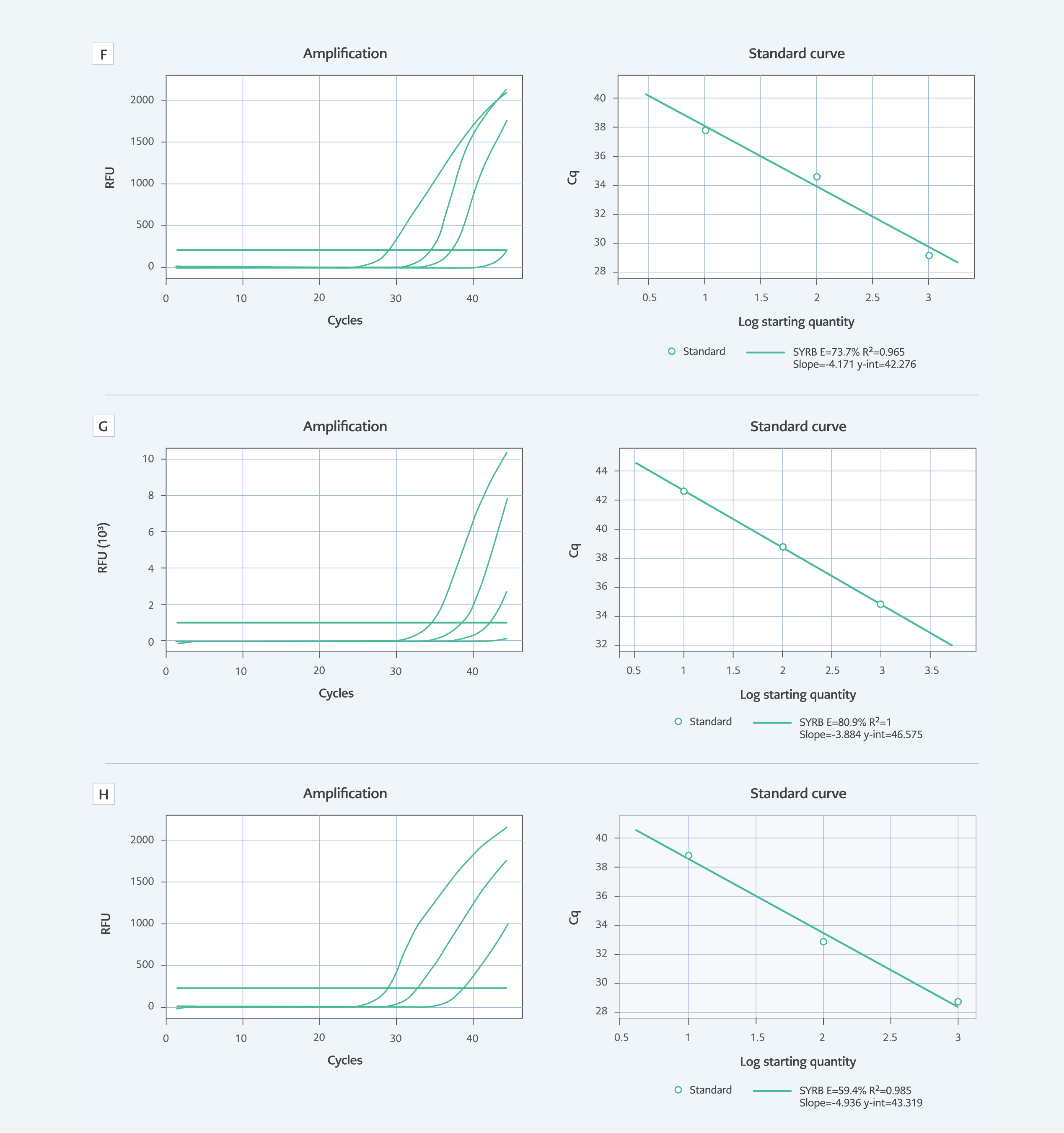
Figure 2.2. Amplification and melting curve analyses. Non-specific and inadequate amplification curves for C. parapsilosis (F); Amplification curves for D1/D2 with samples containing 1000, 100, 10, and 1 Candida cells, along with the standard curve for C. albicans (G) and C. parapsilosis (H).
Similarly, positive amplification was detected in blood samples containing 1000, 100, and 10 Candida cells with primers targeting the D1/D2 region, with no amplification in blood containing 1 Candida cell. This also established the detection limit at 10 cells/mL. The specificity of the amplicon was confirmed by melting curve analysis, as illustrated in Figure 2 (D and F).
The slope of the standard curve, drawn quantitatively, was found to be -2.585 for C. albicans with a fit of 0.960 and a cutoff point of 42.661, and -4.171 for C. parapsilosis with a fit of 0.965 and a cutoff point of 42.276. The amplification curves for samples containing 1000, 100, 10, and 1 Candida cells, along with the standard curve, are presented in Figure 2 (G and H).
The slope of the standard curve, drawn quantitatively, was found to be -3.884 for C. albicans with a fit of 1.000 and a cutoff point of 46.575, and -4.936 for C. parapsilosis with a fit of 0.986 and a cutoff point of 43.319. Figure 2 shows the amplification curves for samples containing 1000, 100, 10, and 1 Candida cells, along with the standard curve.
Discussion
Candidemia, a critical condition prevalent in ICUs, remains a significant cause of morbidity and mortality (4, 5). This study highlights the challenges and advancements in diagnosing and managing candidemia. Our findings suggest that candidemia is common among ICU patients, with a high prevalence of Candida colonization and a significant mortality rate. We identified several key risk factors for candidemia, including sepsis, intra-abdominal infections, hospitalization within the last three months, prolonged antibiotic use (>1 week), Candida colonization, PEG, CVC, and AKI. These findings are consistent with established risk factors in the literature and underscore the importance of closely monitoring high-risk ICU patients (1, 7, 9, 16).
In this study, we observed a notable shift in the distribution of Candida species among ICU patients, with C. parapsilosis being the predominant isolate (58%), followed by C. albicans (24%). This shift reflects a broader trend observed in other studies (4, 6), where non-albicans Candida species are becoming increasingly prevalent. The high incidence of C. parapsilosis in our study may be related to factors such as the use of TPN, CVC, recent surgery, and unresolved intra-abdominal infections in the surgical ICU.
Effective early detection of candidemia is crucial, as delays in diagnosis and treatment are linked to increased mortality rates. Traditional microbiological methods often detect candidemia late in the course of the infection, highlighting the urgent need for Candida scoring systems and more rapid diagnostic techniques (13). In this study, we evaluated the Cerrahpaşa Candida score, a scoring system designed to assist in early diagnosis and treatment decision-making. This score was developed by a multivariate model using risk factors such as intra-abdominal infection, antibiotic use for more than 7 days, hospitalization within the last 3 months, and AKI development. In the prospective follow-up, no cases of invasive candidiasis were detected in patients with a Cerrahpaşa Candida score below 3. Of the eight patients with a score of 4 or higher, three developed candidemia, underscoring the importance of this score in assessing candidemia risk. A statistically significant difference (p<0.05) was observed between the Cerrahpaşa Candida score and candidemia.
Our findings demonstrate that the Cerrahpaşa Candida score, particularly with a cutoff value of 4, effectively identifies patients at high risk for candidemia. The Cerrahpaşa Candida score accurately identified 94% of patients with positive blood cultures as having a score greater than 2.5. Cerrahpaşa Candida score exhibited a high negative predictive value of 98.53%. This makes the Cerrahpaşa Candida score a valuable tool for minimizing unnecessary antifungal use and guiding early intervention.
Our findings align with those of León et al., who emphasized the importance of early diagnosis and treatment in invasive candidiasis (14). They found that a Candida score greater than 2.5 was associated with an 81% sensitivity and 74% specificity for predicting infection. In our study, the Cerrahpaşa Candida score at a cutoff of 4 showed a sensitivity of 75% and a specificity of 93%, further supporting the use of such scoring systems to guide early intervention and improve patient outcomes. Major guidelines support using Candida scoring systems for early diagnosis and prompt initiation of antifungal therapy (13, 17-20).
A prospective study by León et al. in 2009 found a statistically significant association between invasive candidiasis and Candida score, similar to our findings (21). Their 2006 study (14) reported a sensitivity and specificity of 81% and 74%, respectively, for a Candida score cutoff of 2.5 points, with the risk of invasive candidiasis being 7.75 times higher in patients with a Candida score >2.5 points. In our study, the Cerrahpaşa Candida score cutoff of 4 had a sensitivity of 75% and a specificity of 93%, with the risk of invasive candidiasis being 40.2 times higher for those with a score of 4 or higher (Table 6).
Our study also addressed the limitations of conventional blood cultures, which often require several days to yield results and can delay the initiation of appropriate treatment. The delay in diagnosis and treatment is associated with higher mortality rates, underscoring the need for more rapid diagnostic methods. Empirical antifungal therapy is commonly initiated in ICU patients with suspected invasive candidiasis to reduce mortality. However, the overuse of antifungal drugs is a concern, making the development of reliable bedside scoring systems and early diagnostic tests crucial. Despite the growing use of biomarkers such as mannan, anti-mannan, and 1,3-β-D-glucan, PCR remains a promising tool for early diagnosis and treatment (11).
To address this, we developed a single EvaGreen-based real-time PCR test for the rapid detection of Candida species in blood samples. Although the test achieved a detection limit of 10 CFU/mL, it was not effective in detecting very low fungal burdens (1 Candida cell). The use of whole blood samples for PCR testing enhanced the method’s specificity, as it allows for the detection of intact Candida cells, which is advantageous compared to serum or plasma samples. This approach improves the accuracy of the PCR test, especially in patients undergoing antifungal therapy, although interpreting positive results can still be challenging.
Additionally, our PCR approach targeted the ITS and D1/D2 regions of the fungal ribosomal DNA (rDNA), which are widely recognized for their utility in identifying and distinguishing between different Candida species (22). The ITS region is known for its high variability among species, making it a valuable marker for species-level identification (22). Meanwhile, the D1/D2 domains of the large subunit rDNA are more conserved but still provide sufficient variation to differentiate closely related species. By targeting both ITS and D1/D2 regions, our PCR assay enhances species-specific detection, contributing to more accurate and timely diagnosis, especially in cases where rapid identification is crucial for guiding antifungal therapy.
In other studies, similar to our research, melting curve analysis of ITS sequences was performed, and each amplicon was found to have a specific melting point (23, 24). This molecular method could serve as a potential diagnostic tool for the rapid detection of Candida species, facilitating early and targeted treatment for patients with invasive candidiasis.
Our findings align with previous research that utilized real-time PCR and melting curve analysis to detect invasive yeast species, establishing specific melting points for each amplicon (24, 25). However, our test’s detection limit of 10 CFU/mL is higher than those reported by some other studies. For instance, while one study acknowledged a detection limit of 10 CFU/mL as adequate (26), others have reported lower limits, such as 5 CFU/mL, which are considered more representative of fungal sepsis conditions (27, 28). This discrepancy highlights the variability in sensitivity among different testing methods.
Several limitations of our study should be noted. First, our reliance on blood cultures as the definitive diagnostic criterion may not fully capture all cases of candidemia due to their delayed detection capabilities. Second, the study did not include serological testing due to issues with standardization and economic constraints. These factors may impact the overall diagnostic accuracy and generalizability of our findings. Third, the detection limit of the PCR test at 10 CFU/mL restricts its ability to identify very low fungal burdens. Fourth, the ongoing COVID-19 pandemic has influenced patient demographics, treatment practices, and hospital workflows, which may have affected the prevalence and outcomes of candidemia during the study period. Fifth, our focus on C. albicans and C. parapsilosis in our PCR assay, due to their high prevalence in both our study and other studies from Turkey, may limit the comprehensiveness of our findings by excluding other significant species, such as C. glabrata and C. tropicalis. Nonetheless, although we did not conduct a cost analysis, the Cerrahpaşa Candida score and PCR test developed in this study offer a more financially accessible alternative to existing rapid diagnostic options like the T2 Candida panel, which costs over 200 USD per test and makes it less accessible in low- to middle-income countries (17, 29). Our methods are easy to perform and appear to be beneficial for the early detection of candidemia, especially in resource-limited settings (30).
In conclusion, the increasing prevalence of non-albicans Candida species and the identification of key risk factors for candidemia emphasize the need for improved diagnostic and therapeutic strategies in the ICU setting. The Cerrahpaşa Candida score and the developed PCR test offer promising approaches for early detection and management of candidemia. Further multicenter studies with larger patient populations are needed to validate these findings and refine diagnostic and treatment protocols.