Introduction
At the end of 2019, a novel coronavirus was identified as the cause of a cluster of pneumonia cases in Wuhan, a city in the Hubei Province of China. It spread rapidly, resulting in a pandemic throughout the world. In February 2020, the World Health Organization (WHO) named the disease COVID-19 (1, 2). Studies reported that COVID-19 mostly progressed with asymptomatic or mild pneumonia; however, more severe or critical pneumonia and death were seen in elderly patients (3).
As the population has got older worldwide, old age is becoming one of the most important problems for many countries. For instance, in Turkey, 10% of the population was found to be over the age of 65 at the end of 2019 (4). Elderly patients have higher morbidity and mortality rates compared to younger individuals because of underlying diseases. As a result, although the entire population is susceptible to SARS-CoV-2, the group requiring hospital monitoring includes the elderly mostly.
The vast majority of patients infected with SARS-CoV-2 are over the age of 50, and approximately 80% of the deaths are over the age of 60 (5, 6). Infections can be atypical in elderly patients. Since COVID-19 is a newly defined disease, it is important to determine its clinical features in elderly patients (7). Considering the excess of age-related sensitivity and complications, determining the clinical characteristics associated with SARS-COV-2 infection may contribute to reducing mortality in elderly patients. The number of studies examining the factors determining clinical severity in elderly patients is limited (3, 5). Therefore, in our study, we aimed to evaluate the factors that determine the severity of the disease in elderly patients who were followed up in our hospital.
Materials and Methods
The files of definite or probable COVID-19 patients over 65 years of age who were followed up by the infectious diseases clinic of our hospital between March 15 and October 1, 2020, were evaluated retrospectively. Demographic, clinical, laboratory and clinical course information were recorded. When we evaluated underlying diseases in patients, two or more comorbid situations (accompanying diseases or conditions) were defined as multimorbidity. Cases were defined according to the COVID-19 guidelines of the Republic of Turkey Ministry of Health. Although the SARS-COV-2 real-time polymerase chain reaction (RT-PCR) test was negative, the patient with appropriate clinical complaints and findings consistent with viral pneumonia in thorax computed tomography (CT) were accepted as a possible case. Cases that were found to have SARS-CoV-2 by molecular methods were defined as confirmed cases. If the RT-PCR test for SARS-CoV-2 was negative, it was repeated 24 hours later in patients with clinical, laboratory and radiological findings compatible with COVID-19 (8).
Clinically mild-moderate or severe patients were included in the study according to the Republic of Turkey Ministry of Health COVID-19 Guide (9) Patients having fever, muscle/joint pains, cough and sore throat, respiratory rate <30/minute, SpO2 level >90% in room air, and mild-moderate pneumonia finding on chest X-ray or tomography were defined as mild to moderate cases; and those having altered consciousness, respiratory distress, respiratory rate ≥ 30, room air SpO2 ≤ 90%, bilateral diffuse (>50%) involvement on lung imaging were defined as severe cases. Indications for hospital follow-up and selection of antiviral treatment, doses were made in line with the recommendations of the Republic of Turkey Ministry of Health COVID-19 Adult Patient Treatment Guide (9). The duration of hospitalization, follow-up in the intensive care unit, death and discharge status of the patients were recorded.
Laboratory measurements
A definitive diagnosis was made detecting the SARS-CoV-2 virus in oropharyngeal and nasopharyngeal swabs by RT-PCR. Complete blood count, electrolytes, kidney and liver tests, creatine kinase and MB fraction, high-sensitive troponin, D-dimer, ferritin, C-reactive protein (CRP) and procalcitonin (PCT) were studied in the patients. Necessary permission and local ethics committee approval were obtained from the Republic of Turkey Ministry of Health for the study. Descriptive statistics, statistical relationships and differences were examined for the obtained information. While the mean, standard deviation, median and interquartile range (IQR) were obtained for continuous quantitative variables, interpretations were obtained by giving frequencies and percentages for categorical variables. While statistical analyzes were performed, independent t-test for pairwise comparison, ANOVA for multi-group comparison, and chi-square analysis for categorical data were used according to the parametric properties of the data. In the measurement of the variables that did not meet the distribution and scatter conditions, Mann Whiney-U and Kruskal Wallis examinations were performed, respectively, from non-parametric alternative methods. In advanced statistical analysis, selective multiple logistic regression and binary logistic regression models were obtained and interpretations were made based on explanation ratio, correct classification ratio and odds ratios. Statistical significance was interpreted at a 95% confidence level.
Results
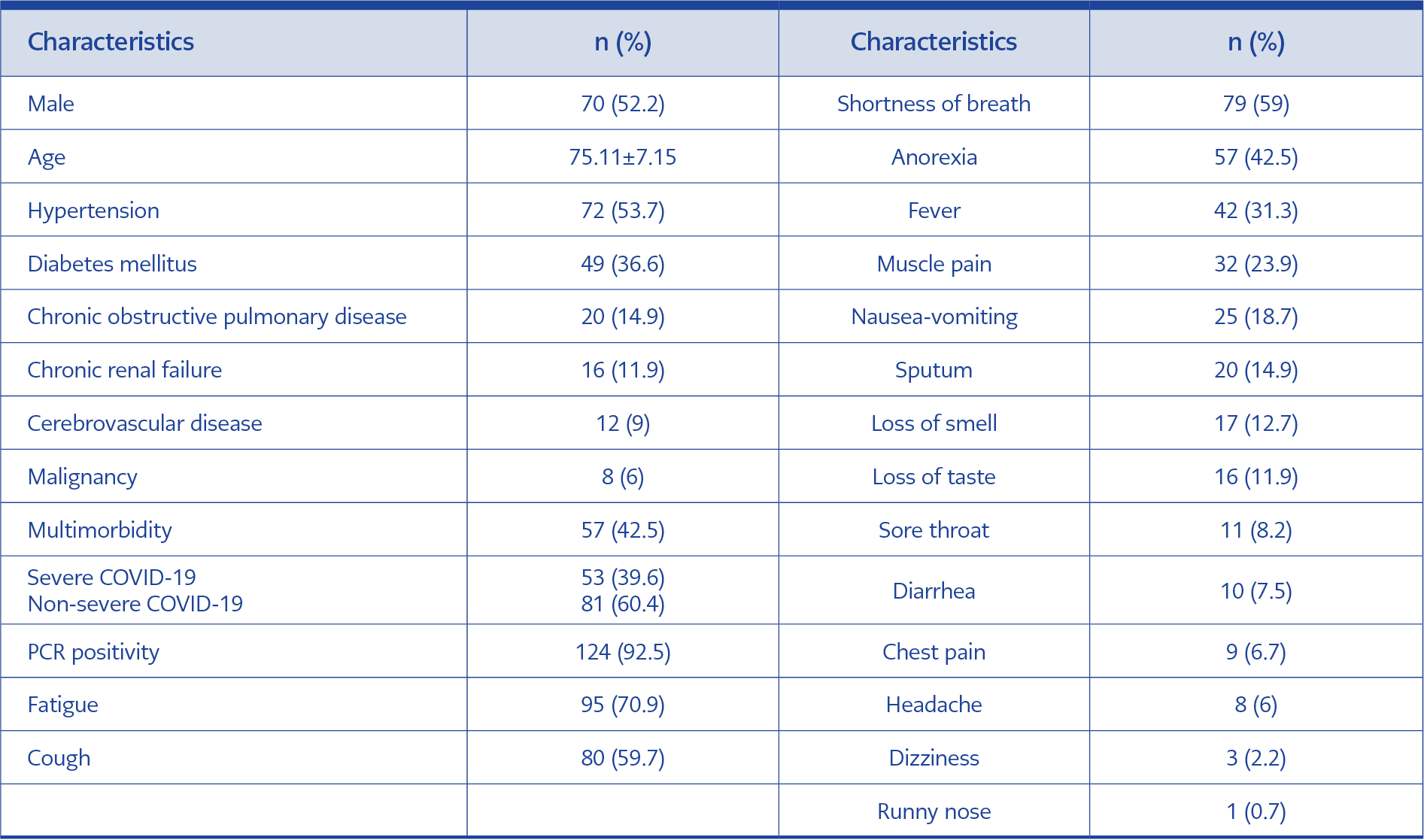
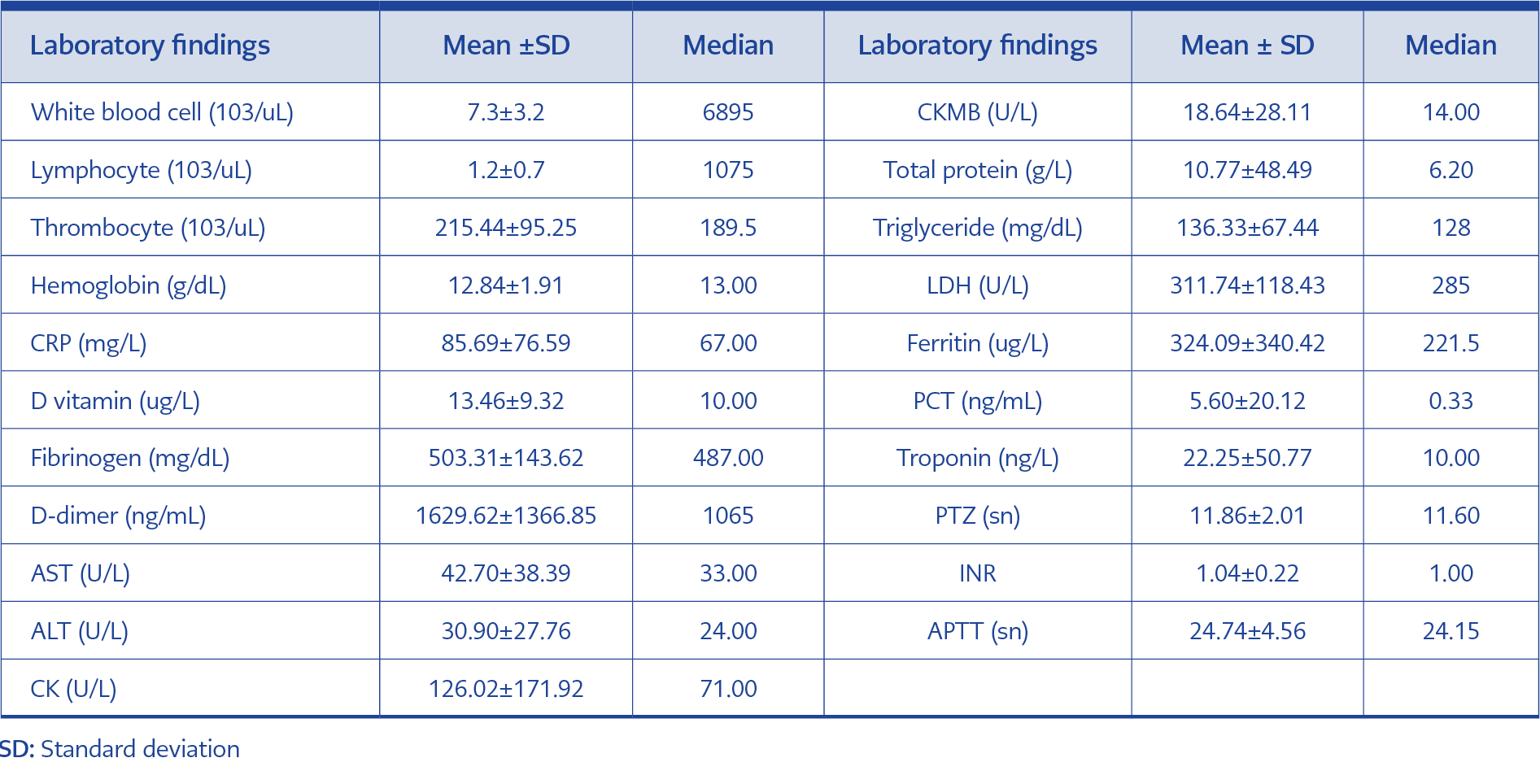
A total of 134 patients were included in the study, 52.2% of the patients were male and the mean age was 75.11±7.15 (min 65-max 94). Multimorbidity was detected in 42.5% of the patients. The most common comorbidities were hypertension (53.7%) and diabetes mellitus (36.6%). Severe COVID-19 was defined in 39.6% of patients. The most common complaints were fatigue (70.9%), cough (59.7%), and shortness of breath (59%). The characteristic data of the patients are given in Table 1. When the laboratory findings of the patients were evaluated the median of the white blood cell was 6895 (103/uL), the median of the lymphocyte was 1075 (103/uL), and the median of the D-dimer was 1065 ng/mL. The laboratory values of the patients are given in Table 2.
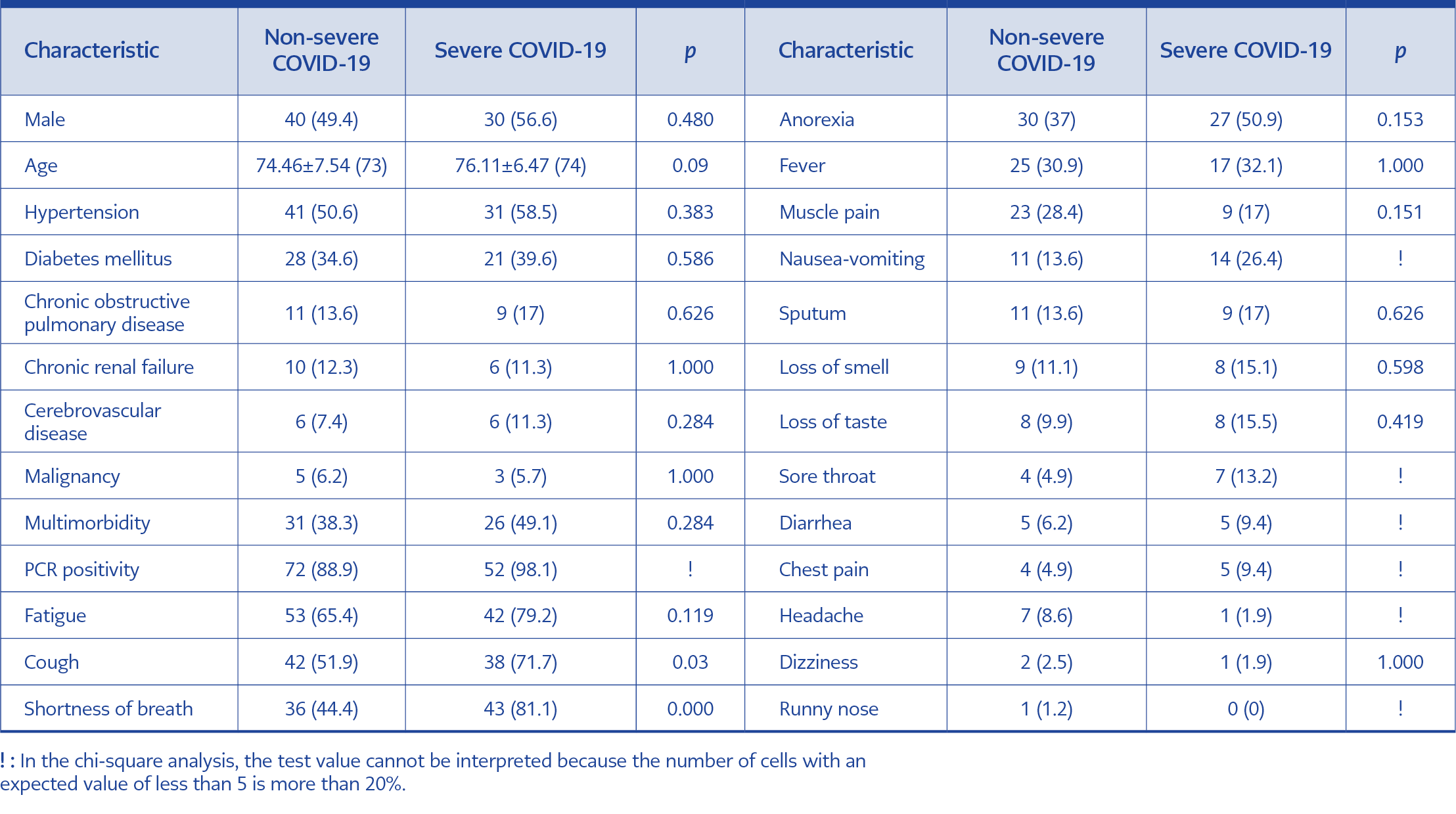
Table 4. Comparison of demographic data and application complaints of severe and non-serious patient groups in elderly patients.
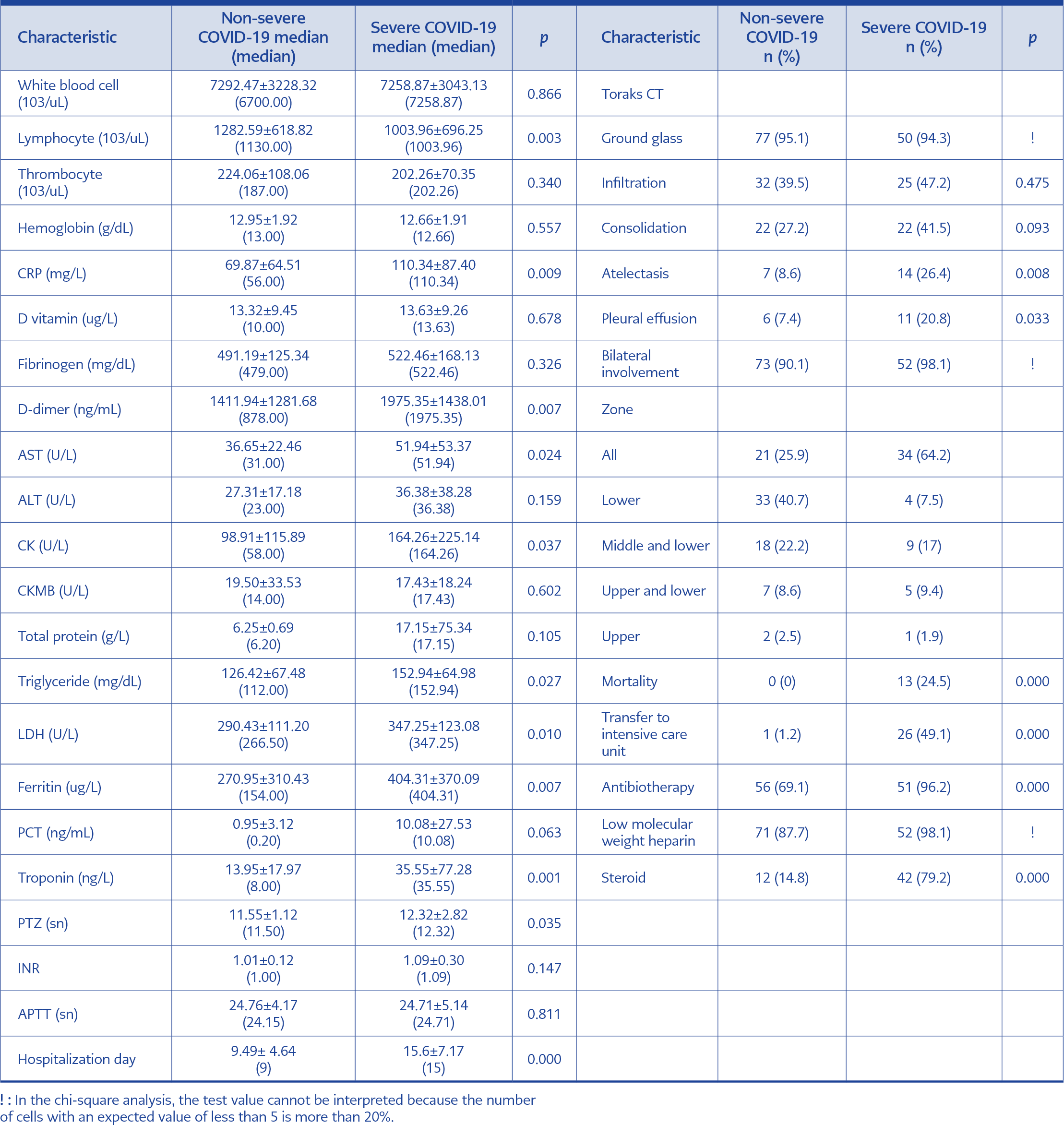
Table 5. Comparison of laboratory values, thorax CT findings, treatment and clinical course of severe and non-serious
patient groups in elderly patients.
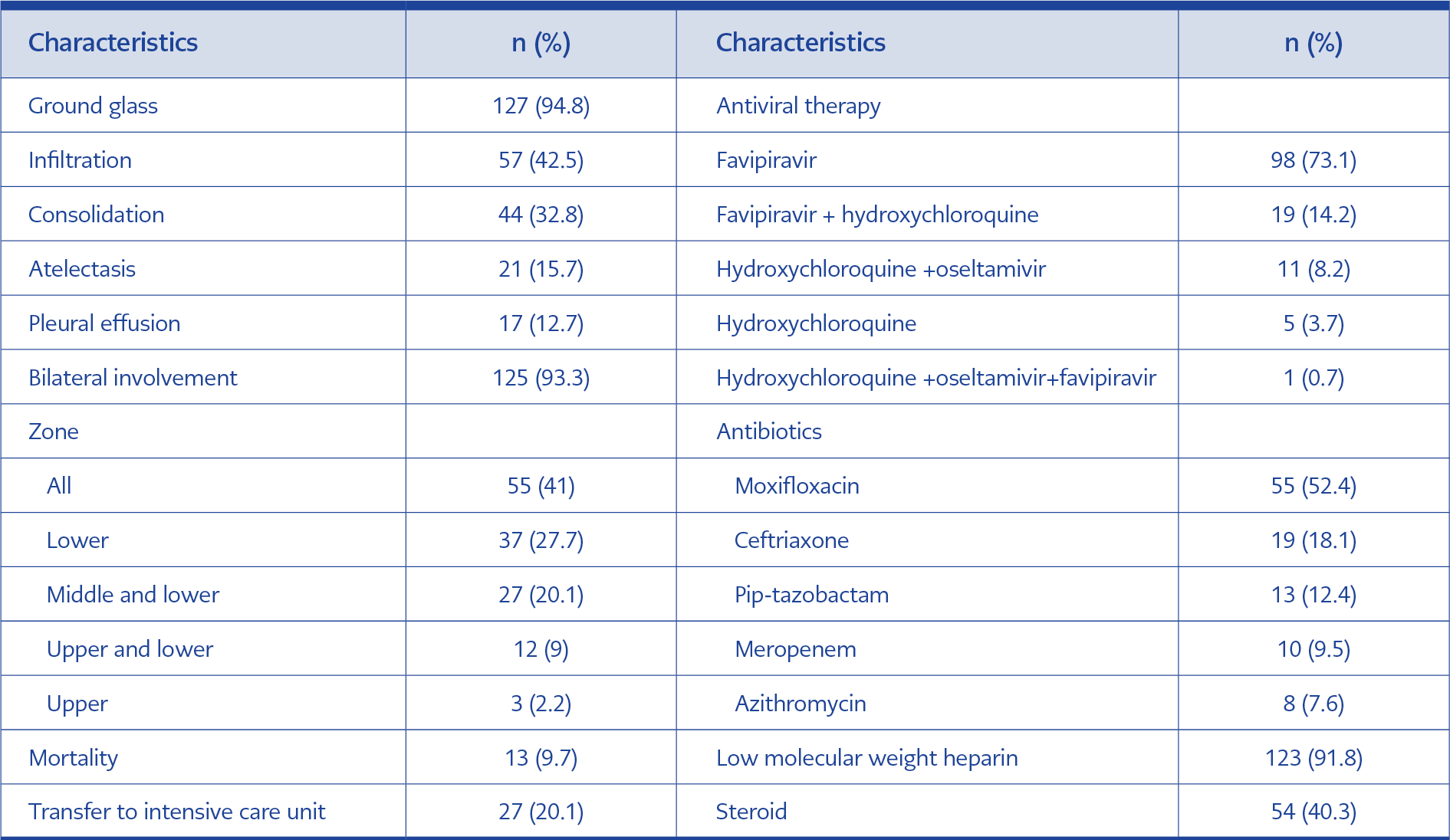
Ground-glass was observed in 94.8% (n=127) of the patients’ CT scans, infiltration in 42.5% (n=57) and consolidation in 32.8% (n=44). There was bilateral involvement in 93.3% (n=125) of the patients. The involvement was observed in all lung areas in 41% (n=55) of the patients, and in the lower lobe in 27.6% (n=37). The most commonly used antiviral treatment in patients was favipiravir 73.1% (n=98). Low molecular weight heparin prophylaxis was added to the treatment in 91.8% of the patients, and antibiotics were used in 80% (n=107). Moxifloxacin was the most commonly used antibiotic (52.4%). Steroids were added to the treatment of our patients who needed oxygen (40.3%) following the COVID-19 treatment guide of the Ministry of Health. 6 mg/kg of dexamethasone or equivalent prednisolone was given for 10 days (9). The average hospitalization period of the patients was 12±6.36 days, the rate of follow-up in the intensive care unit was 20.1% (n=27), and death occurred in 9.7% (n=13) of the patients (Table 3).
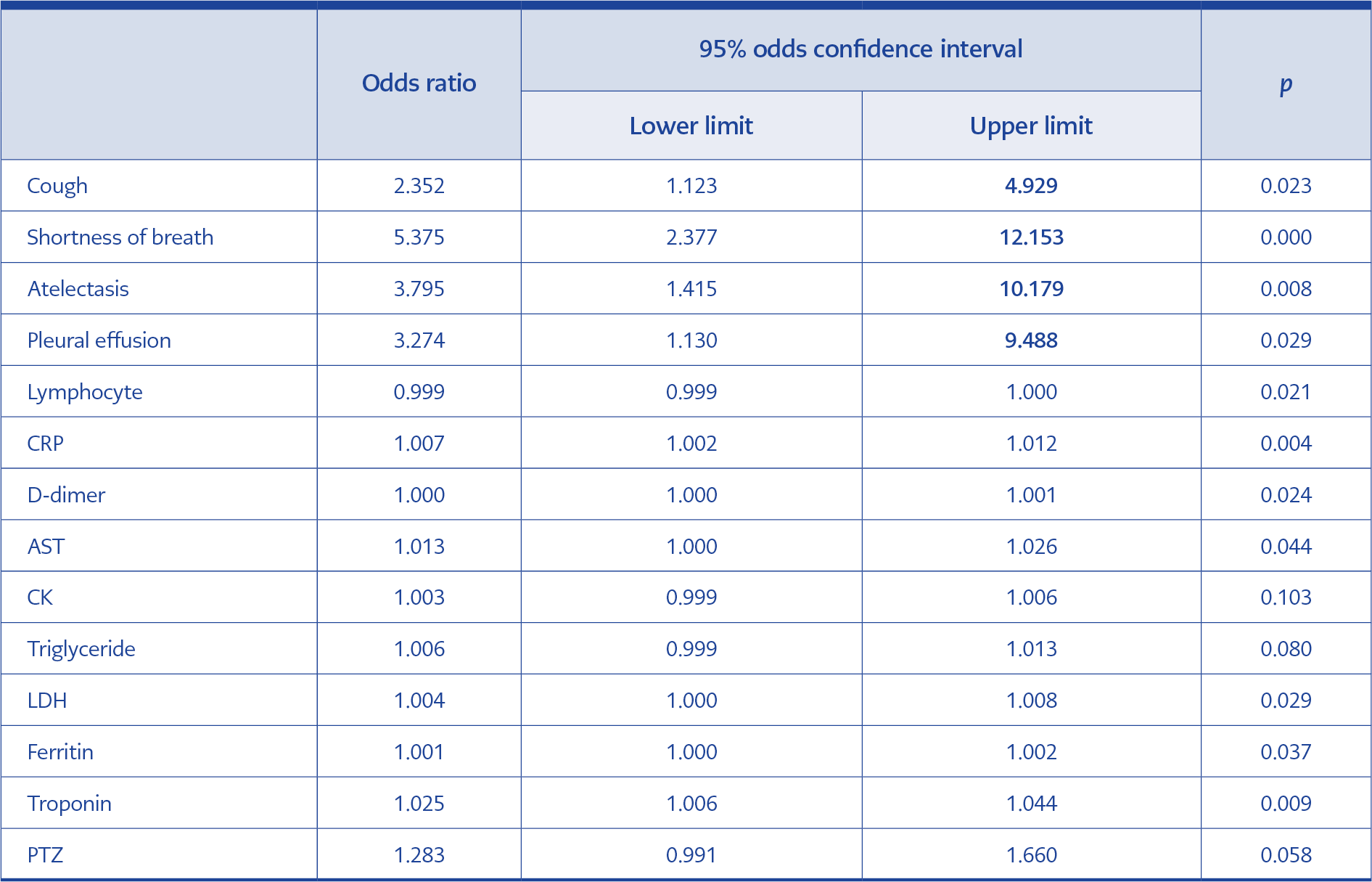
In the patient group with severe COVID-19, complaints of breath shortness and cough at the time of admission, and atelectasis and pleural effusion findings on thorax CT were significantly higher than the non-severe group (p< 0.05). Lymphocyte, CRP, D-dimer, aspartate aminotransferase (AST), creatine kinase (CK), triglyceride, lactate dehydrogenase (LDH), ferritin, troponin, prothrombin time (PTZ) values were significantly higher in the patients with severe disease than non-severe group (p<0.05). The rate of steroid and antibiotic treatment in the severe COVID-19 group was significantly higher, and the average of transfer to the intensive care unit, death and hospitalization time was higher in this group (p<0.05). No significant difference was found in terms of other variables (p>0.05). Demographic, laboratory and treatment information according to severe and non-severe groups are given in Tables 4 and 5.
In the multivariate analysis of the variables that were significant in the univariate analysis in severe and non-severe patient groups; cough and shortness of breath at admission, atelectasis and pleural effusion on thorax CT were found to be significant for severe COVID-19 disease (p<0.05). The variables that increase the risk of severe COVID-19 are the cough (2.35 times), shortness of breath (5.38 times), the presence of atelectasis in thorax CT (3.8 times), development of pleural effusion (3.17 times). No significant difference was found in terms of other variables (p>0.05). Multivariate analysis of risk factors for severe COVID-19 is given in Table 6.
Discussion
Studies have reported that the most common complaints in elderly patients are cough, shortness of breath, sputum, fever and fatigue (3, 5, 10-13). However, atypical complaints of infection can be seen in elderly patients. In a study, fatigue (58.8%), diarrhea (35.3%), falls (23.5%) and delirium (52.9%) were detected following fever, cough and dyspnea (14). In our study, fatigue (70%), cough (59.7%), shortness of breath (59%), anorexia (42.5%), and fever (31.3%) were the most common complaints. The elder people are naturally susceptible to fatigue. Combined with the effects of hypoxia, the proportion of elderly patients with fatigue is also higher than in the general population (5). Therefore, we evaluated fatigue and anorexia as atypical complaints related to the disease. Similar to the study of Steinmeyer et al., fatigue was the most common complaint (15). Atypical complaints in elderly patients can delay the quarantine process, as well as diagnosis and treatment, making it difficult to control disease transmission.
The most common chronic diseases in elderly patients have been reported as hypertension, diabetes mellitus, dementia, cardiovascular diseases and chronic respiratory diseases (5, 10-13, 15). The most common comorbid diseases among our patients were diabetes mellitus, hypertension and chronic obstructive pulmonary disease and 42.5% of them had multimorbidity.
In a study conducted among elder patients, the mean white blood cell was 8.4 ±4.5 (109/L), the mean lymphocyte was 1.3±0.6 (109/L), the mean CRP was 93.2±86.1 mg/L (10). In another study, the mean white blood cell was 7.54 ±4.3 (109/L), the mean lymphocyte was 1.1±0.4 (109/L), the mean D-dimer was 0.7±0.6 (ng/ml) (5). When the laboratory values of our patients were examined, the mean white blood cell was 7.3 ±3.1 (6895) (103/uL), the mean lymphocyte was 1.2±0.6 (1075) (103/uL), the mean CRP was 85.69±76.59 (67) mg/L, the mean D-dimer was 1629.62±1366.85 (1065) ng/mL and our results were consistent with the other studies.
In a study, ground-glass appearance (81%) and consolidation (52%) were reported as the most common thorax CT findings in elderly patients, with a bilateral involvement rate of 74% (5). In another study, the most common finding was ground-glass (80%), followed by bilateral involvement (58%) and pleural effusion ( 23.3%) (15). In another study conducted in elderly patients, 85% bilateral involvement was observed on thorax CT, and ground glass appearance and consolidation were the most common findings, and pleural effusion was observed in 10.3% of the patients (12). Similarly, bilateral involvement (93.3%) was common on thorax CT in our study, and the most common lesion was ground-glass (94.8%). We observed pleural effusion in 12.7% of our patients. In the elderly patient group, CT findings may be complicated depending on the underlying diseases (heart failure, chronic lung disease). Pleural effusion is a finding frequently encountered in elderly patients because of comorbidities (12, 15). Unlike previous studies in elderly patients, atelectasis was found in 15.7% of our patients.
COVID-19 may progress more severely in elderly patients, therefore it is important to identify the risk factors that determine the course of severe illness and provide early medical support (3). It is stated that concomitant comorbid diseases and advanced age cause severe disease (16-19). In a study in which the risk factors that increase the severity of the disease were performed in elderly patients, fatigue, shortness of breath, complaints of fever, accompanying comorbid diseases and age were found to be significantly higher in the group with severe COVID-19 than the non-severe patient group (5). In contrast, another study found no significant relationship between disease severity and symptoms, comorbid diseases, and age in elderly patients (3). In our study, dyspnea and cough complaints were more common in the group with severe disease, but no difference was found in terms of comorbid diseases and age.
As in studies involving all age groups, low lymphocyte and thrombocyte counts, prolonged coagulation time, increased D-dimer, transaminase, bilirubin and creatinine are significant laboratory findings in elderly patients. In a study investigating the severity of the disease in elderly patients, the number of lymphocytes was lower than the non-severe group, and neutrophils, PTZ, D-dimer, transaminases, bilirubin, creatinine, troponin, ferritin, and PCT were found to be higher than the non-severe group (3). Similarly, in another study investigating the severity of the disease in elderly patients, lymphocyte, albumin, LDH, bilirubin, CRP, PTZ, D-dimer, and PCT were variables that made a difference (5). In our study, it was determined that the lymphocyte count was lower in patients with severe disease, and CRP, D-dimer, AST, CK, triglyceride, LDH, ferritin, troponin, and PTZ values were significantly higher than in the non-severe group.
The lung is one of the organs most affected by COVID-19. In elderly patients, similar to the whole population, bilateral involvement and ground-glass appearance are most common in thorax CT (3, 5, 12, 15). The presence of atelectasis and pleural effusion was observed more in the severe group. A similar study showed that consolidation was significantly higher in elderly patients with severe disease (5). We believe that accompanying pathologies in the lung increase the severity of the disease by increasing respiratory failure.
Dexamethasone and other glucocorticoids, remdesivir, baricitinib and the other Janus kinase (JAK) inhibitors, IL-6 inhibitors (tocilizumab) and monoclonal antibodies are recommended for COVID-19 treatment (20). In Turkey, hydroxychloroquine treatment was started to our patients in the early stages of the epidemic in line with the COVID-19 treatment guide recommendations of the Ministry of Health; however, after many large randomized studies, it was concluded that it had no clinical benefit and no contribution in reducing mortality in patients. Then, it was removed from the guideline recommendations. In the guide of the Republic of Turkey Ministry of Health, it was recommended to add oseltamivir to the treatment of influenza cases at the beginning of the epidemic (9).
Favipiravir is an RNA polymerase inhibitor available in some countries in Asia (including India and Russia) for the treatment of non-severe COVID-19. Data of outcomes are mixed, some trials have suggested more rapid virologic clearance and clinical improvement with favipiravir, but most were limited by potential confounders (20). These treatments have been used in the treatment of COVID-19 patients in line with the recommendations of national guidelines (9).
Antibiotics may be indicated in patients with COVID-19 due to suspected or confirmed bacterial superinfection. In some studies, the rate of antibiotic use varies between 58-71% in COVID-19 patients (21, 22, 23). The severity of disease, the probability of bacterial superinfection and the increased workload of prescribers may lower the threshold for antibiotic use (23). Moxifloxacin was mentioned as the most common choice in one study (24). In a multicenter study, 62% of physicians stated that they used antibiotics in the treatment of COVID-19 patients (24). The high rate of antibiotic use in our study was attributed to the high rate of serious illness, high CRP and procalcitonin values in our patients. In addition, the widespread use of antibiotics by physicians may have resulted from the lack of information in the first period of the epidemic.
In our study, we observed that the rate of steroid and antibiotic use in the treatment of the patient group with severe COVID-19 was significantly higher, and the average of transfer to the intensive care unit, death and hospitalization time was higher in this group compared to the non-severe group. Similarly, in the severe COVID-19 in elderly patients, the use of antibiotics, systemic steroids and invasive O2 support systems was high, as well as mortality rate (5). Because of the weak compensatory functions of many organs in elderly patients, more intensive medical treatment is applied in the severe course.
In the study of Li et al., age, SOFA score, APACHE score, thrombocyte, D-dimer, creatinine, IL-6 and presence of consolidation were determined as independent variables affecting disease severity (5). In our study, cough, shortness of breath, atelectasis on thorax CT, presence of pleural effusion are independent variables for severe COVID-19 disease. The presence of cough (2.35 times), shortness of breath (5.38 times), the presence of atelectasis on thorax CT (3.8 times), the presence of pleural effusion (3.17 times) increase the risk of severe COVID-19. According to the results of our study, the presence of additional problems with the lung on thorax CT, cough and shortness of breath at admission are the most important factors affecting the severity of COVID-19 in elderly patients. Although the variables such as dyspnea and cough are also markers of severity, which were also detected in studies in adult COVID-19 patients, it is expected to be encountered in the elderly group with a higher rate of severe course of the disease.
Our study is important in that it draws attention to abnormalities such as consolidation, pleural effusion and atelectasis in thorax CT in demonstrating the severity of the disease. There are some limitations of our study. First, it contains data from a single center and provides information about the small number of hospitalized elderly patients. Second, it has a retrospective design.
In conclusion, independent variables determining disease severity in elderly patients in our study are cough, shortness of breath, pleural effusion and atelectasis on chest CT. The duration of hospitalization, transfer to the intensive care unit, and death rate are significantly higher in elderly patients. Therefore, providing early medical support to these patients, especially in the presence of cough and shortness of breath on admission and in the presence of pleural effusion and atelectasis on thorax CT, may help to reduce the poor clinical course.