Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a strain of the coronavirus that causes COVID-19, spread rapidly around the world and was defined as a pandemic on March 12, 2020, by the World Health Organization (1). As of June 2023, more than 767 million cases were confirmed globally, along with 6.9 million deaths (2). Human immunodeficiency virus (HIV) is one of the diseases that threaten human life and is widespread all over the world. As of 2022, 39 million people were living with HIV in the world (3). There are 34,453 people living with HIV (PLWH) in Turkey, and the number of newly diagnosed individuals is increasing (4). PLWH are at risk for potentially worse COVID-19 outcomes due to underlying immunosuppression (5). In addition, the COVID-19 pandemic disrupted HIV control and prevention efforts, especially in low-income countries (6).
The clinical spectrum of COVID-19 is broad; while most patients develop only mild symptoms such as nasal congestion, loss of taste and smell, or arthralgia, especially in the early phase of illness, some patients have severe disease that requires hospitalization and oxygen support, even admission to an intensive care unit (7). Recent studies have suggested that patients with comorbidities, such as hypertension, obesity, immunocompromised status, and diabetes, are more likely to have worse outcomes (8).
PLWH might be at an increased risk of severe COVID-19, especially in patients with comorbidities, having lower CD4+ T cell counts and unsuppressed HIV RNA values, and not taking antiretroviral therapy (ART) (9). Although there are many studies on HIV and COVID-19 co-infection, published data that examine COVID-19 vaccines in PLWH is limited (10). Our country had an inactivated coronavirus vaccine (CoronaVac®; Sinovac Biotech, China) and a mRNA vaccine (Comirnaty®; Pfizer-BioNTech) in the study period. In this study, we aimed to investigate the impact of vaccination preferences and vaccination rates on the severity of COVID-19 in patients with HIV co-infection.
Materials and Methods
PLWH who were followed by Kocaeli Outpatient HIV Clinic and on ART during the COVID-19 pandemic (January 2020- December 2022) were retrospectively included in the study. Patients who received at least two doses of the COVID-19 vaccine and whose second dose was at least one month before were accepted as fully vaccinated. Diagnosis of COVID-19 was made using real-time reverse transcriptase-polymerase chain reaction (rRT-PCR) to detect SARS-CoV-2 RNA positivity in nasopharyngeal swab specimens. Patients requiring hospital admission were classified as severe. The patient’s demographics and vaccination status were collected from the hospital data system.
The Ethics Committee of Kocaeli University approved the study with the protocol number GOKAEK-2023/08.20.
Statistical Analysis
The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 20.0 (IBM Corp., Armonk, NY, USA). The statistical significance was set as p <0.05. The data were interpreted according to means and percentages. The Kolmogorov-Smirnov test was used to evaluate the normal distribution of investigated parameters. The differences were compared using the Mann-Whitney U and Wilcoxon tests.
Results
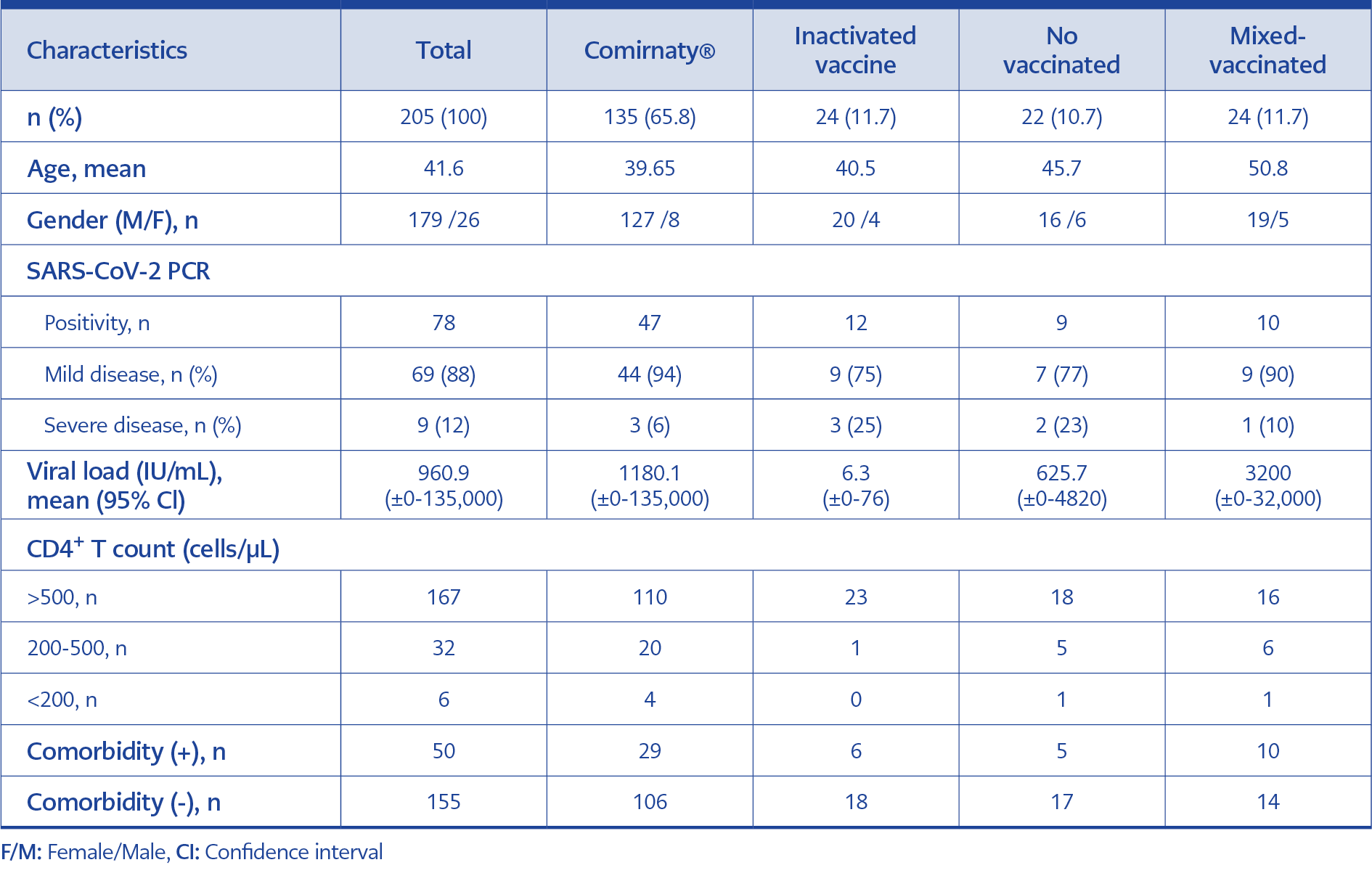
A total of 205 patients receiving ART were included in the study, 179 of whom were male and had a mean age of 42. The HIV RNA of 182 patients was negative, and CD4+ T cell counts were above 200 in 199 patients. Patients were aware of their HIV status for a mean of five (1-16) years. The demographics and laboratory findings of the patients are shown in Table 1.
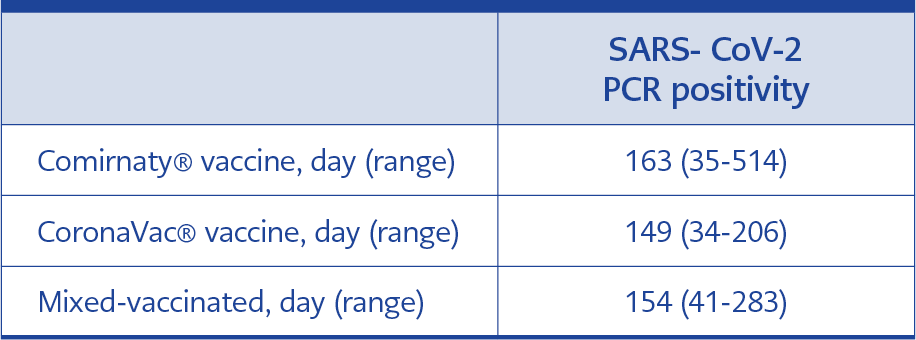
Of all patients, 135 (65.8%) were vaccinated with the Comirnaty® vaccine and 24 (11.7%) with the CoronaVac® vaccine (11.7%). While 24 (11.7%) patients had mixed immunization, 22 (10.7%) were unvaccinated. In the Comirnaty® vaccinated group, 47/135 (35%) patients had COVID-19 at least one month after the second dose; 12/24 (50%) patients in the CoronaVac® group, and 10/24 (42%) patients in the mixed vaccinated group had COVID-19 disease after the second dose. COVID-19 infection rate was 41% (9/22) among unvaccinated patients. The time between the vaccination and PCR positivity is shown in Table 2. The mean day counts between the last vaccine date and SARS-CoV-2 PCR positivity date were 163 in the Comirnaty® group, 149 in the CoronaVac® group, and 154 in the mixed vaccinated group.
There were 78 patients with PCR-confirmed COVID-19; 69 (88%) of them had mild disease, eight were admitted to clinics, and one was admitted to the intensive care unit due to hypoxia. Of 9 patients with severe disease, three had received the
CoronaVac® vaccine, three had received the
Comirnaty® vaccine, one had had the mixed immunization, and two were unvaccinated. The one patient who died had received the mixed immunization and had a positive HIV RNA value and a low CD4+ T cell count. On the other hand, seven patients with severe diseases had negative HIV RNA values.
Discussion
Data on the effect of COVID-19 vaccines in PLWH are limited. In a review comparing vaccine responses in PLWH and people living without HIV, Jin et al. stated that protection after the second dose was lower in PLWH but similar after the first dose (11). In a meta-analysis including 44 studies and approximately 38,971,065 COVID-19 patients conducted in Belgium, co-infection prevalence was found to be 2.96%. In PLWH, rates of severe COVID-19 ranged from 11% to 28.7% (12). In our study, this rate was %11.5. This low rate may be due to patients receiving ART regularly and having a CD4+ T cell count above 200. Basoulis et al. indicated that the immunological and virological status in PLWH is related to the severity of COVID-19 (5).
In our study, we found that the rate of severe COVID-19 (12%) and COVID-19-related mortality rates (1.28%) were similar between in PLWH with well-controlled HIV infection and in people living without HIV. Our findings showed that PLWH with COVID-19 had mostly mild symptoms. Similarly, Gatechompol et al. found that there were no differences in the clinical presentations, outcomes, morbidity, and mortality between individuals who had SARS-CoV-2 with or without HIV infection (13). However, Danwang et al. said that co-infection with HIV was associated with an increased risk of hospital admission in people with COVID-19 before vaccines (8). We found that those vaccinated with the Comirnaty® got over COVID-19 with statistically significant mild symptoms. In Lang et al.’s study, breakthrough infection was most frequently observed after the Johnson&Johnson vaccine, compared to Pfizer-BioNTech and Moderna vaccines (14). Although we found the rate of both COVID-19 and severe COVID-19 were lower among patients vaccinated with the Comirnaty® vaccine, it was difficult to reach a definitive conclusion with our findings. Our study did not include some factors that could contribute to the immunity, such as previous undiagnosed or diagnosed COVID-19 episodes and details of comorbidities.
The longest time between the new COVID-19 infection and the last vaccine dose was in the Comirnaty® vaccine arm in our study. In another study, Israel et al. evaluated 33,993 people who had received at least two doses of the Comirnaty® vaccine, and they found that a new COVID-19 infection was seen on average 146 days after the second vaccine, the period gradually shortening over the age of 60 (15). A study investigating the impact of vaccination type on new COVID-19 infections in the United Kingdom associated the new infections after vaccines with a cycle threshold (CT) value above 30 and a decrease in symptoms; however, there was no statistically significant difference in effectiveness between Comirnaty® and AstraZeneca vaccines (16).
Vaccines against SARS-CoV-2 had a significant impact on decreasing rates of new cases and controlling the pandemic, particularly for populations at high risk. Although it varies according to the variants, the efficacy of the inactivated vaccine and Comirnaty® was found to be 60% and 90%, respectively (17). It was reported that the seropositivity rate was low after the first dose of the vaccines in the immunosuppressive patient group; still, in a meta-analysis including four studies on PLWH, three studies reported that the response occurred at the same rate as immunocompetent patients after the first dose (10). Several studies demonstrated that the seropositivity of both the primary and booster vaccinations was similar in people living with or without HIV, especially when CD4+ T cell counts were well preserved (18, 19).
Our study has some limitations. The patient number was small, and there was no control group. The distribution of age, gender, and comorbidities was similar in both vaccine arms, but more patients were in the Comirnaty® vaccine arm. In conclusion, the course and the outcomes of COVID-19 among SARS-CoV-2 vaccinated PLWH, especially with well-controlled HIV infection seem to be similar to people living without HIV. Future studies on post-vaccine breakthrough infections among PLHW should be conducted to contribute to COVID-19 vaccine guidelines.