Introduction
The use of antiretroviral therapy (ART) in individuals with the human immunodeficiency virus (HIV) has significantly increased their life expectancy. Nevertheless, an increase in the frequency of chronic diseases such as diabetes mellitus (DM), hypertension (HT), and cardiovascular disease (CVD) in this population with advancing age is expected (1). Also, they are at greater risk for subclinical atherosclerosis and CVDs than people without HIV (2).
Carotid artery intima-media thickness (cIMT) is a measurement method of subclinical atherosclerosis used to predict future CVD events in the general population (3). It was demonstrated in previous studies that HIV infection is an independent risk factor for subclinical atherosclerosis (4). In many studies investigating the relationship between HIV infection and cIMT, it was shown that cIMT was higher in individuals with HIV. Several studies showed that traditional CVD risk factors become more dominant with advancing age in individuals with HIV, and the relationship between HIV and cIMT weakens in this age group (5-9). In addition, in a small number of studies conducted in the general population, a positive correlation was found between brachial artery intima-media thickness (IMT) measurement and Framingham risk score (FRS) in predicting CVD risk, and it was emphasized that brachial artery IMT could also be predictive in cardiac risk assessment (10, 11).
In this study, we aimed to investigate whether HIV infection affects carotid and brachial artery wall thickness and whether measurement of this thickness contributes to traditional cardiovascular risk scoring in individuals living with HIV.
Materials and Methods
We compared people living with HIV under ART followed in the infectious diseases clinic with a control group consisting of patients with similar characteristics who did not have HIV. The control group was selected from patients who applied to the outpatient clinic with diagnoses such as urinary tract infection, upper respiratory tract infection, or skin soft tissue infection without a diagnosis of cardiological disease. The age and gender distributions of the groups were similar. Inclusion criteria were determined as being older than 18 years of age, continuing their follow-up in our hospital, and agreeing to participate in the study. Patients who did not come for regular follow-up, had missing data, and had already experienced CVD were excluded.
Demographic characteristics of all participants, comorbid diseases, family history of heart disease, risk factors for CVD, medications, examination findings such as blood pressure measurement, body mass index (BMI), and routine laboratory tests including hemogram, biochemistry, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), lipid panel, and HbA1c were recorded. In addition to routine laboratory tests in individuals with HIV, descriptive information such as HIV RNA and CD4 T-lymphocyte values and the ART regimen used was recorded. In order to predict cardiovascular risk, the two risk scores, D:A:D score and FRS for individuals aged 30 years and above, were calculated in the patient group, while only FRS was calculated in individuals aged 30 years and above in the control group. The FRS 2008 version was calculated using variables of age, total and high-density lipoprotein cholesterol, systolic blood pressure, hypertension, smoking and diabetes status (11). According to FRS, patients were classified as low (<10%), moderate (10-20%) and high (>20%) risk. The D:A:D score was calculated by considering age, gender, total and HDL cholesterol level, smoking status, systolic blood pressure, history of diabetes, family history of CVD, and exposure to indinavir, lopinavir, and abacavir. In the D:A:D system, patients’ CVD risk was classified as low (<1%), moderate (1% to 5%), and high (≥5%) (12).
Because of the variation in CVD risk according to age and gender, the data obtained in the study were compared according to age (under 40 years old and above) and gender groups. The cIMT, brachial artery IMT and FRS data obtained in the patient and control groups were re-evaluated among these subgroups. In addition, according to the results of cIMT measurements, the patients were divided into subclinical atherosclerosis and non-atherosclerosis groups, and their data were re-evaluated in this respect. We also investigated the independent risk factors for increased cIMT and brachial artery IMT.
Ankara Yıldırım Beyazıt University Ankara City Hospital Clinical Research Ethics Committee approved the study on September 2, 2020, with decision number E1-20-919. Informed consent was obtained from all participants.
cIMT and Brachial Artery Intima-Media Thickness (IMT) Measurement
cIMT measurement was performed by the same radiologist in the radiology department of our hospital using high-resolution B-mode ultrasonography (B-USG). The ultrasound machine with software version R3 and lineer probe (11L4) (GE HealthCare, USA) was used for measurements. cIMT was measured on a longitudinal scan showing two bright lines on the posterior wall of the distal common carotid artery, 2-3 cm proximal to the bifurcation on both sides. Measurements were repeated three times for both sides, and the average values were calculated. Patients with cIMT ≥0.9 mm were considered to have subclinical atherosclerosis (13).
In the literature, there are no reference values for brachial artery IMT for determining atherosclerosis in the general population. Brachial artery IMT measurement was performed from the segment with clearly defined anterior and posterior intimal surfaces before the brachial artery branches off in the antecubital fossa. Brachial artery IMT measurements were measured three times from the far wall of the probe and averaged. In our study, the average of the results measured on the right and left sides were used as cIMT and brachial artery IMT values.
Statistical Analysis
The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 20.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics were shown as mean ± standard deviation for variables with normal distribution, median (minimum-maximum) for variables with non-normal distribution, and frequency and percentage for nominal variables. The Kolmogorov-Smirnov test was used to assess the normality assumption.
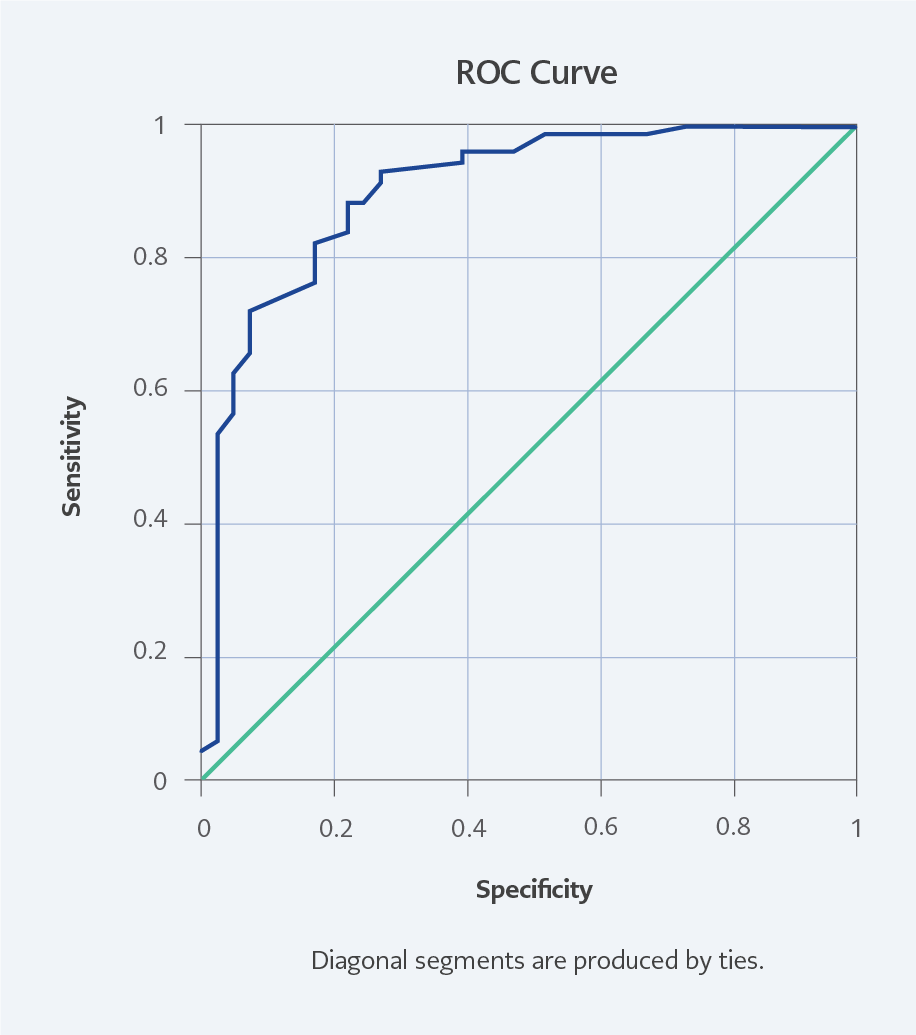
The significance of the difference between the two groups was examined using the Student’s t-test or Mann-Whitney U test. Nominal variables were evaluated with the Pearson chi-square. Univariate regression analysis was applied to determine the factors affecting cIMT and brachial artery IMT. The variables that were considered in the analyses for cIMT and brachial artery IMT were age, gender, BMI, smoking, DM, HT and living with HIV. The variables with a significance level of p-values below <0.20 from the univariate analysis were identified as candidate variables for the multivariate model. A multiple linear regression model was created with the backward method. The results were considered statistically significant when the p-value was <0.05. ROC analysis was used to evaluate the discrimination of cIMT and brachial artery IMT between patients and healthy individuals. The cut-off point was determined with the Youden index. Sensitivity and specificity values for the cut-off point were calculated.
Results
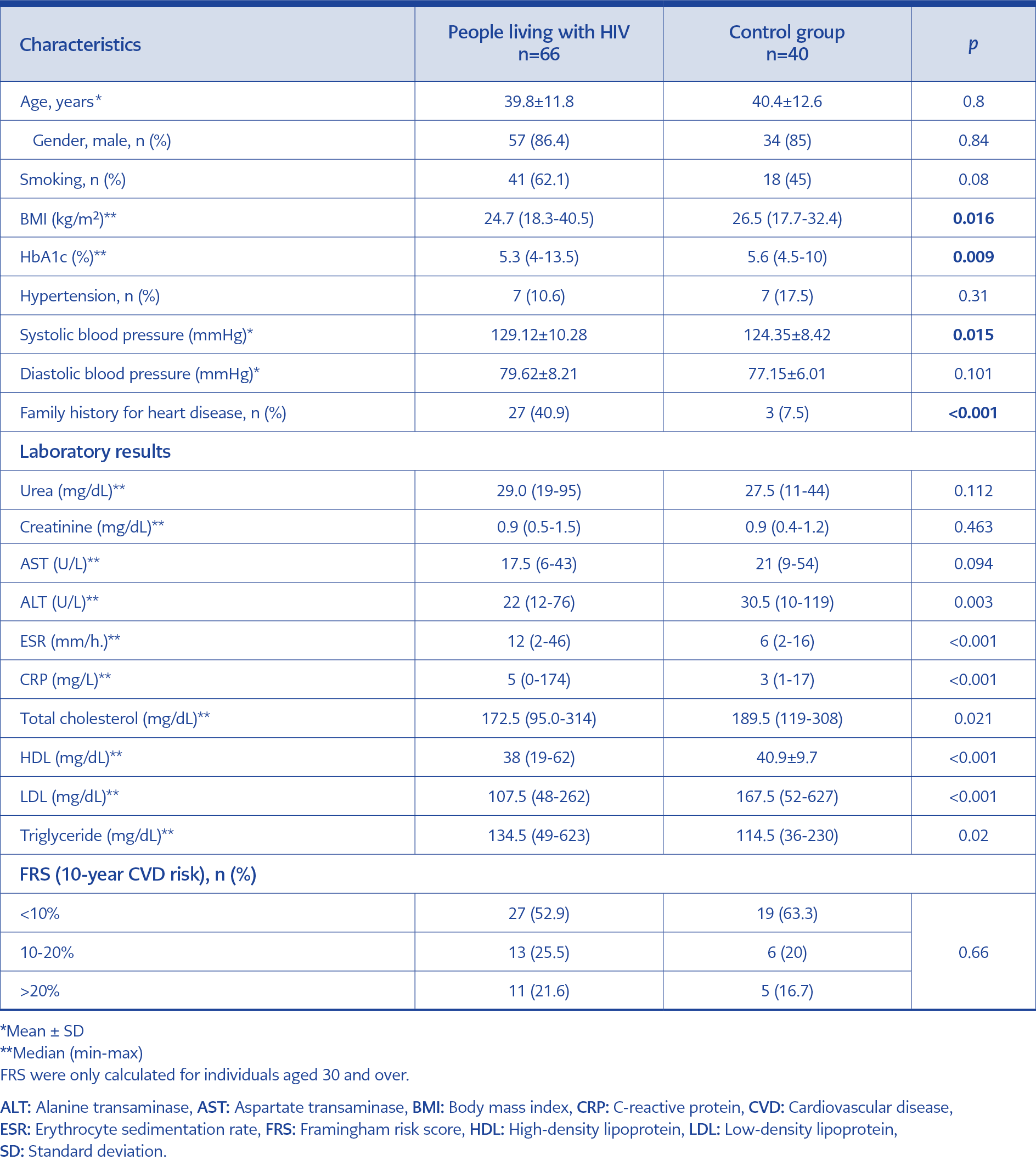
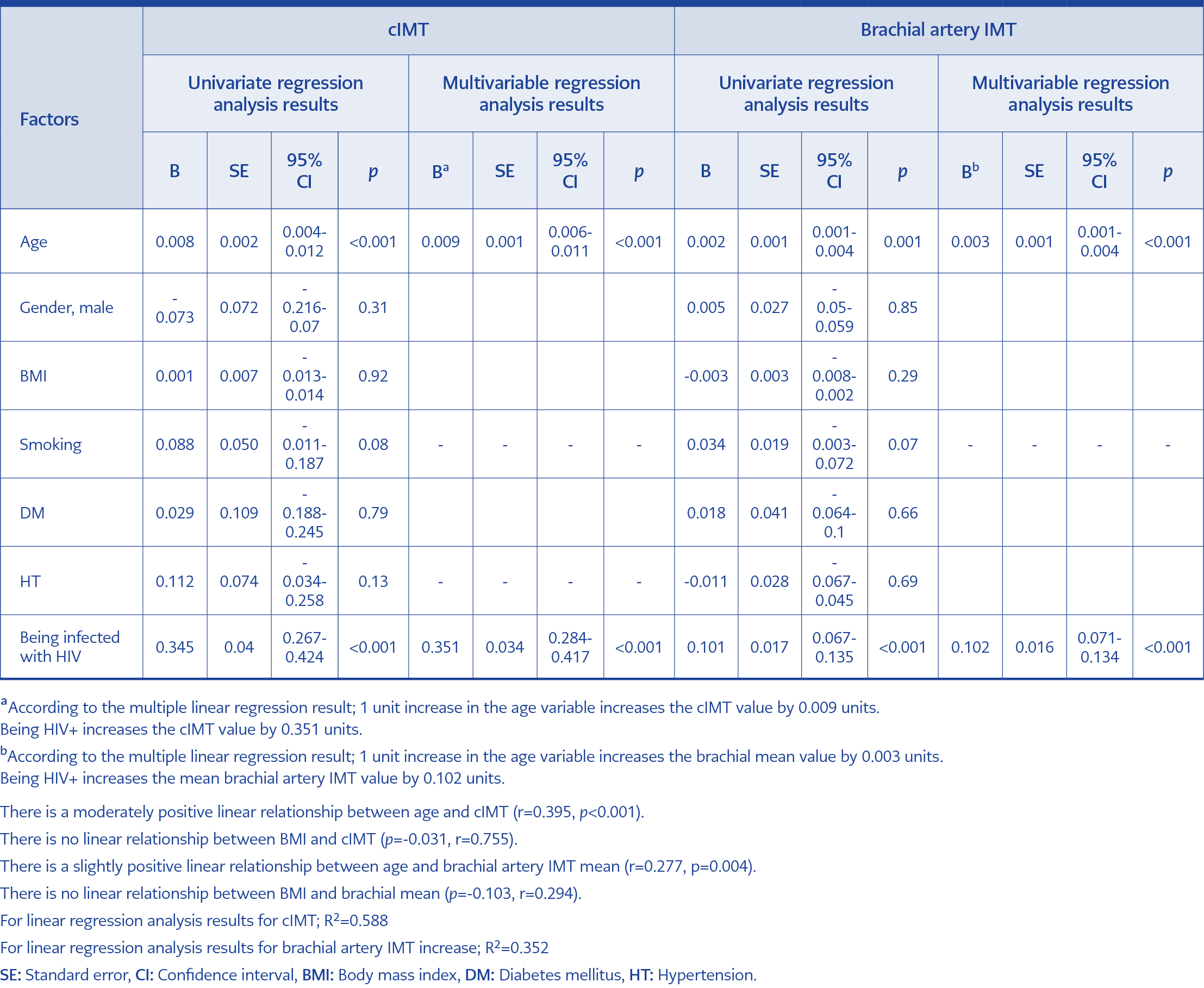
Table 1. Comparison of baseline demographic and clinical characteristics, laboratory results, and Framingham risk scores of the patient and control groups.
The patient group consisted of 66 participants living with HIV under ART, and the control group consisted of 40 participants without HIV. The mean age was 39.8±11.8 years in the patient group and 40.4±12.6 years in the control group (p=0.81). Gender distribution was similar between the groups (p=0.84). All individuals in the patient group were receiving ART and achieved viral suppression. Smoking rates of the patient and control groups were similar (p=0.085). The median BMI of the patient group was 24.7 kg/m², which was lower than the control group (p=0.016) (Table 1).
When the groups were compared in terms of cIMT measurement results, the median value of cIMT in individuals with HIV was detected to be significantly higher than the control group (0.92 [0.45-1.45] mm vs. 0.55 [0.35-1.25] mm; p<0.001). Similarly, brachial artery IMT measurement was significantly higher in the patient group (0.45 [0.30-0.76] mm vs. 0.35 [0.17-0.50] mm; p<0.001). While the rate of subclinical atherosclerosis was 57.6% in individuals with HIV, this rate was 5.0% in the control group (p<0.001) (Table 2). Atheroma plaque was present in four patients in the patient group and one in the control group. In both groups, the cIMT value of atheroma plaque was 1 mm and above. The participants’ cIMT and brachial artery IMT values were evaluated in two groups under 40 years of age and above. In the patient group, cIMT and brachial artery IMT were significantly higher among patients both under and over 40 years compared with the control group (p<0.001 for all). On the other hand, the FRS risk score distribution of the patient and control groups was similar in both age groups (p=1.0 for <40 years, and p=0.34 for 40 years and older) (Table 1).
Although the cut-off value for cIMT for detecting atherosclerosis in the general population is 0.9 mm, we found the cut-off value for cIMT in individuals living with HIV as 0.70 mm (sensitivity=0.879 specificity=0.775; p<0.001) (Figure 1). In addition, although there is no cut-off value determined in the literature for brachial artery IMT, we determined the cut-off value for detecting atherosclerosis for individuals living with HIV as 0.385 mm (sensitivity=0.818, specificity=0.675; p<0.001) (Figure 2).
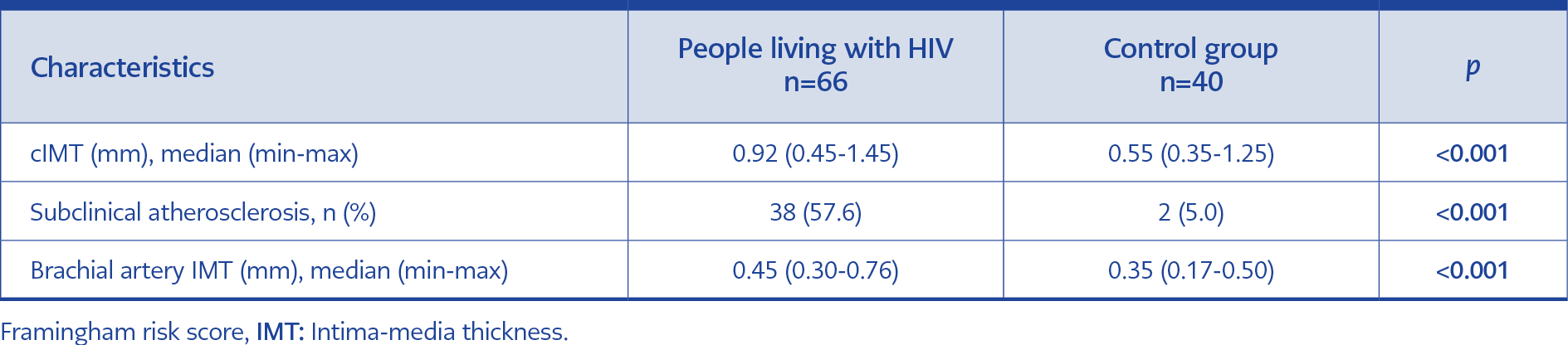
Table 2. Carotid and brachial artery intima-media thickness (IMT) measurements of the patient and control groups.
When the FRS and ultrasonographic measurement results were compared according to gender groups, the median cIMT value was 0.83 (0.45-1.17) mm in females living with HIV, while it was 0.5 (0.4-0.9) mm in females in the control group (p=0.066). The median cIMT value was 0.93 (0.55-1.45) mm in males in the patient group, while it was 0.58 (0.35-1.25) mm in males in the control group (p=0.001). Brachial artery IMT was higher in males in the patient group compared to males in the control group (p<0.001) (Table 2).
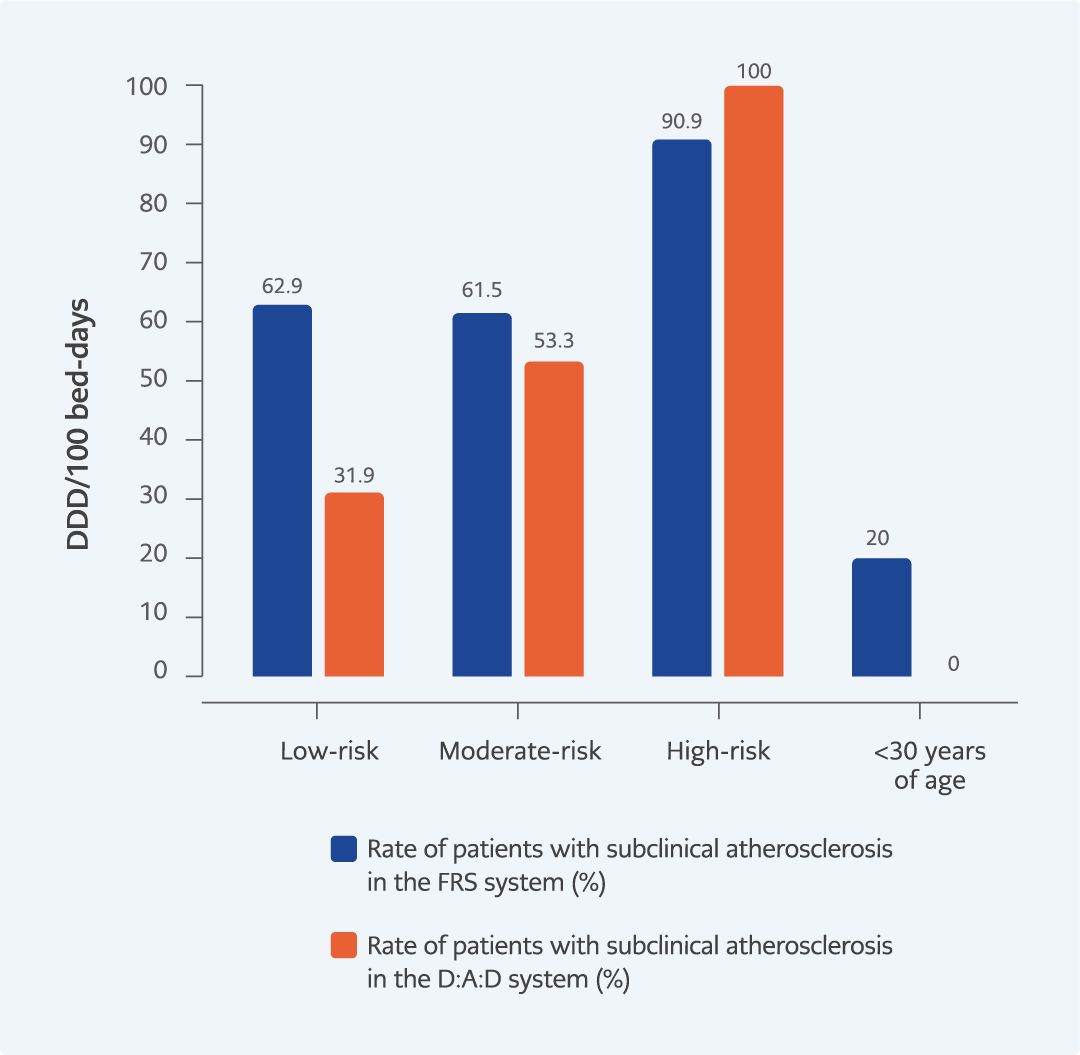
Figure 3. Subclinical atherosclerosis rates of risk groups formed according to FRS and D:A:D system in the patient group.
When individuals with HIV were evaluated within themselves, smoking rates and BMI values, disease duration, and duration of ART use were similar in the groups with and without subclinical atherosclerosis. HIV-specific parameters such as maximum HIV RNA and minimum CD4 T lymphocyte count were similar in patients with and without subclinical atherosclerosis (p=0.11 and p=0.82, respectively) (Table 3). Subclinical atherosclerosis was present in 62.9% of patients with low risk based on the FRS system and 20% of patients for whom FRS could not be calculated. When patients were divided into groups according to the D:A:D system, subclinical atherosclerosis was found in 39.1% of low-risk patients (Figure 3).
According to the results of multivariate analysis, age and HIV infection were independent risk factors for the increase in both cIMT and brachial artery IMT (Table 3). It was determined that living with HIV increased the cIMT value by 0.351 (95% CI=0.28-0.42) mm (p<0.001) and the brachial artery IMT value by 0.102 (95% CI=0.07-0.13) mm (p<0.001).
Discussion
Besides increased life expectancy, comorbidities are more common in individuals living with HIV compared to the uninfected population (14), and cardiovascular diseases take the first place among comorbidities (15-17). Detection of subclinical atherosclerosis before end-organ damage due to atherosclerosis occurs is an effective method for preventing important diseases, especially CVD (18, 19). The rate of calcification in atherosclerotic plaques is lower in patients with HIV infection than in patients without HIV, and these plaques are more prone to rupture (20, 21). Hence, the detection of subclinical atherosclerosis is of greater importance in individuals with HIV than in the population without HIV to prevent future complications.
Endothelial dysfunction and LDL oxidation by passing under the endothelium are the basic mechanisms that initiate the atherosclerosis process. In individuals with HIV, ongoing chronic inflammation poses an extra risk for atherosclerosis (21). Although LDL was higher in our control group, the higher cIMT value in the patient group suggested that endothelial damage resulting from HIV-related inflammation was a more effective mechanism than dyslipidemia in the pathogenesis of atherosclerosis.
In most studies, cIMT was found to be significantly higher in individuals with HIV (4-11). Consistent with the literature, we found that cIMT values were higher in people living with HIV compared to the control group. While some of the clinical and laboratory findings, accepted as the risk factors for CVD, were in favor of the patient group, some of them were in favor of the control group. These data supported the view that the high cIMT value in people living with HIV could not be explained only by other risk factors for CVD (17, 22). In multivariate regression analysis, only increasing age and living with HIV were found as independent risk factors for increased cIMT. These findings show that HIV infection is more determinant in increased cIMT and subclinical atherosclerosis.
The increased cIMT and higher rate of subclinical atherosclerosis can be explained by the ongoing chronic inflammation associated with HIV infection (21). Supportingly, inflammation markers (CRP and ESR) were significantly higher in people living with HIV than in the control group. However, in the study, although inflammation markers were higher in the patient group than in the control group, no difference was found between patients with and without subclinical atherosclerosis. Considering the importance of inflammation in the pathogenesis of atherosclerosis, CRP and ESR would be expected to be higher in the group with subclinical atherosclerosis. Our study’s low number of patients with and without subclinical atherosclerosis may have caused such incidental results. In addition, ESR and CRP are only two of the markers of acute inflammation. Other inflammatory markers, such as microbial translocation markers (16S ribosomal DNA and sCD14 and sTNFRI, IL-6, TNF-α) that we could not measure in this study might have played an important role in inflammation. If these markers could be measured, the difference between groups with and without subclinical atherosclerosis could have been more clearly demonstrated.
It is known that the risk of atherosclerosis and cIMT, an indicator of atherosclerosis, increase with age. The groups were re-evaluated as under and over 40 years old, and cIMT and brachial artery IMT were found to be higher in the patient group in both age groups. The median cIMT was 0.83 mm in people living with HIV under the age of 40, close to the subclinical atherosclerosis border. High cIMT levels detected at an early age indicate that individuals living with HIV are at risk for atherosclerosis development from an early age. Another risk factor for CVD is the male gender (23). When the results of cIMT were compared among gender groups, cIMT was higher among men living with HIV compared to the control group among male participants; the absence of such a difference among women indicates that the relationship between HIV infection and atherosclerosis is stronger in men than in women.
In our study, FRS and D:A:D scores were calculated to examine the CVD risk. According to the FRS system, the risk distribution of the patient and control groups was similar. While the FRS categorization evaluated according to age (30-39 years and ≥40 years) between the patient and control groups could not detect a difference between the two groups, the measured cIMT values revealed that individuals living with HIV were at higher risk for the development of atherosclerosis. Especially although individuals living with HIV appear in the low-risk group according to FRS at an early age, our results revealed that they had higher cIMT values. Even those under the age of 30, in whom FRS cannot be calculated, had a higher cIMT. Considering that the majority of the population with HIV worldwide consists of young adults, the HIV-cIMT relationship, which is more pronounced in the male gender, reveals the contribution of cIMT measurement to traditional risk scoring.
One of the important results of our study was the detection of subclinical atherosclerosis in 62.9% of the patients who fall into the low-risk group, according to the FRS system. The most important contribution of cIMT measurement emerges in the low-risk group. The contribution of cIMT measurement to FRS has been investigated in several studies in the general population. Although it is not thought to have a significant contribution according to the previous studies, in our study, subclinical atherosclerosis was detected with cIMT in more than half of the patients in the low-risk group in individuals living with HIV (24-27). Besides, the detection of subclinical atherosclerosis in 20% of individuals for whom FRS could not be calculated revealed the power of IMT in this group. Considering the groups classified according to the D:A:D score, although the detection of subclinical atherosclerosis in 39.1% of the patients in the low-risk group showed that the D:A:D system was superior to the FRS in predicting the CVD risk, D:A:D still missed a large number of the patients with a substantial CVD risk, and these patients appear to be detectable only with cIMT. In the control group, the probability of being overlooked in terms of subclinical atherosclerosis seems to be very low in people with low risk, according to FRS. The reason for this is that the chronic inflammatory state in individuals living with HIV is ignored in systems such as FRS and D:A:D (11, 28). Therefore, the contribution of cIMT measurement to the classical risk scoring systems in individuals with HIV at early ages is an expected result that is more pronounced in low-risk groups.
Recently, it was investigated whether brachial artery IMT measurement can be used as a predictor of atherosclerosis. Studies investigating the relationship between brachial artery IMT and atherosclerosis are limited in the literature (10, 29, 30). In our study, the brachial artery IMT was significantly higher in the patient group, which was expected to have a high risk of CVDs. The similarity between carotid and brachial artery IMT measurement results suggests that brachial artery IMT measurement can also be used to determine atherosclerosis burden in individuals living with HIV. In the literature, there are no reference values for brachial artery IMT for determining atherosclerosis in the general population; our study will contribute to the available literature in this field. Additionally, we determined new cut-off values for cIMT and brachial artery IMT for determining atherosclerosis in individuals living with HIV. Measurement of brachial artery IMT in individuals with HIV and reevaluation of cIMT and brachial artery IMT in age and gender subgroups make our study powerful. Another strength of our study is the comparison between classical risk estimation scores and carotid and brachial IMT values to determine the best method for estimating CVD risk.
Our study had several important limitations. First, since it coincided with the COVID-19 pandemic, there were disruptions in outpatient follow-ups, and the predicted number of patients could not be reached. Besides, the relationship between CVD risk scores, carotid and brachial artery IMT measurements and the development of cardiovascular events in the follow-up of the patients could not be examined because the long-term follow-up results had not been performed. Also, the R2 value for linear regression analysis results for brachial artery IMT increase was 0.352. This low value should be supported by larger studies with more participants.
In conclusion, the fact that the relationship between HIV and cIMT is more significant in the male gender. Furthermore, the CVD risk in patients whose FRS cannot be calculated or who have a low FRS can be determined only by cIMT, showing that cIMT measurement is a very advantageous way of estimating CVD risk in people living with HIV, predominantly in males and young adults. The use of carotid and brachial artery ultrasonography, which is a non-invasive, inexpensive and easily applicable method, in individuals living with HIV will help in the early detection of patients at risk for CVDs and taking necessary precautions, minimizing cardiovascular events that may develop during the follow-up of patients.