Introduction
Aspergillus spp. are ubiquitous and frequently inhaled by humans as spores in the natural environment and hospital settings. Despite this high frequency of exposure, aspergillosis is a rare disease in humans. Many Aspergillus spp. have been defined as causing infections, including Aspergillus fumigatus and Aspergillus flavus, among the most common Aspergillus spp. (1). Invasive aspergillosis (IA) frequently occurs in immunocompromised hosts, and these patients generally have several risk factors, including neutropenia (severe and prolonged) and receipt of immunosuppressive drugs. IA manifests in a variety of infections, particularly in pulmonary disease. It can also less commonly spread to other body parts, such as the skin, brain, and liver. In recent years, several studies have indicated a general increase in the incidence of invasive pulmonary aspergillosis (IPA) in patients with hematological disorders, with the condition responsible for substantial morbidity and mortality in these populations. Therefore, diagnosing and treating immunocompromised patients as early as possible is important. Voriconazole is the main drug of choice for IPA, but amphotericin B (AmB) is also used in febrile neutropenia and some specific conditions. It does not interact with drugs typically used in patients with hematological malignancies and does not show significant in vitro / in vivo resistance in molds and yeasts (5). Despite being one of the first-line antifungal drugs used for IPA for 50 years, the success rate of AmB in these patients remains unsatisfactory (6). In this report, we present two cases of IA that were resistant to AmB.
Case 1
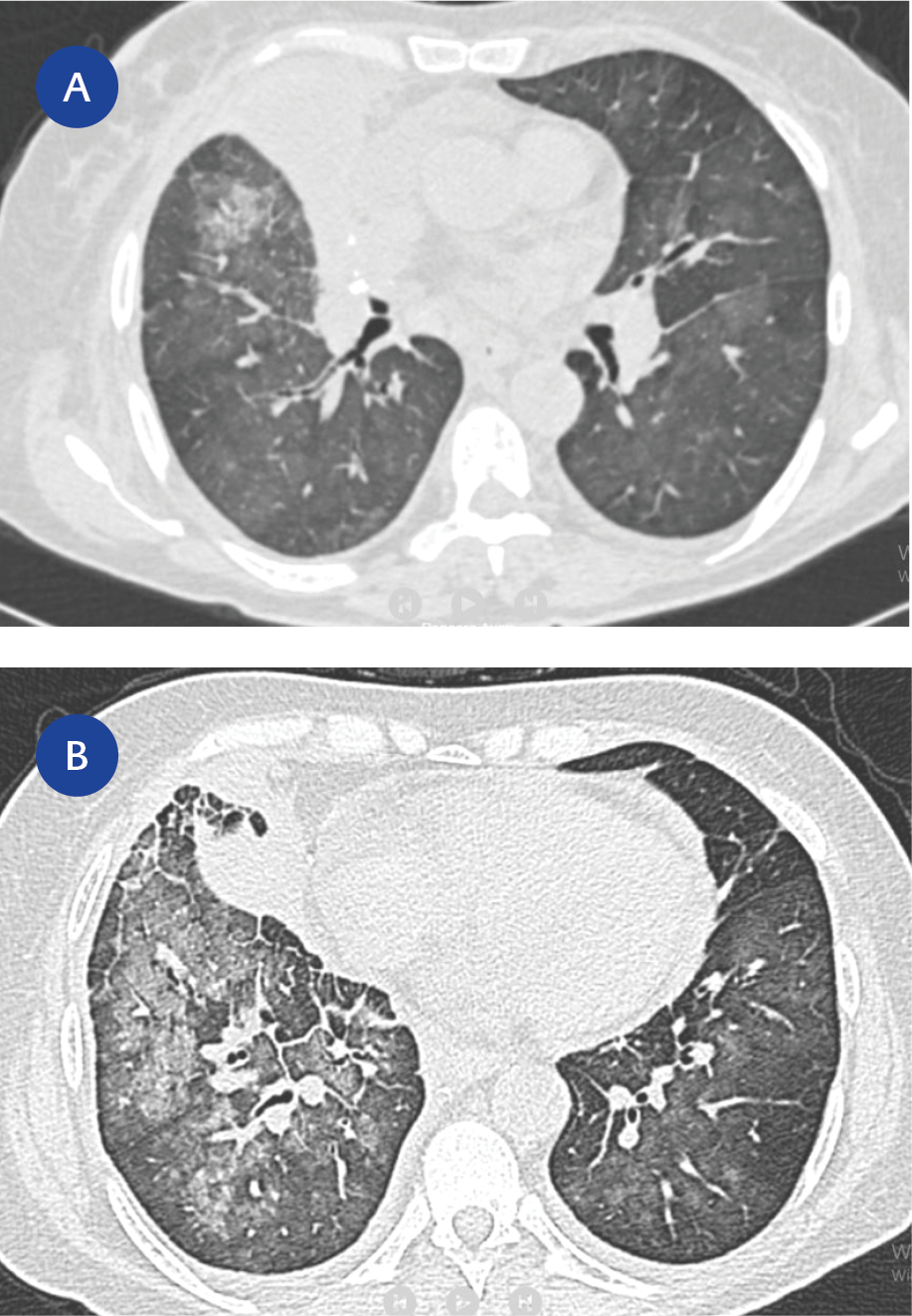
Figure 1. (A) Showing a consolidation near the lobectomy under the FNA. (B) Showing the consolidation spreading all lobes.
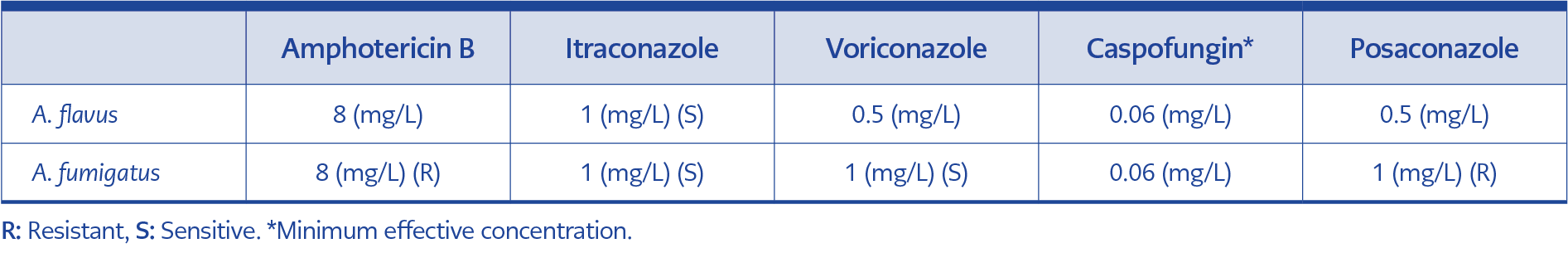
Table 1. Broth microdilution for antifungal susceptibility results by utilizing the EUCAST methodology.
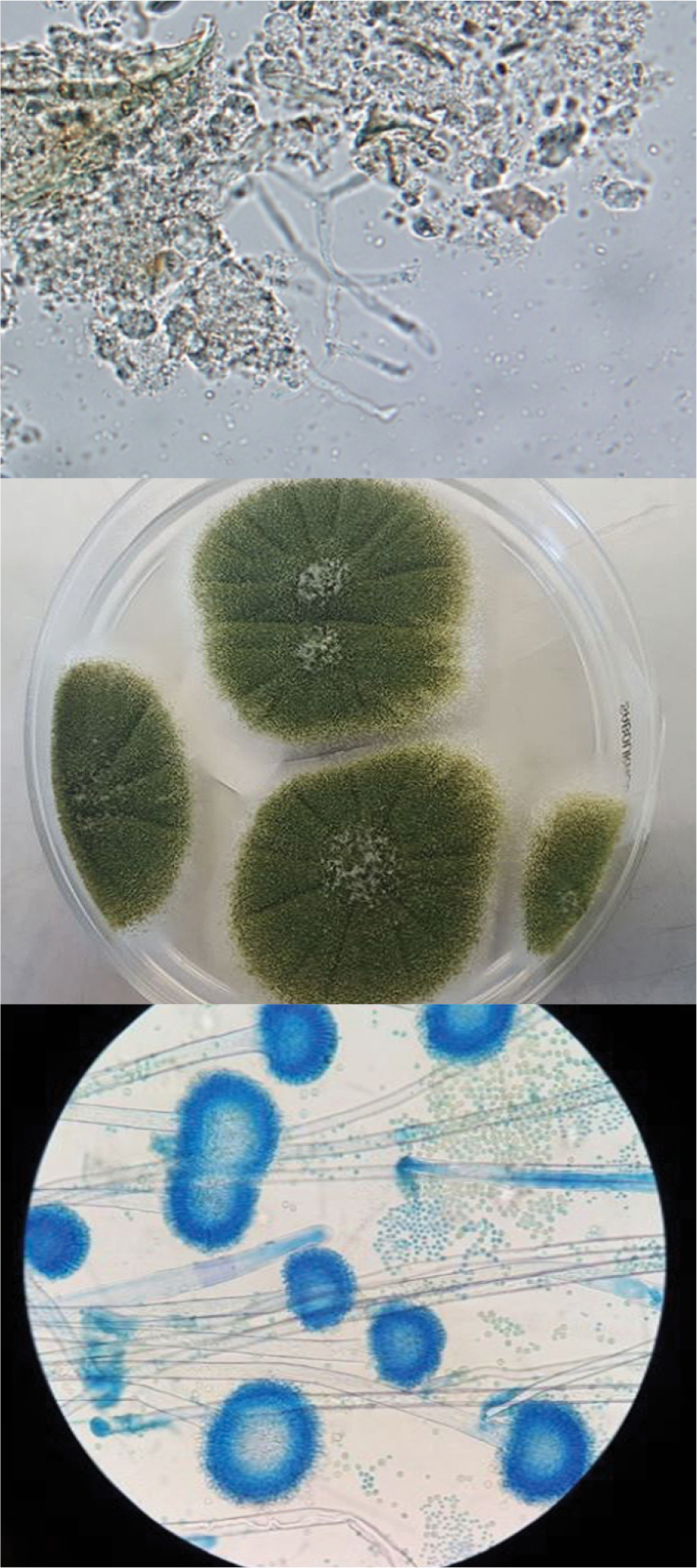
A 53-year-old female diagnosed with acute myeloid leukemia presented with a febrile neutropenic attack (FNA) after chemotherapy; she was empirically given piperacillin-tazobactam. Previously, she was administered 3 + 7 (idarubicin + cytarabine), had a complete response, but relapsed after six months, then received FLAG-Ida (fludarabine + cytarabine, idarubicin), lost its response and never in remission again. Her medical history included a left lower lobectomy for aspergilloma, and oral voriconazole was continued for possible residual lesions. On the fifth day of FNA, she did not respond to the antibiotic, and a computed tomography scan was performed. Following the preliminary diagnosis of probable IPA, liposomal amphotericin B (L-AmB) at a dose of 5 mg/kg once daily was added to the treatment regimen, and galactomannan (GM) testing using Platelia Aspergillus Ag (Bio-Rad Laboratories Inc., France) was negative during this period. However, the fever persisted. Enterococcus spp. was isolated from the hemoculture, prompting the addition of vancomycin to the therapeutic regimen. Despite the administration of 21-day L-AmB, the patient remained febrile and neutropenic. Subsequently, she developed hemoptysis and then cough and sputum. Her general condition deteriorated acutely. A repeat CT demonstrated the presence of diffuse glassy densities on all lobes, with an increase in the size of the right pleural effusion and the development of a new effusion in the left lung (Figure 1). Piperacillin tazobactam was discontinued, and meropenem plus colistin was administered. In these periods, the results of the cytomegalovirus polymerase chain reaction (PCR) and GM tests were negative. Subsequently, the patient’s respiratory distress was exacerbated by the development of cardiac arrest. Following the cessation of 28 days of L-AmB, the combination of caspofungin and voriconazole (the loading dose was 6 mg/kg twice daily, followed by 4 mg/kg twice daily) was initiated. No relevant drug-drug interactions were determined. The patient was later transferred to the intensive care unit (ICU). On the culture of endotracheal aspirate (ETA), leukocytes and abundant hyphae were observed on gram staining, and an A. flavus species complex was identified (Figure 2). The GM test results were found to be positive (>10 index) in the last consecutive sera. The fungus was resistant to L-AmB (Table 1). The patient ultimately succumbed to her illness in the ICU within two days.
Case 2
A 49-year-old male with T-cell-rich B-cell lymphoma was initially treated with eight cycles of R-CHOP (R-CHOP – Rituximab [R], Cyclophosphamide [C], Doxorubicin hydrochloride [H], Vincristine sulfate [O], Prednisone [P]) in 2006. However, he relapsed in 2009. An autologous stem cell transplant was performed in 2011, but he did not attend medical appointments until 2016. The disease relapsed in 2016, and the patient was subsequently given chemotherapy, including gemcitabine-cisplatin-dexamethasone, as a salvage regimen. He had severe neutropenia and developed a fever. He was primarily considered FNA, so two sets of hemocultures were drawn, and piperacillin-tazobactam was empirically administered. Despite antibiotics, the fever persisted, and GM tests were negative during these periods. CT showed multiple consolidations in the right lung and a 25 mm nodule in the left lung. L-AmB was added to the antibiotic regimen due to these findings and persistent high fever. After 14 days of L-AmB therapy, the patient’s general condition deteriorated, resulting in hypotension. He was subsequently transferred to the ICU. Piperacillin-tazobactam was stopped, and meropenem, amikacin and vancomycin were initiated. Two days later, multiple rashes compatible with ecthyma gangrenosum appeared on different parts of the skin (Figure 3). The histological examination of the biopsy specimen revealed the presence of multiple leukocytes and hyphae. GM test results were found to be positive (>4.6 index) in the last consecutive sera. A. fumigatus species complex was isolated from the materials. The fungus was resistant to L-AmB (Table 1). The patient eventually died in intensive care.
Discussion
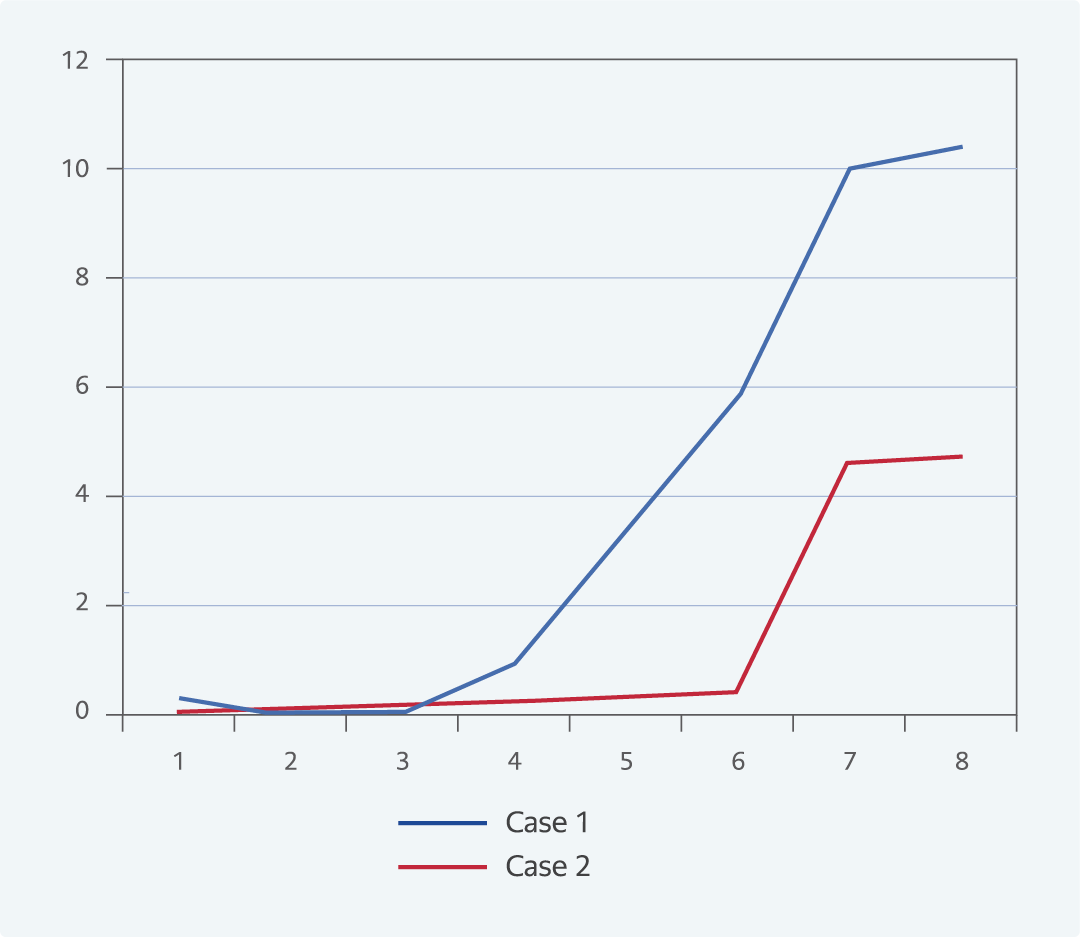
The definitive diagnosis of IA is quite difficult and is generally based on histopathological demonstration of the organism in tissue or fungal staining and/or culture of Aspergillus spp. (7, 8). In our cases, the A. flavus species complex was recovered from ETA and the A. fumigatus species complex from a skin biopsy. Both Aspergillus spp. were identified with conventional methods and MALDI-TOF MS (score >2). In clinical practice, the diagnosis of IA is usually made with appropriate radiological studies and diagnostic biomarkers in blood. GM is a non-invasive diagnostic test for IA. Although false-negative and false-positive results for serum GM have been reported in immunocompromised hosts, serum GM is useful in diagnosing IA with a sensitivity of 70%, and it can be used in combination with clinical, radiographic and bi-weekly screening of serum GM (8, 9). Initially, serum GM tests were negative in the patients. The radiological results of two patients were compatible with IPA, and the GM levels of the cases increased rapidly on routine blood screening during treatment with L-AmB (Figure 4).
Antifungal drug resistance is not as much of a concern as resistance to antibacterial agents; however, there has been an increase in the number of case series of both primary and secondary resistance in human mycoses (5, 10). L-AmB is a broad-spectrum antifungal active against molds and yeasts; some species, such as Aspergillus terreus and Aspergillus lentulus, are intrinsically resistant to AmB. This drug binds irreversibly to ergosterol in the fungal cell membrane, forming pores. This leads to a disruption of the proton gradient and, ultimately, to fungal cell death. Some researchers suggest that overuse of AmB against fungal infections leads to the emergence of less susceptible species, such as A. terreus and A. flavus (11). Resistance to AmB is quite rare; fungi can gain resistance to AmB by reducing the amount of ergosterol in the plasma membrane or changing the target lipid (12). The problem with in vitro susceptibility testing for AmB is the lack of reliable susceptibility breakpoints for Aspergillus spp. Susceptibility breakpoints to AmB are ≤1 mg/L for Aspergillus niger and A. fumigatus using the European Committee on Antimicrobial Susceptibility Testing (EUCAST) method. It has not been defined for A. flavus and A. terreus (12). Epidemiological cut-off (ECOFF) values for these species are generally one step higher than for A. fumigatus (13). Our patients did not improve under L-AmB; on the contrary, they worsened clinically and radiologically, and both Aspergillus spp. were resistant to AmB.
L-AMB is a potent antifungal; its resistance is common in A. terreus and, to some extent, in A. flavus (14, 15). AmB resistance has rarely been reported in clinical practice and environmental A. fumigatus samples. In a study, A. flavus isolates showed high minimum inhibitory concentration (MIC) values to AmB, with 81% of the isolates having MIC values ≥ 2 mg/L and resistance to AmB was found to be lower in A. fumigatus (14). Worldwide, resistance to AmB varies in A. fumigatus isolates. In a study, none of the 156 clinical isolates they tested were resistant to AmB (15). In Brazil, the highest percentage of AmB-resistant A. fumigatus has been reported, with 27.4% of the isolates having MIC values ≥ 2 mg/L (14).
In our cases, antibiotic susceptibilities and identification were determined by using the broth microdilution method according to EUCAST (16). The results were interpreted with ECOFF values. As controls, strains of Candida parapsilosis ATCC 22019 and Candida krusei ATCC 6258 were used. However, there are some limitations on the identification of the species. For cryptogenic Aspergillus isolates, sequencing and, if possible, whole genome analysis to investigate possible resistance mechanisms would make study results more meaningful. Unfortunately, these could not be carried out because financial support could not be found.
In conclusion, aspergillus infection should be considered in the preliminary diagnosis of in immunocompromised hosts who do not respond to antimicrobial treatment. Mycological and serological investigations should follow this. Early diagnosis allows rapid initiation of treatment, improving prognosis. Thereafter, resistant fungal strains should be considered in patients who do not respond to antifungal therapy. More data are needed to plan the treatment strategy for these individuals.