Introduction
Infective endocarditis is the infection of the endocardial surfaces of the heart, including native valves, mural endocardium, or septal defects. Involvement of previously implanted prosthetic valves, intracardiac devices, or pacemakers are commonly predisposing risk factors for infective endocarditis. If left untreated, it is inevitably fatal due to complications such as congestive heart failure, stroke, embolic events, and cardiac abscess. Therefore, rapid diagnosis of the disease, determination, and treatment of the causative agents are of critical importance (1).
Pseudomonas stutzeri is a gram-negative, rod-shaped, aerobic, catalase, and oxidase-positive bacterium found in soil and water. Unlike the widely known organisms that are often isolated, P. stutzeri is rarely identified as the causative agent of nosocomial and community-acquired infections. Patients with P. stutzeri infection usually have predisposing risk factors such as immunosuppression or a history of recent surgery. However, most patients respond successfully to antibiotic therapy, reflecting this organism’s relatively low degree of virulence (2). This case report presents a patient with a history of the Benthall-DeBono procedure, a cardiac surgery involving composite graft replacement of the aortic valve, aortic root, and ascending aorta, and graft reimplantation of the coronary arteries, who was reoperated for late endocarditis due to P. stutzeri.
Case
A 55-year-old female patient was admitted with complaints of weakness, loss of appetite, fever, and progressive dyspnea. She had a history of the Benthall-DeBono procedure due to bicuspid aortic valve stenosis and aortic aneurysm eight years ago. The patient also had sarcoidosis and Crohn’s disease. She was using methotrexate 6×2.5 mg PO per week and 64 mg/daily methylprednisolone. On admission, she had a temperature of 38.5 °C, her blood pressure was 135/85 mmHg, and her pulse rate was 82/min. On the physical examination, there was a 2/6 diastolic murmur in the aortic area of the heart. In blood tests, white blood cell (WBC) 16,000 mm3 (82% neutrophil, 16% lymphocyte), hemoglobin 11.4 g/dL, C-reactive protein (CRP) 88 mg/L, sedimentation rate 39 mm/h, troponin 0.01 ng/mL were detected. Three sets of blood cultures were taken at the admission.
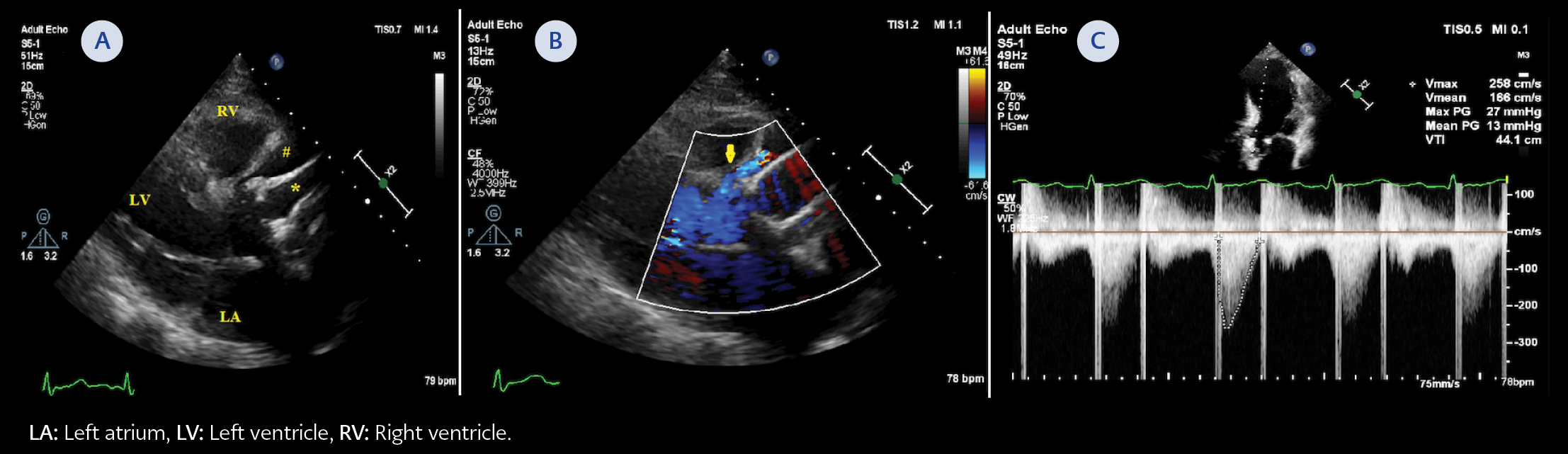
Figure 1. Transthoracic echocardiography showed that sol ventricle systolic function was normal, dehiscence of the aortic valved conduit (*), periaortic pseudoaneurysm (#) (A) and early diastolic severe aortic insufficiency (B). Transvalvular gradients of the mechanical aortic valve were 27/13 mmHg, Doppler examination showed early diastolic severe periaortic insufficiency (yellow arrow, part B), and pressure half time was 180 ms (C).
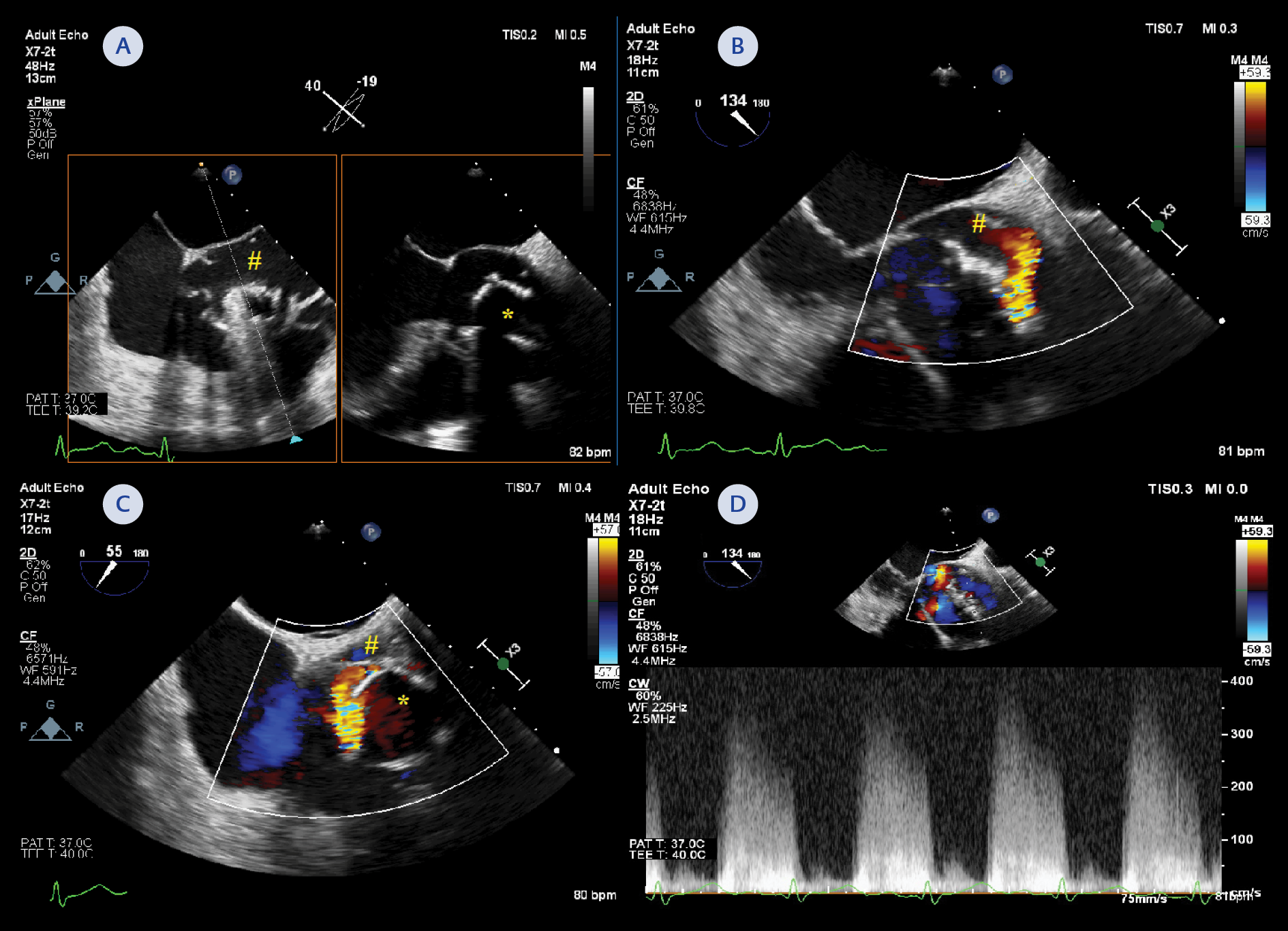
Figure 2. Two-dimensional transesophageal echocardiography with biplane examination revealed that dehiscence of the aortic valve conduit (*), periaortic large pseudoaneurysm (#) (A). Color Doppler examination showed that the posteromedial of the distal anastomosis of the conduit were impaired and there was anastomotic leakage in diastole from that region to the periaortic region and severe paravalvular aortic insufficiency (Part B, C, and D).
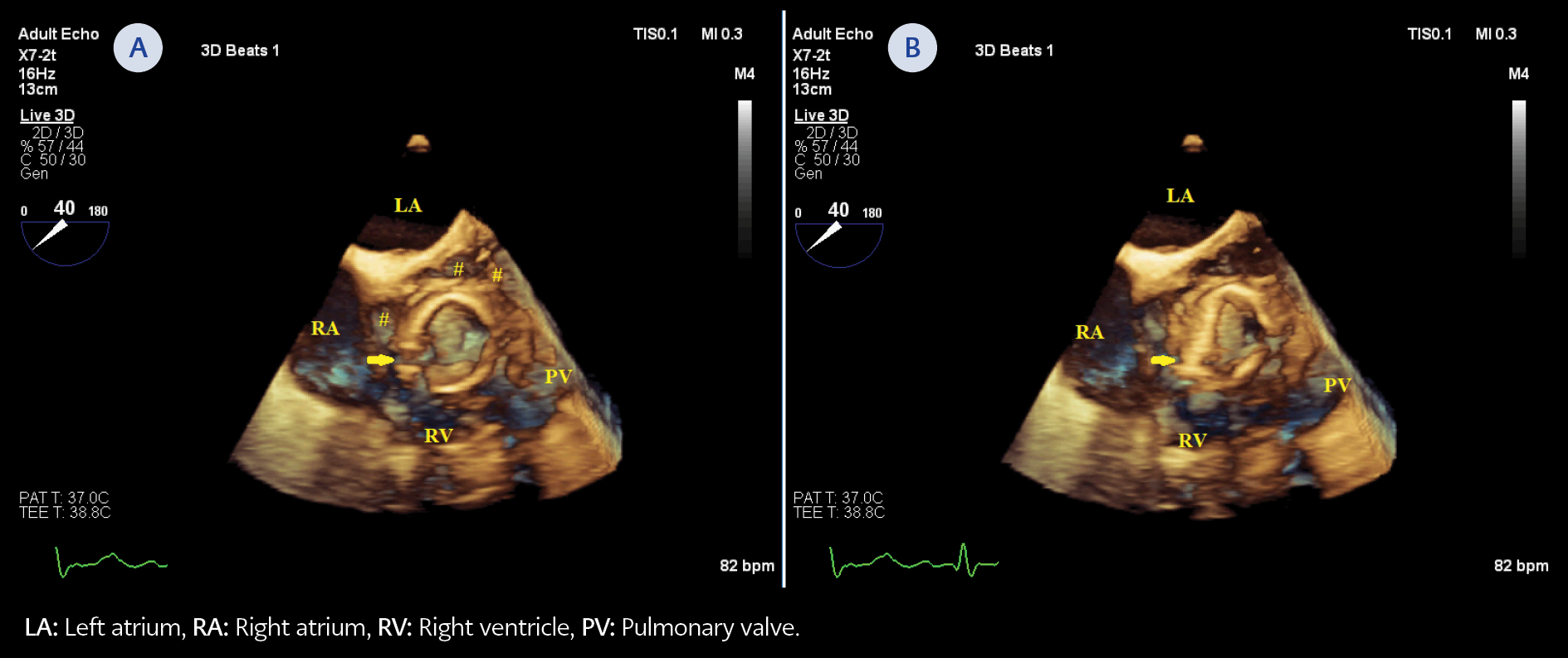
Figure 3. Three-dimensional transesophageal echocardiography showed that dehiscence of the aortic valve conduit (*), large pseudoaneurysm (#), the systolic collapse of the conduit and the posteromedial of the distal anastomosis of the conduit were impaired (yellow arrow). Part A) Diastolic frame and Part B) systolic frame of the heart cycle.
There was no history of dental or interventional procedures, animal contact, drug usage, or travel. Serological testing for human immunodeficiency virus infection was negative. Transthoracic echocardiography revealed that the Benthall graft was separated almost 360 degrees from the aorta, dehiscence of the aortic valved conduit, and periaortic large pseudoaneurysm (Figures 1 and 2). No vegetations or thrombus were identified on the valve, and transvalvular gradients were 27/13 mmHg. On transesophageal echocardiography, the posteromedial of the distal anastomosis of the conduit was impaired, and there was an anastomotic leakage in diastole from that region to the periaortic region and severe paravalvular aortic insufficiency (Figure 2B, 2C and 3). These signs were confirmed by computed tomography aortography, and the distal ascending aorta’s diameter was 4.03 cm.
Based on the modified Duke criteria (3), the case’s findings met two major and two minor criteria: repeatedly positive blood cultures for P. stutzeri, echocardiography findings consistent with endocarditis, and the presence of a predisposing condition (prosthetic valve) to infective endocarditis and fever. Following the diagnosis of definitive infective endocarditis, empirical antibiotics for prosthetic valve endocarditis were initiated (vancomycin 1 g twice a day and ceftriaxone 2 g once a day, intravenous).
Since P. stutzeri was grown in the blood cultures taken on admission and on the third day of the treatment, the therapy was modified to ceftazidime 2 g three times a day. Blood cultures were evaluated using BACTECTM FX (Becton Dickinson and Company, USA), and the antibiotic susceptibility tests for positive cultures were performed according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST). Bacterial identification was performed using the VITEK® 2 system (bioMérieux Inc., France). In the antibiogram, ciprofloxacin, gentamicin, ceftazidime, and piperacillin were detected as sensitive, meropenem as intermediate sensitive, and imipenem as resistant. There was no growth in blood cultures taken on the second day after ceftazidime treatment.
After ten days of antibiotic and diuretic therapy, cardiac surgery was done due to complicated infective endocarditis. Intraoperatively, small vegetations were visible, which attached to the inner wall in the distal part of the graft. There was no visible vegetation on the prosthetic aortic valve, and its leaflet movements were normal. The aneurysmatic segment of the distal ascending aorta was resected, and a redo Benthall procedure was performed. The same microorganism was isolated in the culture growths planted from the vegetation material in the resected old graft. No embolic events were detected during her hospitalization. Antibiotherapy was completed in six weeks, and the patient was discharged with recovery.
Discussion
Endocarditis is still a major cardiac problem in terms of mortality and morbidity, necessitating urgent medical intervention. While most patients recover with antibiotic treatment alone, surgical procedures are sometimes required. We presented an endocarditis case caused by P. stutzeri, which was treated surgically and medically. The isolation of P. stutzeri, widely distributed in the environment, is usually considered as colonization or contamination. However, infections caused by P. stutzeri, especially endocarditis, are rare (4).
Ten cases have been reported in the literature since 1987, when the first case was presented (5-14). The first case was mitral bioprosthetic valve endocarditis two years after cardiac surgery and recovered with antibiotherapy (5). Lopez et al. reported a case of prosthetic aortic valve endocarditis in 2002, which was treated with antibiotics and surgery (6). Grimaldi et al. reported a prosthetic aortic valve abscess because of P. stutzeri six years after the surgery; a few months later, pulmonary sarcoidosis was diagnosed, and prednisolone was given. After four years following the treatment, recurrent endocarditis developed with the same agent (7). The first case reported as native valve endocarditis at the age of 91 was successfully discharged with medical treatment (9). In 2018, Halabi et al. presented early endocarditis with P. stutzeri detected on the 26th postoperative day of aortic valve operation, but the patient died despite aortic and tricuspid valve replacement and medical therapy (10).
Five of the seven cases reported in the literature so far have been seen in the prosthetic valve, and six were in the aortic valve. Prosthetic valve endocarditis caused by P. stutzeri seems to have an indolent course that typically occurs years after cardiac surgery. Five cases were treated both surgically and medically. Only one case died due to recurrent endocarditis after surgery in the early period. While tobramycin, mezlocillin, aztreonam, cefotaxime, ceftriaxone, and ciprofloxacin were preferred in the treatment of the patients, ceftazidime was used in the last two cases, as we did (10-11).
Non-antipseudomonal antibiotics such as cefotaxime and ceftriaxone were used empirically in the cases in the literature, and treatment was initiated after bacterial growth. Antimicrobial resistance is not as frequent among P. stutzeri isolates compared with Pseudomonas aeruginosa isolates. Many
P. stutzeri strains are susceptible to quinolones; extended-spectrum penicillins, with and without β-lactamase inhibitors; and carbapenems, unless it was acquired from the hospital. In our case, it was determined to be sensitive to all antibiotics except carbapenems.
A literature review (8) suggests that P. stutzeri may occur more frequently in Israel and other countries of the Mediterranean, a statement that seems consistent with the given previous cases and ours. Our case is similar to previous cases regarding aortic involvement and valve replacement history. Furthermore, our patient’s history of underlying immunosuppressive conditions such as sarcoidosis and Crohn’s disease may have played a predisposition role for endocarditis with this microorganism. In most cases, in addition to a history of previous surgery, some conditions may have caused immunosuppression, such as age, transplantation, and underlying autoimmune disease. Most cases were observed in the late period after surgery and were community-acquired.
P. stutzeri may rarely be the pathogen microorganism of infective endocarditis and usually causes late prosthetic valve endocarditis years after cardiac surgery. Because of its susceptibility to a wide array of antibiotics, a good response to treatment can be achieved. To obtain full recovery in these patients, besides medical therapy, early surgical intervention seems to have a place. Additional studies are needed to find out the route of the bacteria acquisition and the source of bacteremia among cases of community-acquired prosthetic valve endocarditis caused by P. stutzeri.