Introduction
The development of a vaccine was a big step in the fight against COVID-19. However, with the introduction of vaccines in a short time, there were many people in society and among healthcare workers (HCWs) who did not want to get vaccinated (1, 2, 3).
Although efficacy levels have changed with newly emerging variants, vaccination has remained an effective solution for controlling the disease and preventing deaths. It was difficult to comprehend why people refused vaccines when there was no effective treatment and deaths occurred even at young ages (4, 5). Despite more information about the disease and vaccines, many HCWs hesitated or refused to receive vaccines (2, 6). Although the number of hesitant HCWs decreased in time, some HCWs insisted on vaccine refusal and they lost their jobs or lives (7, 8).
The attitudes of HCWs have a significant impact on society and patients (9). In this study, we aimed to investigate vaccine hesitancy rates and reasons among HCWs by conducting two surveys at different times to contribute to developing strategies for increasing vaccine acceptance.
Materials and Methods
Study Design
When the first COVID-19 vaccine, CoronaVac, arrived in January 2021, HCWs were the first group in the vaccination program. They had a limited period to get vaccinated from January 14 to 20. Before the arrival of the vaccine, an information meeting was organized for all HCWs in our hospital on the efficacy and possible side effects of vaccines available worldwide. After the first vaccination period, we investigated the HCWs who were not vaccinated.
All hospital staff was grouped according to their occupations as doctors, nurses, cleaning staff, “other HCWs,” and “non-HCWs.” The “other HCWs” group included staff such as laboratory technicians and radiology technicians. Those who were not related to healthcare and worked in administrative units were grouped as “non-HCWs.”
First, we conducted a face-to-face survey with the staff who agreed to participate. The occupations, demographic features, health problems, history of COVID-19 disease, and history of antibody tests were questioned in the survey. There were also possible reasons for vaccine hesitation and the future plans for COVID-19 vaccination. After the first survey, we organized several meetings about COVID-19 vaccines. We announced the phone numbers that the staff asked questions about the vaccine, and we answered all questions in light of current scientific information.
From January 14 to April, CoronaVac was the only vaccine option in Turkey. Pfizer-BioNTech arrived in April. After people at high-risk were vaccinated, the Ministry of Health activated the vaccination system for HCWs a second time. At the end of July, the Ministry of Health reactivated the vaccination system for the booster dose for HCWs. The HCWs who did not receive vaccines before could get the primary vaccination with Pfizer-BioNTech. The others could get the booster dose.
In August 2021, we investigated the vaccination status of HCWs for the second time. The HCWs who received the vaccine between the two periods and their vaccine preferences were investigated, and we detected HCWs who were not vaccinated. We conducted a mini survey with unvaccinated staff on the phone, investigating the reasons for vaccine refusal or hesitancy and their vaccination plans. In the second survey, we identified the rate of hospital staff who refused and were still planning the vaccination.
Statistical Analysis
The relationship between the vaccine hesitation reasons and occupation, age, gender, health problems, COVID-19 history, and antibody test history was investigated using SPSS version 26.0 (SPSS Inc., Chicago, USA). Descriptive statistics were used for demographic features, vaccination rates, and plans. The relationship between vaccine hesitancy and occupation was investigated with the Mann-Whitney U test and Chi-Square. The Student’s T-test was used to investigate the relationship between age and vaccination. The Chi-Square test was used to determine the effect of gender on vaccination. The statistical significance was set as p<0.05.
Results
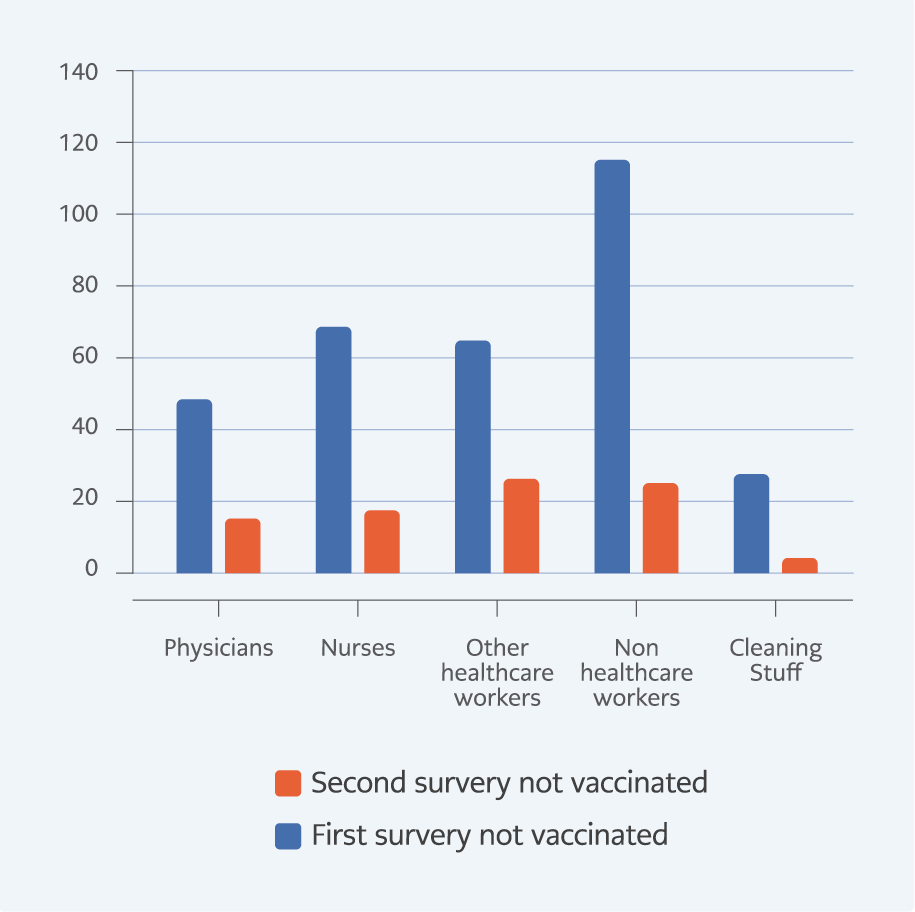
In January 2021, after the healthcare worker’s vaccination period, 1532 HCWs, including 251 physicians and 322 nurses, were investigated. Among them, 325 (21.2%) HCWs were not vaccinated (Table 1) (Figure 1). The mean age was 37.45±8.12 (21-61). In the first survey, the group of non-HCWs (27.7%) included the most unvaccinated participants according to the occupation (Table 1).
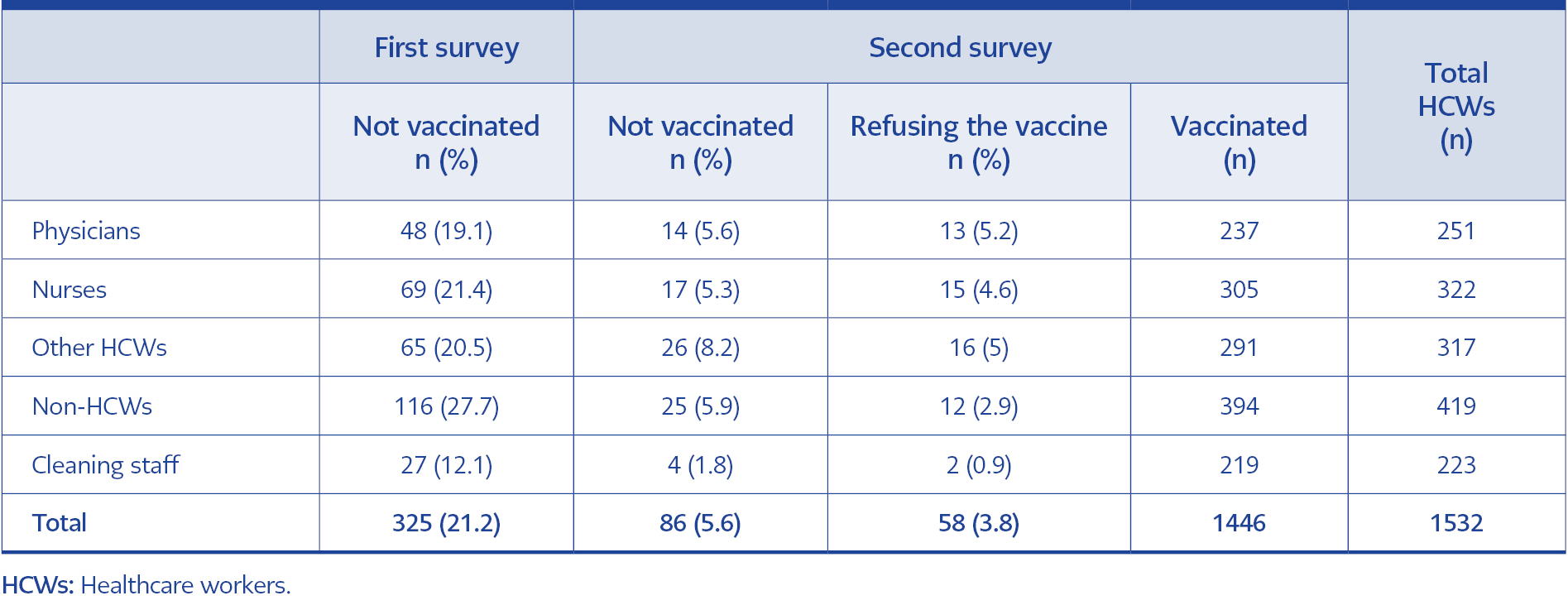
Table 1. Vaccine hesitancy and refusal among healthcare workers and their occupational distribution in the first and last surveys.
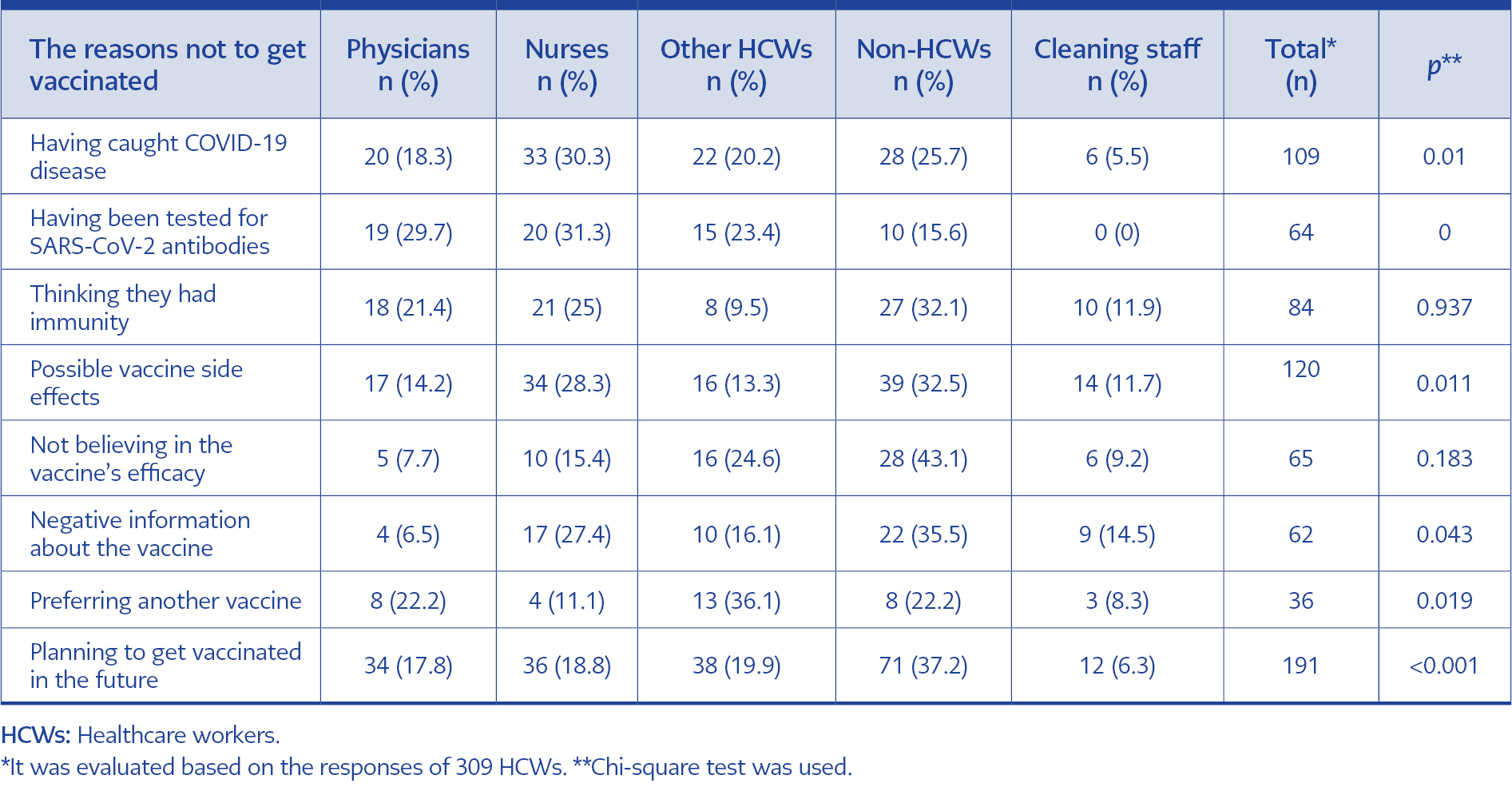
A total of 309 HCWs agreed to participate in the first survey. Two hundred twenty-three (68.4%) of them were female. Seventy-five (23.9%) had a chronic disease. Before the first survey, 109 HCWs (35.3%) were infected with COVID-19. One hundred ninety-one (61.8%) of them were planning the vaccination for the future (Table 2).
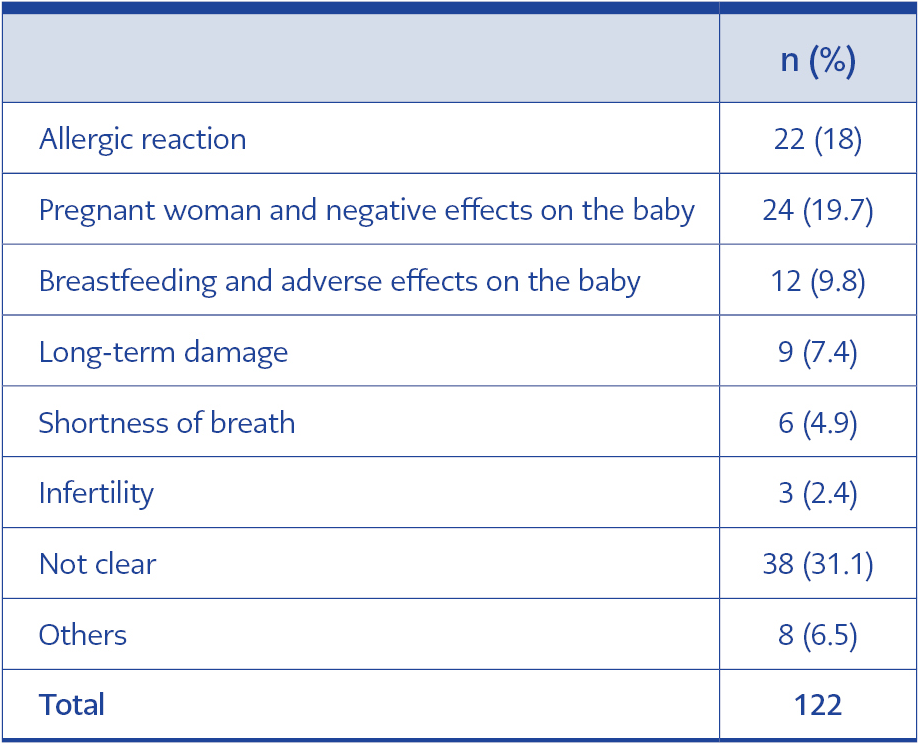
In the first survey, 36 HCWs expressed vaccine hesitancy because they preferred the other vaccine options other than the one available in Turkey (p=0.019) (Table 2). Sixty-four of those who were not vaccinated had an antibody test for SARS-CoV-2, and 84 HCWs did not want to get vaccinated because they thought they were immune to the disease. One hundred twenty-two of them were afraid of the side effects (Table 2). The vaccine hesitancy reason given by 29.5% of HCWs was pregnancy or breastfeeding. Fear of severe allergic reactions was a common reason for vaccine hesitancy (18.0%) (Table 3).
Not accepting the vaccination due to side effects and negative news about the vaccine was associated with the participants’ occupations (p=0.011, p=0.043). The cleaning staff was the most affected by potential side effects and negative news (51.9%; 33.3%) in the first survey.
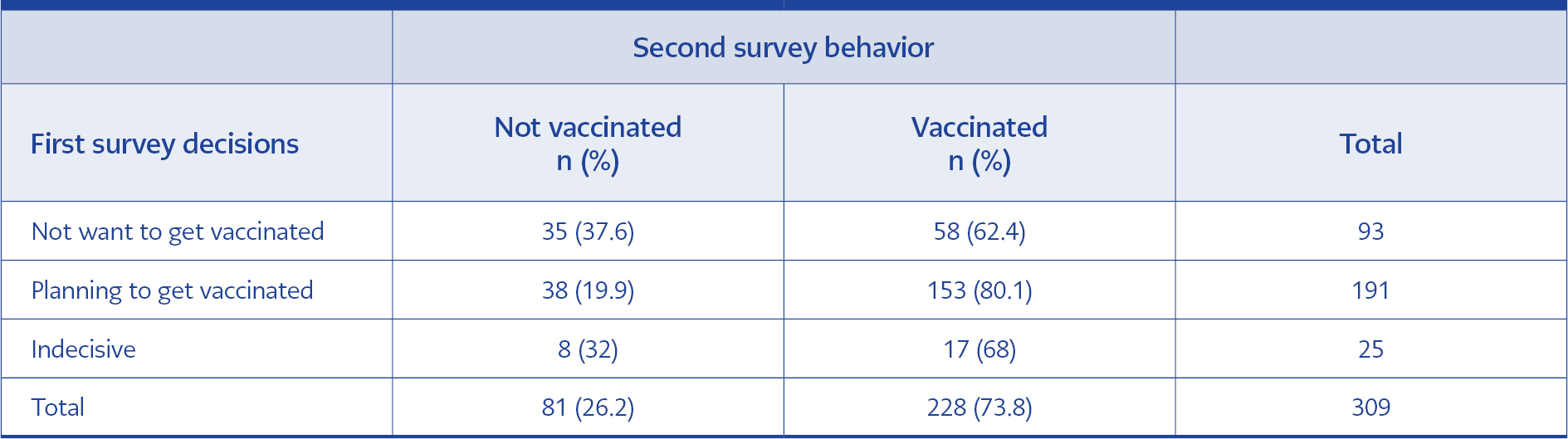
While 62.4% of those who stated that they were not planning to be vaccinated in the first survey were vaccinated between the two surveys, 80.1% of the health workers who said they were planning the vaccination were vaccinated (Table 4). They had 54 (16.6%) CoronaVac, 138 (42.5%) Pfizer-BioNTech, 33 (10.2%) 2 CoronaVac, and 1 Pfizer-BioNTech, 14 (4.3%), 3 CoronaVac vaccines. There was a relationship between vaccination status and occupation in two surveys. While 87.9% of the cleaning staff were vaccinated, 72.3% of the non-HCWs group were vaccinated (p=0.045) in the first survey.
In September 2021, 86 (5.6%) HCWs were still not vaccinated. The group of other HCWs included the most unvaccinated staff in the second survey (8.2%). Twenty-eight (32.5%) of them stated that they had an excuse for delaying it and they were planning to receive the vaccine. According to the second survey, pregnancy and breastfeeding were the most common reasons for vaccine hesitation (42.8%) among the 28 HCWs who were still planning to get vaccinated. In addition, we found that 58 (3.8%) of HCWs were still refusing the vaccine and not planning to be vaccinated. Vaccine refusal was common mostly among physicians (5.2%). Not believing in vaccine efficacy in the first survey was associated with vaccine refusal in the second one (p=0.001). Other reasons for vaccine hesitancy, such as side effects, negative news, and belief that they were already immune, in the first survey were not significantly associated with the vaccine decision in the second survey (p=0.30, p=0.08, p=0.88, respectively). In addition, there was no significant relationship between age, gender, chronic disease history, and vaccination rate in the second survey (p=0.85, p=0.40, p=0.24, respectively).
Discussion
The vaccine hesitancy among the HCWs at the first vaccine arrival was 21.2%, dropping to 5.6% in eight months. Some (3.8%) stated they were refusing the vaccine and not planning to be vaccinated. In studies from different countries, the vaccine hesitancy rates were between 2% and 30% among HCWs (2, 10-12). The rates were initially higher and expected to decrease in time (11).
In several studies, vaccine hesitancy was related to sex, age, education, income level, and health problems (2, 12-16). However, we found no relation between age, sex, having a chronic disease and vaccine hesitancy.
In our study, there was an association with the HCW’s occupation. The highest vaccine hesitancy rate was in the group of non-HCWs (27.7%). After eight months, the “other HCWs” group had the highest vaccine hesitancy rate (8.2%). In both surveys, the lowest rate was among the cleaning staff (12.1%; 1.8%). In the second survey, the highest rates of vaccine refusal were among physicians. Contrary to our study, physicians had the highest compliance rates in some other studies (3, 6, 10, 16).
Vaccine hesitancy is related to cultural reasons, local problems, influencers other than efficacy, and side effects (2, 7, 14, 17). As in other studies, the most common reason for vaccine hesitancy was possible side effects (38.8%) (7, 11, 13, 18). Breastfeeding (9.8%) and pregnant (19.7%) HCWs were the most likely to be hesitant about the possible side effects and postpone the vaccination in our study (7, 16); in the second survey, the rate was 42.8%. Of the HCWs stated that the reason for their vaccine hesitancy was the possible side effects, 31.4% could not have expressed which side effect it was. Another common reason for hesitation was allergic reactions to vaccine components. Another study showed that this hesitancy was not due to a history of allergic reactions (10).
Our results were similar to other studies regarding not believing in vaccine efficacy (21.0%) and the effect of negative information about the vaccine (20.1%) (11). In our study, some HCWs reported that they preferred different vaccines. Having more options could be another reason for the increase in the acceptance of vaccines in time.
The number of HCWs who already had COVID-19 was high among the group with vaccine hesitancy (35.3%) in the first survey. Not having a COVID-19 history was associated with high vaccine acceptance in a study (6). Expecting natural immunity protection after having COVID-19 could be another reason for vaccine hesitancy (19), especially when there was no clear information about immunity after the disease. Vanning immunity and multiple COVID-19 experiences could be another reason for the decrease in vaccine hesitancy.
While 80.1% of workers who planned to get vaccinated in the first survey were vaccinated in the second, (62.4%) not planned were vaccinated in the last. After witnessing experiences with the vaccine, more information about the efficacy and safety changed the hesitancy rates in a few months (11, 19). The lack of knowledge and trust were the main problems for some HCWs (2, 7, 18, 19). There was not enough time to persuade them and disseminate the correct information. In the beginning, effective communication and information could eliminate fear and distrust (7, 20). In our study, most of those who did not plan to be vaccinated in the beginning were vaccinated at the last survey as a result of training, one-on-one interviews, and observing experiences related to vaccination.
Not believing in vaccine efficacy was the only reason that affected the vaccination status we investigated in the second survey. It was related to complex vaccine refusal reasons such as psychology, political opinion, and religious belief (9, 15, 21). Most of the vaccine hesitancy reasons among HCWs at the beginning of the COVID-19 pandemic and vaccine refusion reasons at the end were not the same (21, 22).
Breastfeeding and pregnancy were the big concerns regarding vaccine hesitancy in the second survey; nevertheless, there was sufficient information about vaccine safety in pregnant and breastfeeding women. Most HCWs’ vaccine hesitancy from the beginning to the end was related to wrong information and was preventable with correct information and teamwork at hospitals (7, 22).
Our study was conducted among HCWs, and it has limitations in terms of reflecting society. Although all unvaccinated HCWs in our hospital were included in the study, our survey population was small. In addition, there were no questions about psychological, political, religious, or cultural reasons for vaccine rejection in our survey.
In conclusion, the overall rate of vaccine rejection was low among HCWs. Nevertheless, despite having more information about the vaccines and more vaccine options, physicians, nurses, and other HCWs had higher vaccine refusal rates than the “non-HCWs” group. In both surveys, the most common reason for hesitancy was the fear of possible side effects, especially among pregnant and breastfeeding HCWs. However, vaccine refusal among HCWs having more information about the vaccine and disease than the community may be related to cultural, psychological, and political reasons other than efficacy and safety. Future studies on the cultural, psychological, and political reasons for vaccine refusal will contribute to understanding vaccine refusal and increasing vaccine acceptance.