Introduction
Coronavirus disease (COVID-19) remarkably impacted mortality rates and healthcare resources (1, 2). The causative virus, SARS-CoV-2, is a member of the β family (3). Pulmonary manifestations of COVID-19 can range from asymptomatic infection to severe pneumonia and acute respiratory distress syndrome (4, 5). Research regarding risk classifications continues to determine the pathophysiology of SARS-CoV-2 and develop safe and effective treatment strategies for COVID-19 patients. A new biochemical marker to assess the severity of COVID-19 may facilitate appropriate supportive care and symptom management and, ultimately, reduce mortality (6).
Various pathophysiological pathways, such as direct viral toxicity, endothelial cell damage, and thromboinflammation, are discussed in the pathogenesis of the disease. The dysregulation of the immune response and the renin-angiotensin-aldosterone system has been identified as an important mechanism. Angiotensin-converting-enzyme 2 receptors, which are the entry mechanism of the virus, are expressed in many tissues. In addition, the dysregulation of the osmotic system with hyponatremia has been described in some cases. Arginine vasopressin (AVP), also known as “antidiuretic hormone”, is an antidiuretic and vasoconstrictive hormone. It exhibits an endogenous stress response, and its release is increased by stimuli such as hypotension, hypoxia, hyperosmolarity, acidosis, and infections. However, its circadian rhythm, short half-life, and unstable molecules render it difficult to use as a biomarker. Copeptin has a more stable structure, and its levels in the blood can be easily detected (7-10). Copeptin is the C-terminal peptide resulting from the cleavage of pre-pro-arginine vasopressin. It is released from the posterior pituitary gland into systemic circulation in response to various stimuli, including stress (11, 12). The prognostic role of copeptin has been reported in various clinical conditions, including infectious and cardiovascular diseases. Studies have demonstrated that serum copeptin levels increase due to infectious diseases, such as pneumonia, ventilator-associated pneumonia, and sepsis or septic shock in the community, and this increase is associated with poor prognosis (11, 13-16). Very few studies have examined the role of copeptin in determining prognoses in patients with COVID-19 (4, 5). Therefore, through this study, we aimed to evaluate the role of copeptin in determining the severity of the disease in patients with COVID-19.
Materials and Methods
SARS-CoV-2 PCR-positive patients who were followed up in the pandemic wards with diagnoses of COVID-19 between June 1 and October 1, 2022, were included in the study. Demographic and clinical features and radiological and laboratory findings regarding the patients were recorded in the forms. Laboratory features, including complete blood count, electrolytes, kidney and liver tests, troponin, D-dimer, ferritin, C-reactive-protein, procalcitonin, copeptin and SARS-CoV-2 PCR, were taken during the patient’s admission to the infectious disease clinic for hospitalization (Day 0). The length of the hospital stay, the treatments applied, the need for intensive care, and the death and discharge status were noted. Serum taken from the patients for copeptin measurement was stored at -80 °C after centrifugation.
Thoracic computed tomography (CT) was performed in all patients with suspected pneumonia. Radiological evaluations were performed alongside low-dose non-contrast CT of the thorax (16-section multidetector Aquilion One; Toshiba Medical Systems Corporation, Japan). All images were taken in the supine position with full inspiration. Bilateral and unilateral involvement, as well as the ground glass appearance and consolidation in the affected zone(s) were noted. Patients with pregnancy, malignancy, coronary disease, heart failure, chronic renal failure, immunosuppression, autoimmune disease, and chronic obstructive disease were excluded from the study.
Disease severity classification was made as mild-moderate and severe according to the COVID-19 Guide of the Ministry of Health of the Republic of Türkiye. According to this guideline, cases with fever, muscle/joint pain, cough and sore throat, respiratory rate <30/min, SpO2 level >90% in room air, and mild-moderate pneumonia findings on chest radiography and/or thorax tomography are considered mild-moderate cases. Severe cases were defined as those with changes in consciousness, respiratory distress, respiratory rate ≥ 30, SpO2 ≤ 90% on room air, and bilateral diffuse involvement (>50%) on lung imaging (17). The duration of hospital stays, the intensive care unit follow-up, and the patient’s death and discharge status were recorded. Serum copeptin measurements were performed with a BT LAB Human Copeptin, CPP ELISA Kit (BT LAB Bioassay Technology Laboratory, UK). An absorbance reading was performed on a ChroMate 4300 ELISA (Awareness Technology, Inc., USA) microplate reader. The measurement was made at 450 nm. The data were calculated using a four-parameter logistic regression analysis. The results are indicated in ng/mL.
Kütahya Health Sciences University Ethics Committee approved the study on February 25, 2022, with decision number 2022/06-07. All patients were informed about the study and obtained their written consent.
Statistical Analyzes
Histogram graphs and the Kolmogorov-Smirnov test were used to evaluate the distribution of continuous data. Those with normal distribution were presented with mean ± standard deviation, and those with non-normal distribution were presented with median (minimum-maximum). An independent-sample T-test was used to compare normally distributed data, and the Mann-Whitney U test was used to compare non-normally distributed data. Categorical data were presented as numbers (%), and the chi-square test was used for comparison. The receiver operating characteristic (ROC) analysis was used to evaluate the diagnostic performances of the tests. The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 25.0 (IBM Corp., Armonk, NY, USA). The statistical significance was set as p<0.05.
Results
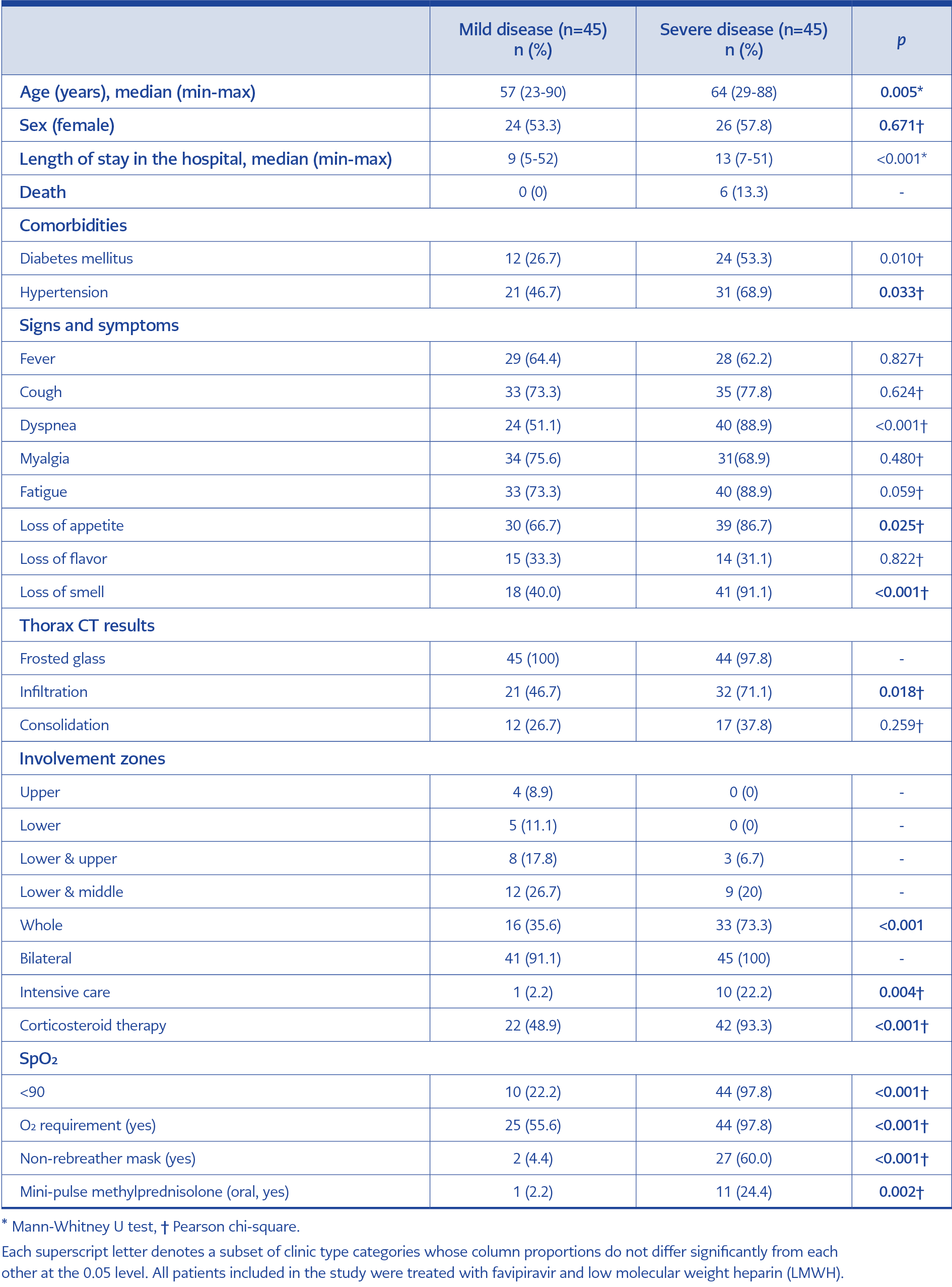
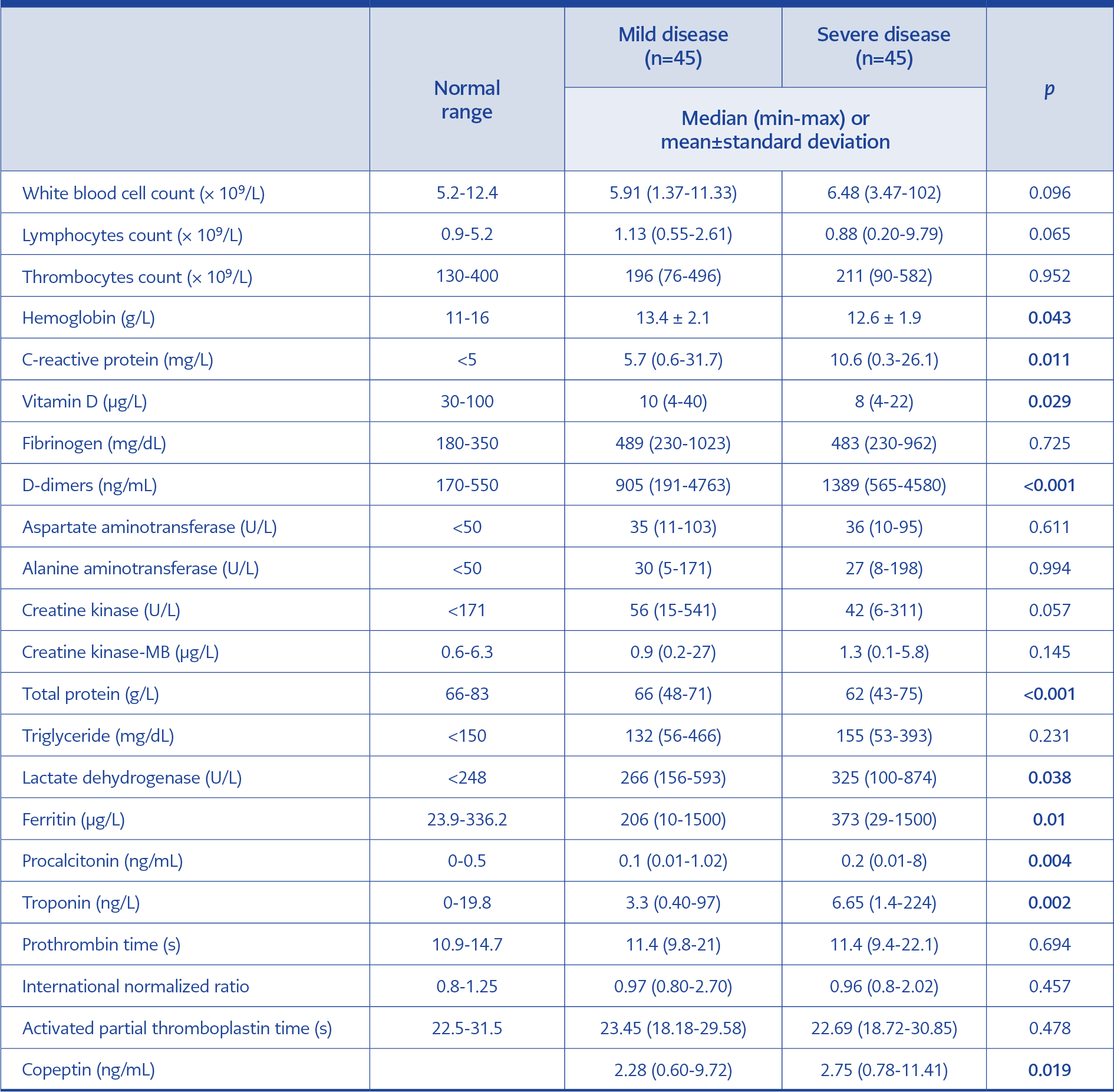
Table 1. Demographic and baseline characteristics of patients with mild and severe COVID-19 disease groups.
A total of 90 patients were included in the study: 45 in the mild disease group and 45 in the severe disease group. While the median age was 64 years old in the severe disease group, it was 57 years in the mild disease group (p=0.005). The frequency of comorbidity was also significantly higher in the severe group (p=0.010 for the patients with diabetes mellitus and p=0.033 for those with hypertension). Regarding gender, the two groups were similar (p=0.671) (Table 1). Dyspnea, loss of appetite, and loss of smell were significantly more common in the severe disease group (p<0.001, p=0.025, and p<0.001, respectively). The patients’ demographic, clinical, radiological, and laboratory findings are presented in Table 1.
The hospital stay duration was longer in the severe disease group (median values were 9 vs. 13 days; p<0.001). The need for intensive care was higher in the severe disease group (p=0.004). Six patients (13%) were deceased in the severe group (Table 1). C-reactive protein (CRP), D-dimer, ferritin, lactate dehydrogenase (LDH), procalcitonin, troponin, and copeptin levels were higher in the severe group (p<0.011, p<0.001, p=0.001, p=0.038, p=0.004, p=0.002, and p=0.019, respectively); besides, levels of hemoglobin, total protein, and vitamin D were lower (p=0.043, p<0.001, and p=0.029, respectively). There was no difference between the groups in terms of other hematological and biochemical markers. Laboratory findings of the patients are presented in Table 2.
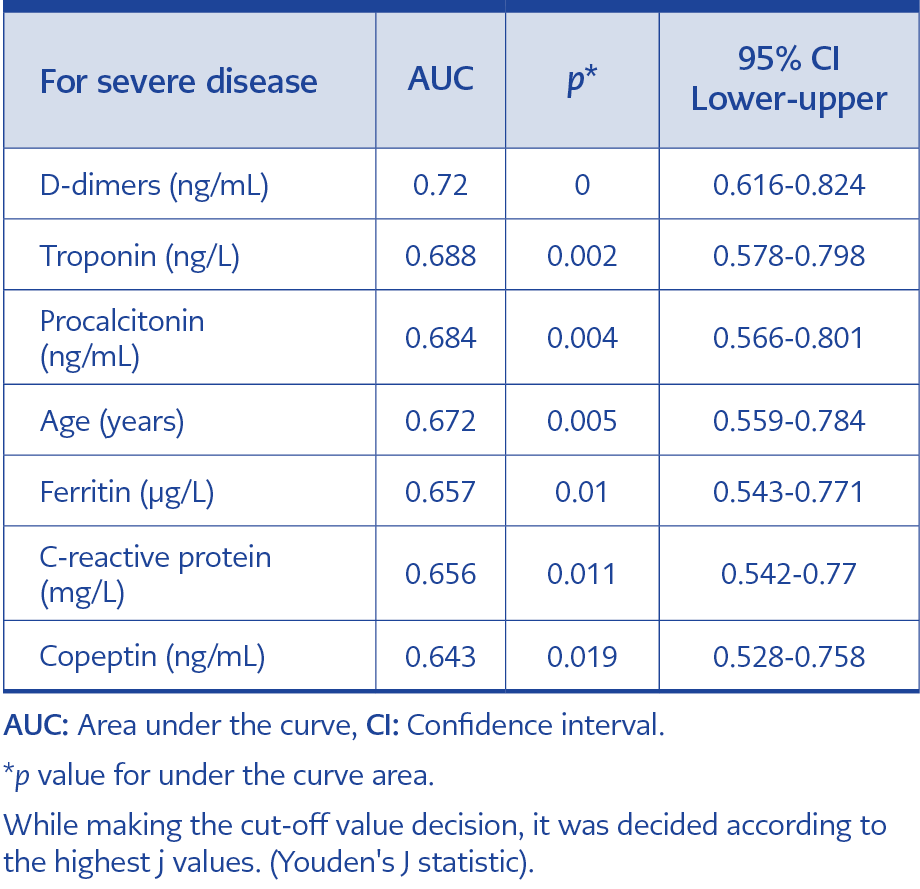
Table 3. The area under the curve values of age, copeptin, CRP, procalcitonin, ferritin, D-dimer, and troponin for severe disease.
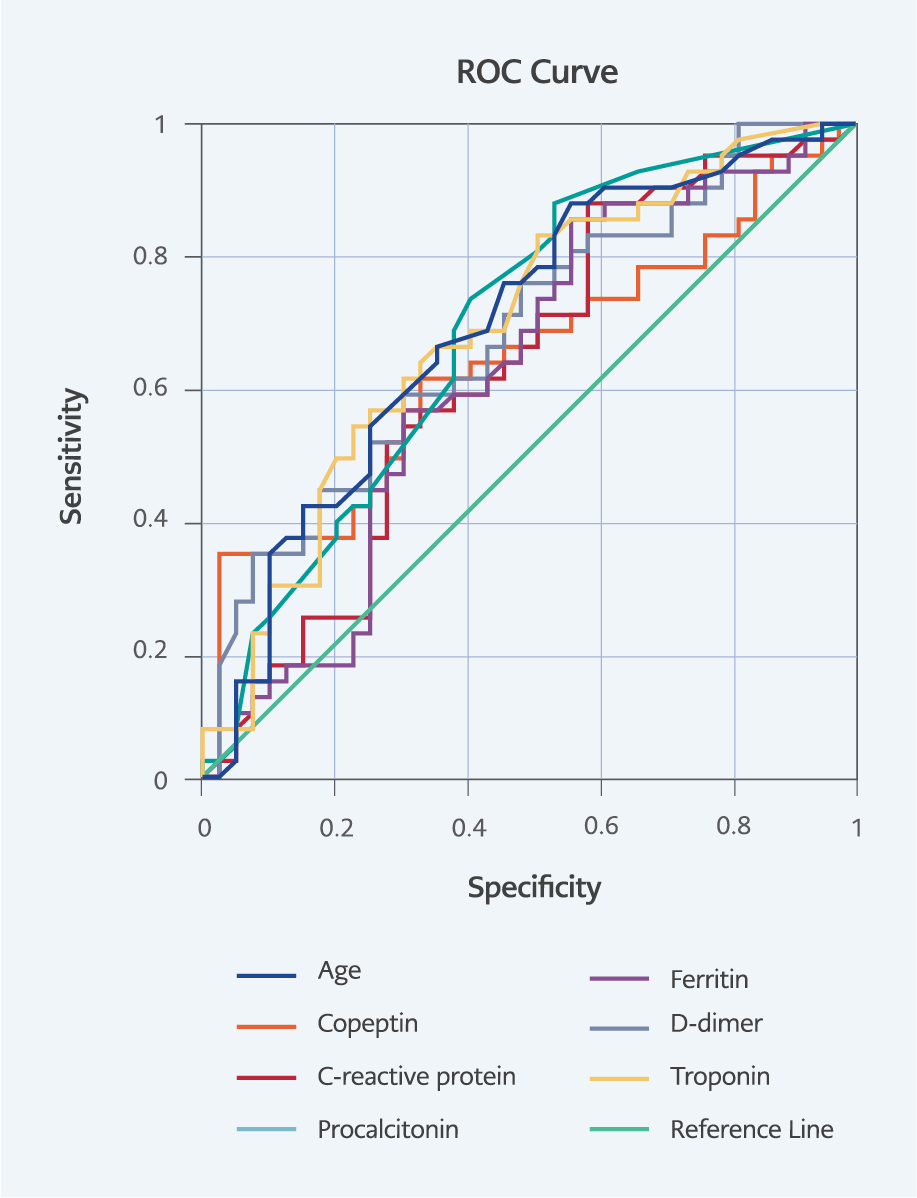
The area under the curve (AUC) was analyzed using ROC analysis for all continuous variables. The AUC values for severe disease were 0.643 (p=0.019) for copeptin, 0.656 (p=0.011) for CRP, 0.684 (p=0.004) for procalcitonin, 0.657 (p=0.01) for ferritin, 0.720 (p=0.000) for D-dimer, 0.688 (p=0.002) for troponin, and 0.672 (p=0.005) for age. The AUC values and ROC analysis results of the variables that were found to be significant for severe disease are presented in Table 3 and Figure 1.
Discussion
As a result of the activation of the hypothalamic-adenohypophyseal axis because of stress, many hormones are released, including arginine vasopressin (AVP) and cortisol. Copeptin is a biochemical mirror of AVP and is more easily detectable in serum due to its stable nature (18, 19). The inflammation, pain, lung injury, plasma osmolarity changes, and psychological stress associated with the COVID-19-induced activation of the stress-adaptive endocrine axis increase circulating AVP/copeptide. Thus, it aims to increase the absorption of free water in the kidneys and thus to provide blood pressure homeostasis through vasopressin receptors 2 (V2Rs) and to produce vasoconstriction in blood vessels through vasopressin receptors 1 (V1Rs) (6).
Lung injuries induced by COVID-19 may affect cardiopulmonary hemodynamics and left atrial underfill, followed by the activation of the renin-angiotensin-aldosterone system and the release of AVP/copeptide. This may result directly from viral or cytokine storm-induced damage (20-23). The pathophysiological mechanisms behind the emergence of inappropriate antidiuretic hormone secretion in pneumonia, as in COVID-19, have not been fully elucidated but may result from the non-osmolar release of AVP secondary to intravascular fluid depletion, which activates baroreceptors and the rennin-angiotensin-aldosterone system (20).
In our study, the relationship between the serum copeptin levels and the severity of the disease in the patients with whom we followed up regarding the diagnosis of COVID-19 was investigated, and it was demonstrated that copeptin plays a role in distinguishing between mild-moderate and severe COVID-19 patients. A limited number of studies have been conducted with copeptin in patients with a diagnosis of COVID-19. One study investigated the role of copeptin in the differentiation between community-acquired pneumonia and COVID-19 disease, and it was noted that copeptin is a useful biomarker in the differentiation of both diseases (24).
Conversely, in another study, found no difference in the copeptin levels between the patients with a diagnosis of COVID-19 and the patients diagnosed with acute or chronic bronchitis and pneumonia. In this study, serum copeptin levels in patients diagnosed with COVID-19 were found to be four times higher in non-survived patients than in survived patients. Although, in this study, copeptin was found to be effective in the clinical course, this was not specific to COVID-19, and a similar phenomenon could be observed in other respiratory tract infections (5). This demonstrates that the activation of the vasopressin system is not specific to COVID-19 but is evident in severe respiratory disease.
The role of serum copeptin and high-sensitive cardiac troponin I (hs-cTnI) on the clinical course and mortality among hospitalized COVID-19 patients was investigated, and both biomarkers were found to influence the clinical course (5). In 116 patients diagnosed with COVID-19, serum copeptin and mid-regional proadrenomedullin (MR-proADM) levels were associated with hospital complications, such as acute renal failure and sepsis. When survived and deceased patients were compared in the same study, serum copeptin levels were found to be significantly higher in patients with a diagnosis of COVID-19 who died compared to those who survived (11).
In another study demonstrating the role of copeptin in the course of COVID-19, age, copeptin, CRP, AST, ALT, LDH, ferritin, and fibrinogen were found to be significant in the differentiation of mild-moderate and severe COVID-19, and the AUC value was found to be 0.869 (p<0.001) in the ROC analysis (4). In another study, copeptin was found to be a significant biomarker in distinguishing mild-moderate and severe COVID-19 patients (6). Similarly, in our study, CRP, D-dimer, procalcitonin, troponin, and copeptin were found to be significant in the differentiation of mild-moderate and severe COVID-19, and the AUC value was determined to be 0.643 (p=0.019) in the ROC analysis.
Our study has some limitations. First, patients’ follow-up data are lacking. The importance of copeptin can be revealed more clearly if serum copeptin levels are measured during the follow-up and post-treatment period. Secondly, the number of patients is relatively small and a healthy control group was not included in the study.
In addition to the existing biomarkers, the serum copeptin level measured at the time of admission to the hospital was identified as a new useful biomarker in the differentiation of mild-moderate and severe diseases. Limited studies have examined the role of serum copeptin levels in the course of COVID-19. Understanding the role of copeptin in the course of COVID-19 is important for effective disease management and risk stratification and, ultimately, for reducing mortality due to COVID-19.