Introduction
Surgical site infections (SSIs) are a significant global problem, and their burden increases with emerging antimicrobial resistance. Globally, around 12.3% of surgical patients suffer from SSIs annually, with higher rates in low-income countries (23.2%) compared to high-income countries (9.4%) (1). Inappropriate antibiotic use not only escalates the rate of antimicrobial resistance but also leads to unnecessary costs and potential side effects (2-5).
The American Society of Health-System Pharmacists (AHSP) established the standards for surgical antibiotic use in 2013, with the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) strongly recommending against the postoperative continuation of prophylactic antibiotics in 2016 and 2017 (6-8). Despite these clear recommendations, the prevalence of prolonged prophylactic antibiotic use in surgical operations (>24 hours) ranges from 29.5% in developed countries to 92.5% in Africa (9). The evidence supporting the need for postoperative continuation to reduce SSIs is limited (4).
This study aimed to achieve the following objectives: 1) enhance compliance with the local surgical prophylaxis guideline, 2) reduce unnecessary antimicrobial consumption before and after surgery, and 3) monitor the long-term impact of these interventions.
Materials and Methods
This study was conducted at a non-profit foundation hospital prospectively in İstanbul with a 300-bed capacity spanning from 2011 to 2022. In December 2014, a local surgical prophylaxis guideline (LSPG) was developed for all surgical patients based on the current AHSP guideline (7). The primary objective of the LSPG was to reduce the misuse and excessive consumption of antibiotics both before and after surgery.
The LSPG outlined several key rules as follows:
- The prophylactic antibiotic should be selected from the LSPG.
- The prophylactic antibiotic should be administered within 60 minutes before the incision and discontinued within a maximum of 24 hours. The duration of prophylactic antibiotic use was calculated based on the time between the first and last dose.
- In cases where the operation duration exceeds two times the half-life of the prophylactic antibiotic, a repeat dose should be administered during the operation.
The Infection Control Team (ICT) closely monitored the thoracic surgery team’s compliance with the LSPG, specifically focusing on single-dose or a maximum of 24-hour cefazolin antibiotic prophylaxis, excluding drainage operations. Monthly evaluations of each surgical antibiotic prophylaxis intervention were conducted in conjunction with the thoracic surgery team.
The study compared all antibiotic prophylaxis procedures applied before (between January 1, 2011, and December 31, 2014) and after (between January 1, 2015, and December 31, 2022) the implementation of the LSPG intervention among thoracic surgery patients. The impact of the LSPG intervention on the rate of SSIs and the appropriateness of antibiotic selection in terms of type, dose, and duration was evaluated. Descriptive statistics were presented with mean, standard deviation, and percentages. Bivariate analyses were conducted by Chi-square tests. The statistical significance was set as p<0.05.
Results
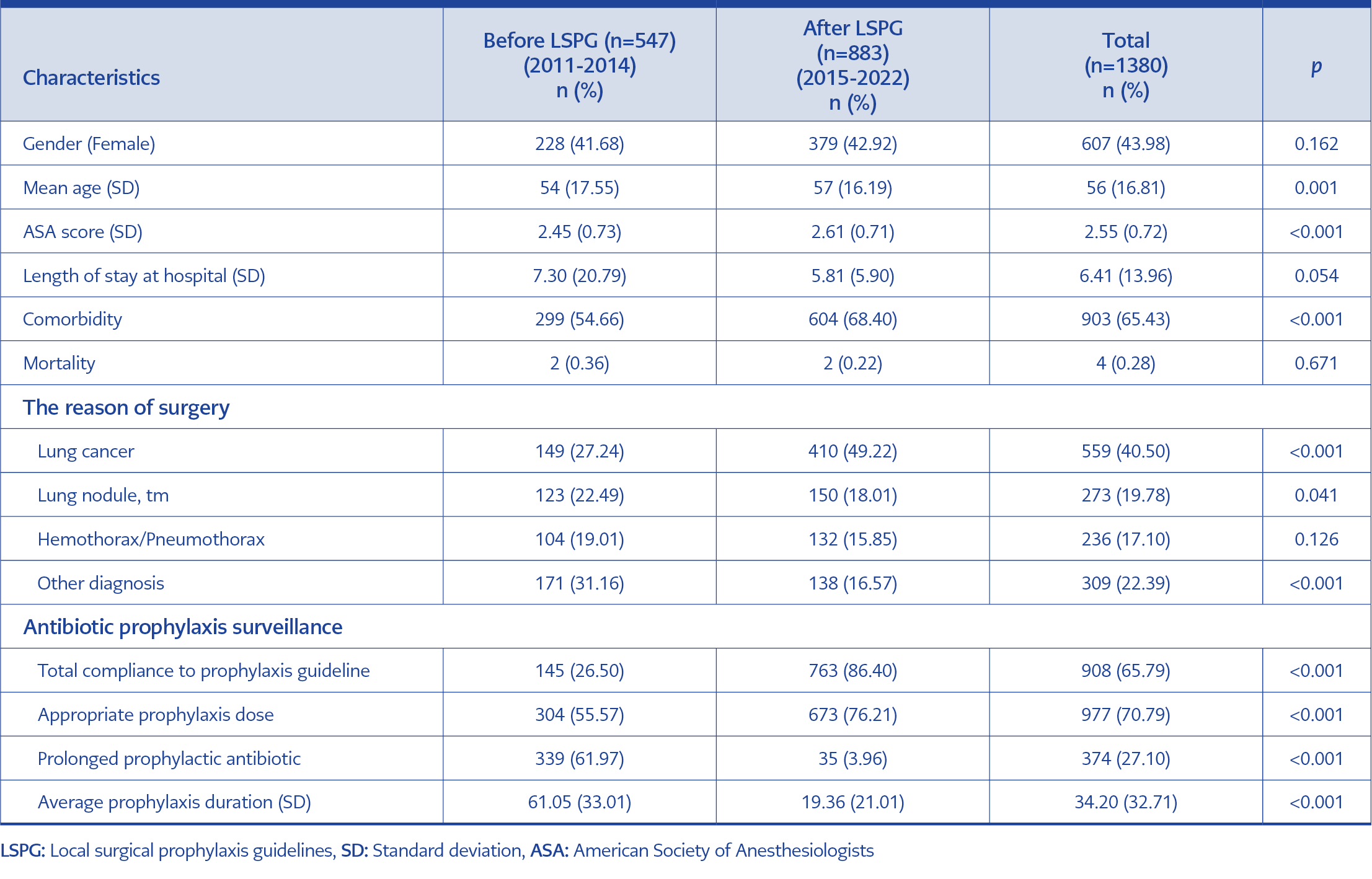
Table 1. The characteristics and the antibiotic prophylaxis details of the study group before and after LSPG.
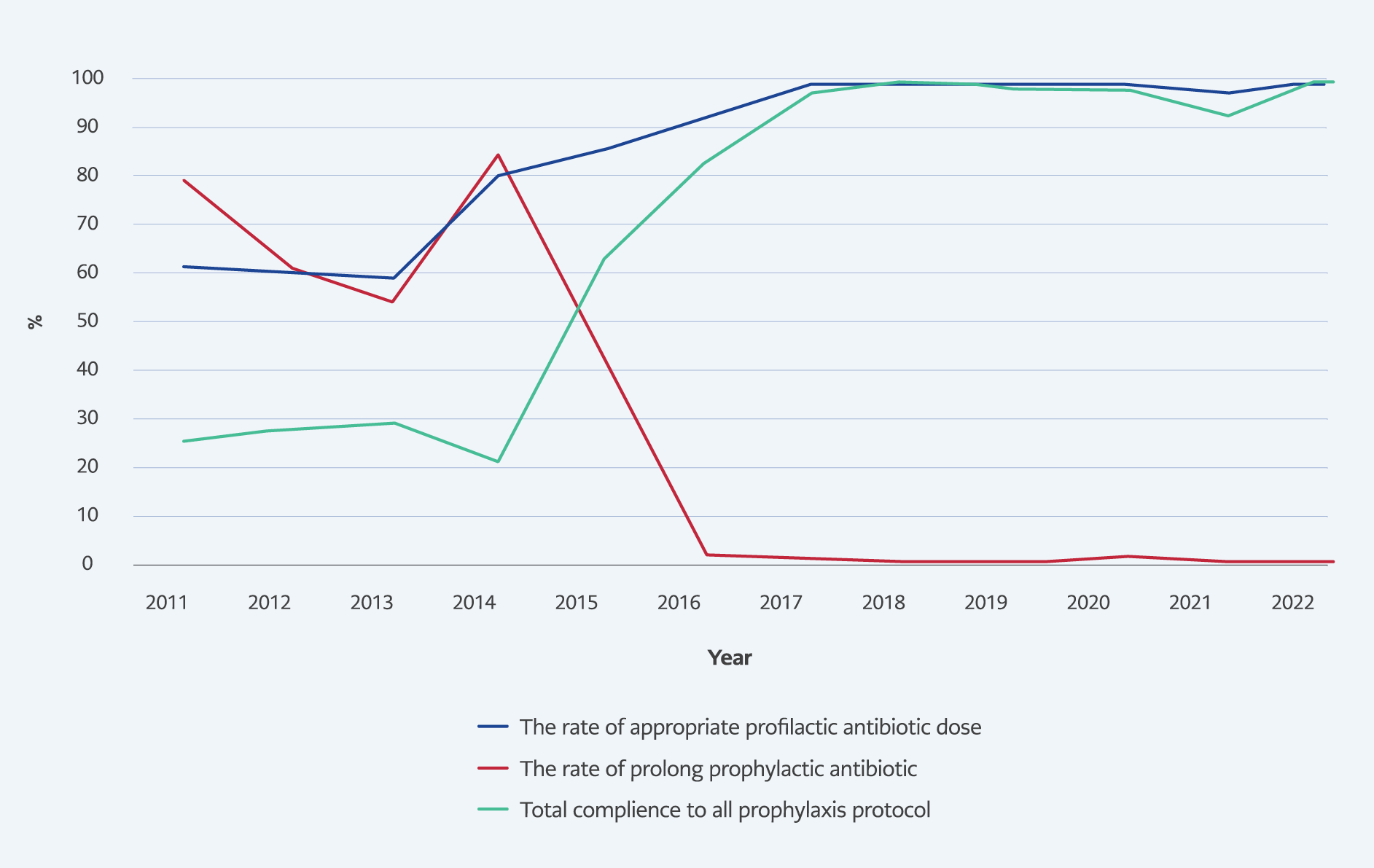
Figure 1. Appropriate antibiotic dose, prolonged prophylaxis (>24 h) and total compliance with all antibiotic prophylaxis protocols over the years.
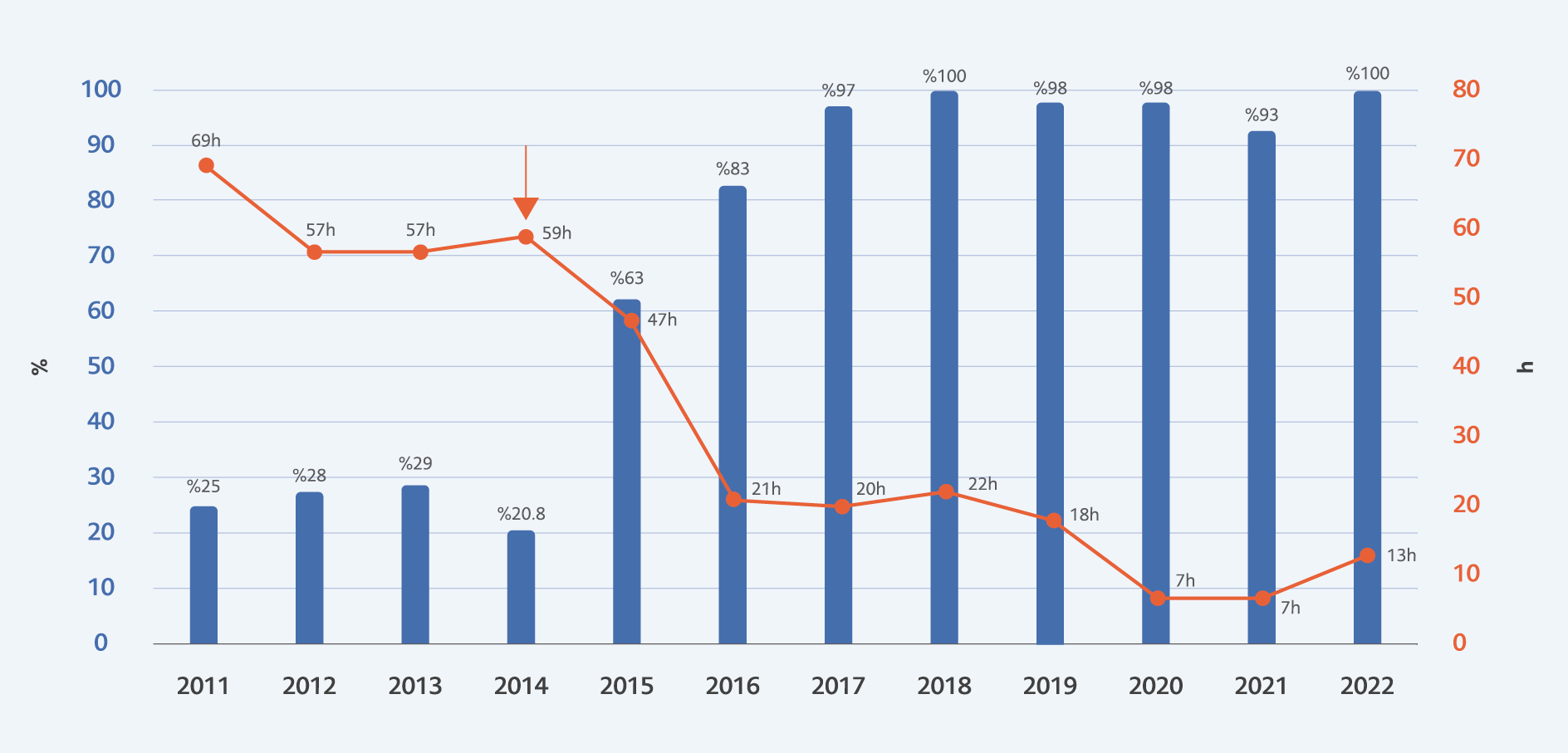
Figure 2. The rate of appropriate prophylactic antibiotic use and prophylactic antibiotic duration (hours) before and after LSPG.
A total of 1380 surgical prophylaxis practices performed by the thoracic surgery team between January 1, 2011, and December 31, 2022, were evaluated. Among these, 44% of the patients were women (n=607), with a mean age of 56 years (SD=16.81; range=2-100 years). Notably, 65.43% of the patients had at least one chronic disease (n=903), and the mean American Society of Anesthesiologists (ASA) score was 2.55 (SD=0.72). The average length of hospital stay was 6.41 days (SD=13.96). In terms of the reason for surgery of patients, 40% of patients had lung cancer, 20% presented with lung nodules or tumors, and 17% had hemothorax/pneumothorax (Table 1).
Implementation of the LSPG significantly improved the overall appropriate prophylactic antibiotic practice rate (choice, dose, and duration) from 26.50% to 86.40% (min:25%, max:100%), (p<0.001) (Table 1, Figure 1-2). Moreover, the rate of appropriate antibiotic prophylaxis dose increased from 55.57% to 76.21% (p<0.001) (Table 1), while the occurrence of prolonged antibiotic prophylaxis decreased from 61.97% to 3.96% (Table 1, Figure 1).
Additionally, the mean duration of antibiotic prophylaxis decreased from 61.05 hours to 19.36 hours (max:69 h, min:7 h) over the 12-year study period (p<0.001) (Table 1, Figure 2). Despite these interventions placed on antimicrobial prophylaxis before and after surgery, no cases of SSI were reported during both periods. Furthermore, the mortality rate remained unchanged (p=0.671), and the length of hospital stay showed a decreasing trend, although not statistically significant (p=0.054), with the mean length of stay reducing from 7.3 days to 5.8 days (Table 1).
Discussion
The results of this study provide valuable insights into the impact of prolonged prophylactic antibiotic restrictions on SSIs in thoracic surgery patients in a country with a higher rate of SSIs caused by multidrug-resistant pathogens. Current literature supports the use of prophylactic antibiotics to reduce the rate of SSIs, with some exceptional cases (10, 11), but emphasizes the importance of limiting its use to a maximum of 24 hours. Prolonged antibiotic prophylaxis has been shown to give no additional benefits compared to discontinuation (4). Zay Ya et al. proved that antimicrobial stewardship programs were associated with reducing the consumption of antibiotics (12). Batlle et al. conducted a study in surgery departments, and they got similar results (13). Moreover, Díaz-Madriz et al. asserted that effective antimicrobial stewardship increases the rate of appropriate prophylactic antibiotic selection and the percentage of optimal duration, with no severe surgical site infection and severe adverse reaction (14).
Despite these studies, compliance with current prophylaxis practices appears to be relatively low, with some studies reporting that compliance rates are as low as 8% globally and also in Turkey (9, 15). The reasons for inappropriate antimicrobial consumption among physicians could be related to the lack of education of physicians and the population, lack of political will, poor implementation of stewardship programs, and lack of access to laboratory services (16). However, this study’s findings demonstrate a remarkable improvement in compliance with current guidelines through the implementation of the LSPG.
Upon adopting the LSPG recommendations in 2015, the total compliance with the guideline reached 100% (Figure 1, Figure 2), and the mortality rate remained unchanged over the 8-year period (from 2015 to 2022) (Table 1). Furthermore, no SSI cases were detected both before (2011 to 2014) and after (2015 to 2022) the implementation of LSPG. The study also compared antibiotic duration, appropriate dose, and overall compliance with LSPG before and after its practice. Remarkably, the implementation of LSPG resulted in a significant reduction in prophylactic antibiotic duration, from an average of 61 hours to 19 hours (p<0.001), and an increase in the rate of appropriate prophylactic antibiotic doses from 55% to 67% (p<0.001). The overall compliance rate with LSPG significantly improved from 26% to 86% (p<0.001) after its implementation (Table 1).
Furthermore, a comparison of patient characteristics between the two groups (before and after LSPG practice) revealed interesting differences. Patients in the “after” group were found to be older (57 vs. 54 years; p=0.001) and had a higher prevalence of comorbidities (68% vs. 54%; p<0.001) compared to the previous patient group. Conversely, the previous group had a lower ASA score (2.45 vs. 2.61; p<0.001). Despite the potentially higher risk profile in the “after” group, the successful implementation of LSPG resulted in positive outcomes in terms of SSIs and compliance rates.
The rate of prolonged antibiotic use in Türkiye was reported as 91.7% (15), aligning with findings from other regions with varying rates reported in the literature, ranging from 29.5% in developed countries to 92.5% in Africa (9). This highlights the significance of interventions like LSPG to improve antibiotic usage practices and combat the growing threat of antimicrobial resistance.
As a result of this study, it is evident that compliance with current prophylaxis guidelines does not increase the risk of SSIs or mortality. On the contrary, adherence to LSPG or discontinuation of prolonged surgical prophylaxis can lead to reduced hospital length of stay and decreased antibiotic consumption. This, in turn, can mitigate the economic burden, the risk of antimicrobial resistance, and the unseen side effects associated with antibiotic usage over time. However, it is essential to acknowledge that this study’s limitations include focusing on a specific surgery patient group in a single center, which may not fully represent all surgery patient groups. However, we presented moderate to strong evidence for the implementation of the antimicrobial stewardship programs for surgical prophylaxis.
In conclusion, we demonstrated the importance of adhering to current guidelines and discontinuing prophylactic antibiotics beyond the recommended timeframe to effectively prevent SSIs in a region where the prevalence of multidrug resistance is high. With proper implementation of LSPG, we observed that compliance rates with appropriate antibiotic use significantly increased, with no cases of SSIs during the study period.