Introduction
Chronic hepatitis B (CHB) infection is a global health problem that the World Health Organization (WHO) reported 296 million individuals diagnosed with CHB, and 820,000 died worldwide in 2019 (1, 2). In our country, as per the Türkiye Viral Hepatitis Prevention and Control Program for 2018-2023, there have been 3.3 million patients with CHB infection in Türkiye (3). According to the WHO’s report, up to 40% of individuals with CHB may develop cirrhosis or liver cancer (1).
The clinical manifestations of hepatitis B virus (HBV) infection vary widely, from inactive hepatitis B to advanced cirrhosis (4). Chronic HBV infection is classified into five clinical groups according to the assessments of hepatitis B e-antigen (HBeAg), alanine aminotransferase (ALT), and HBV-DNA values (5, 6). It is crucial to evaluate disease activity and progression for the management of chronic HBV infection, and antiviral therapy is recommended for those with significant fibrosis (6-8).
In Türkiye, health insurance has covered antivirals in patients with cirrhosis or any contraindications for biopsy. Based on the Turkish Social Security Institution Healthcare Implementation Communique criteria, antiviral treatment cannot be started on hepatitis B patients without showing fibrosis in the liver biopsy (9). Therefore, liver biopsy is often performed in patients with an indication. As a result, centers following patients living with HBV in Türkiye have a large number of liver histopathology results in chronic hepatitis B.
On the other hand, in patients with low fibrosis levels based on liver biopsy results, treatment is not initiated. This may cause an unnecessary invasive procedure. Therefore, it is crucial to evaluate liver fibrosis with non-invasive methods. Although there are some scoring systems for predicting cirrhosis such as fibrosis-4 (FIB-4) and aspartate aminotransferase to platelet ratio index (APRI), they do not have sufficient sensitivity and specificity to indicate fibrosis.
In this study, we aimed to determine the predictors for significant hepatic abnormality (SHA), a treatment indication, by assessing demographic, laboratory, and radiological results of chronic hepatitis B (CHB) patients who underwent liver biopsy.
Materials and Methods
In this retrospective study, individuals with untreated HBeAg-negative CHB infection from Haseki Training and Research Hospital were enrolled from January 2015 to December 2022. A total of 731 patients who tested positive for HBsAg during that period were included. Exclusion criteria comprised individuals with significant alcohol consumption, monogenic hereditary disorders, co-infections with human immunodeficiency virus, hepatitis D, and hepatitis C viruses, as well as patients with a history of prior antiviral therapy for HBV infection.
Four patients with HCV co-infection, three with HIV co-infection, four with malignancy, 21 with insufficient data, 81 identified as HBeAg-positive, and 52 with unavailable HBeAg records were excluded. The final cohort consisted of 566 treatment-naïve patients with HBeAg-negative CHB infection, aged 18 years and older, who underwent liver biopsy after a minimum 6-month follow-up period.
Demographic characteristics (such as gender, age), laboratory findings (hemoglobin, platelet, aspartate aminotransferase [AST], ALT, total bilirubin, HDL and LDL cholesterol, triglycerides, fasting blood glucose, international normalized ratio [INR], alpha-fetoprotein, albumin), virological parameters (HBV-DNA), and liver biopsy findings were collected from patients’ medical charts.
In our center, Ishak’s scoring and Knodell’s histological activity index (HAI) were used to evaluate fibrosis and necroinflammation (10). In determining the indication for antiviral treatment, histopathological evaluation of the liver was taken into account following the requirement of the Turkish Social Security Institution Healthcare Implementation Communique. Therefore, in histopathology, SHA was defined as stage ≥2 fibrosis, grade≥ 6 necroinflammation, or both in patients.
All protocols adhered to the ethical guidelines outlined in the Declaration of Helsinki. The Ethics Committee of Haseki Training and Research Hospital approved the study on August 8, 2023, with decision number 143-2023. Considering the retrospective nature of the research, the informed consent requirement was waived.
Statistical Analysis
The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 15.0 (IBM Corp., Armonk, NY, USA). Categorical variables were presented as frequencies (n) and percentages (%), whereas numerical variables were presented as medians with interquartile ranges (IQR). Group comparisons for rates employed the Chi-square test for categorical variables. Two independent groups were compared using the Student t-test and Mann-Whitney U test. The statistical significance was set at p<0.05. Multivariate analysis modeling was conducted with parameters identified as predictors for SHA in univariate analysis. After performing correlation analysis, the parameters for modeling were selected. Optimal threshold levels for serum ALT, AST, and HBV-DNA, with corresponding sensitivity and specificity for predicting SHA in patients with chronic hepatitis B, were determined based on receiver operating characteristic (ROC) curve analysis.
Results
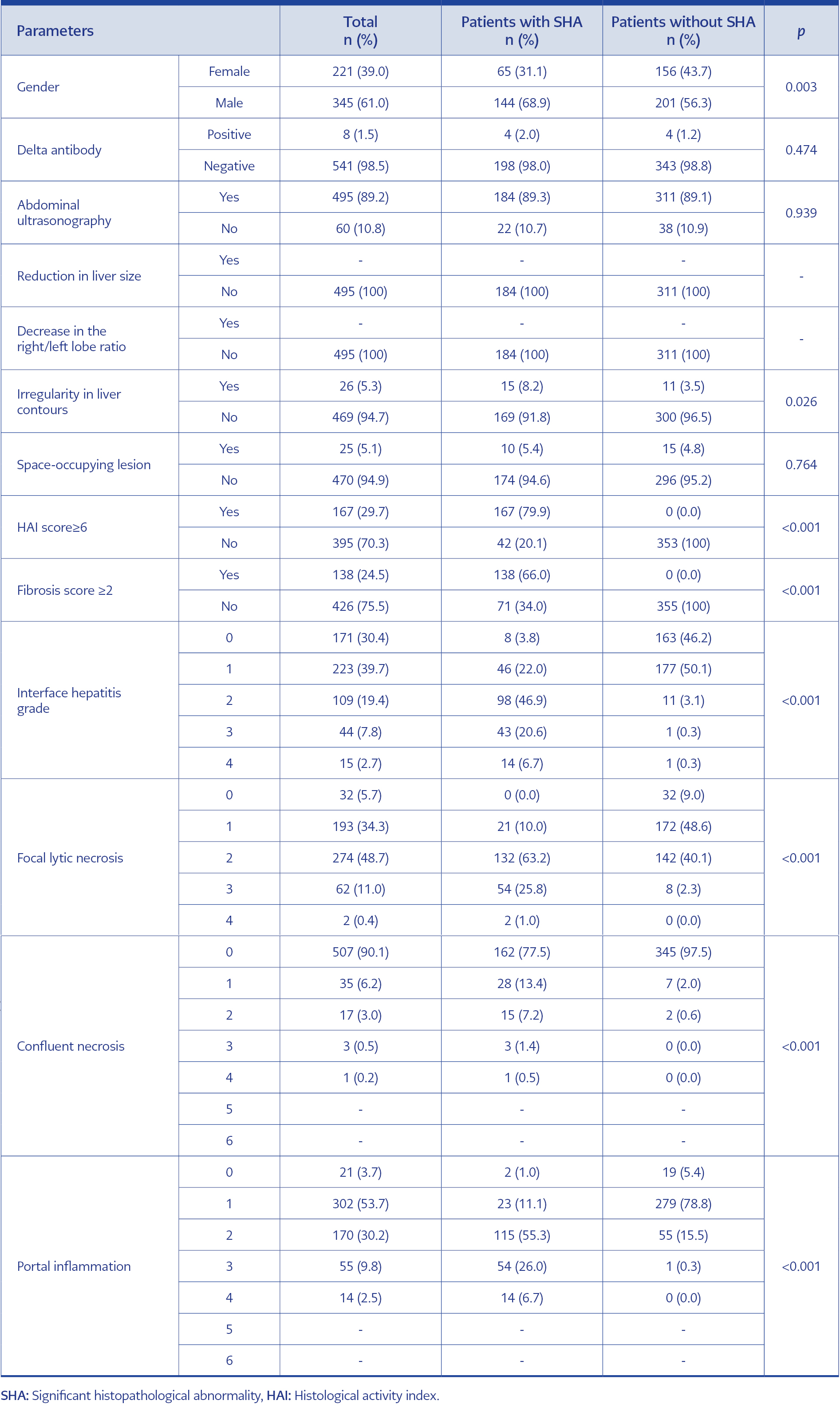
Table 1. Comparison of radiological and histopathological findings in patients with and without significant histopathological abnormality (SHA).
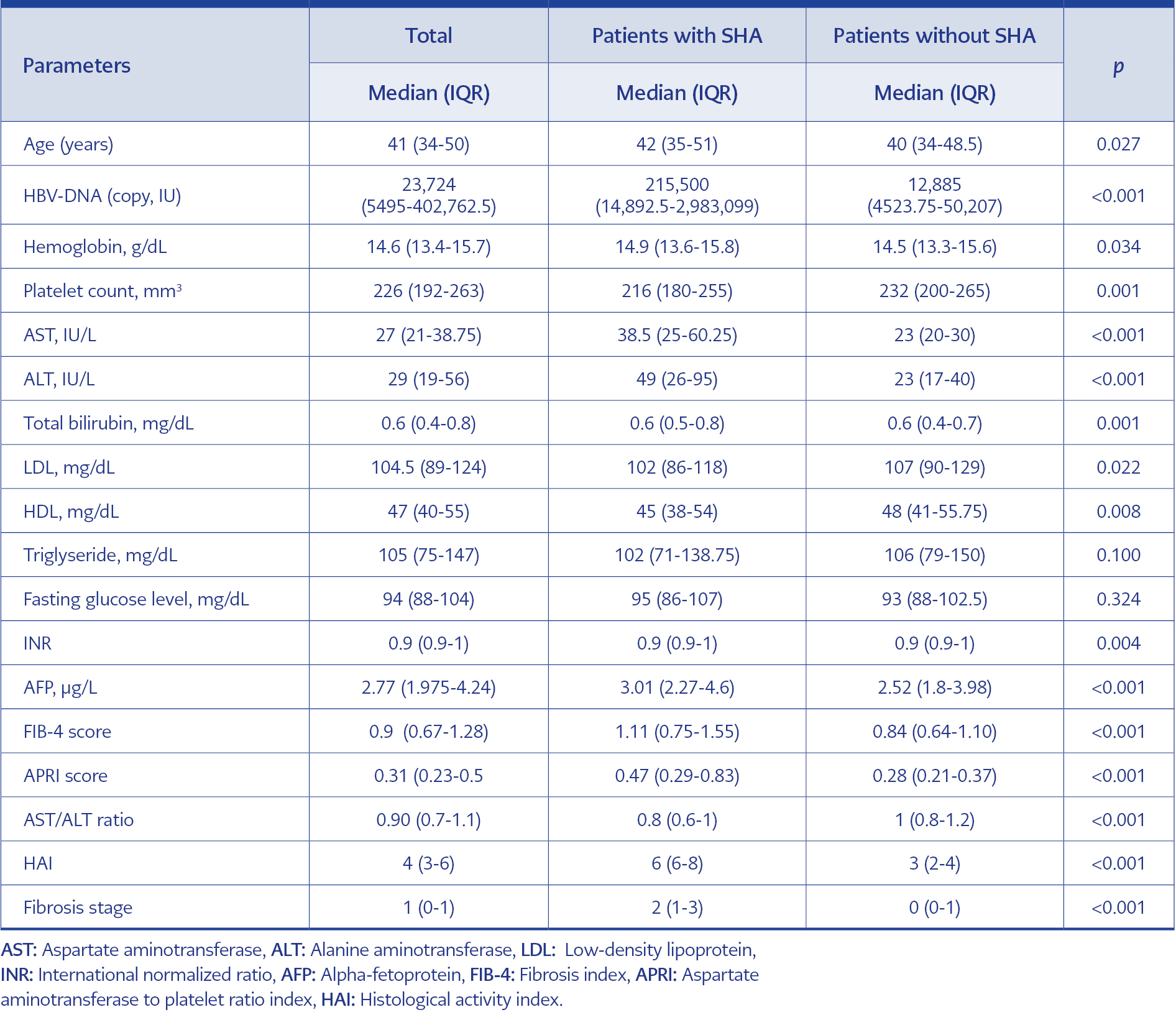
Table 2. Comparison of laboratory parameters in patients with and without significant histopathological abnormality.
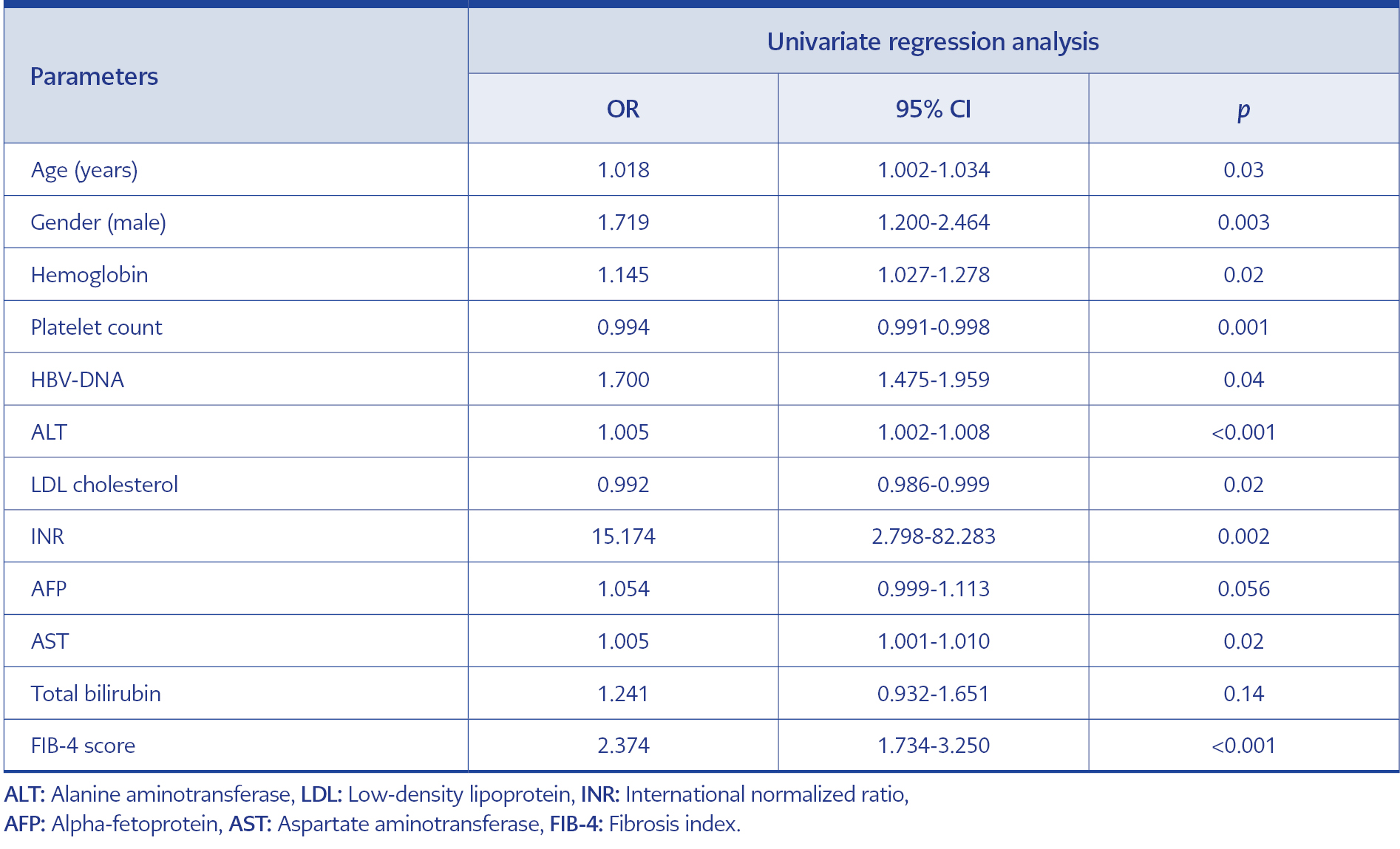
Table 3. Univariate regression analysis for predicting significant histopathological abnormality in patients with HBeAg-negative chronic hepatitis B.
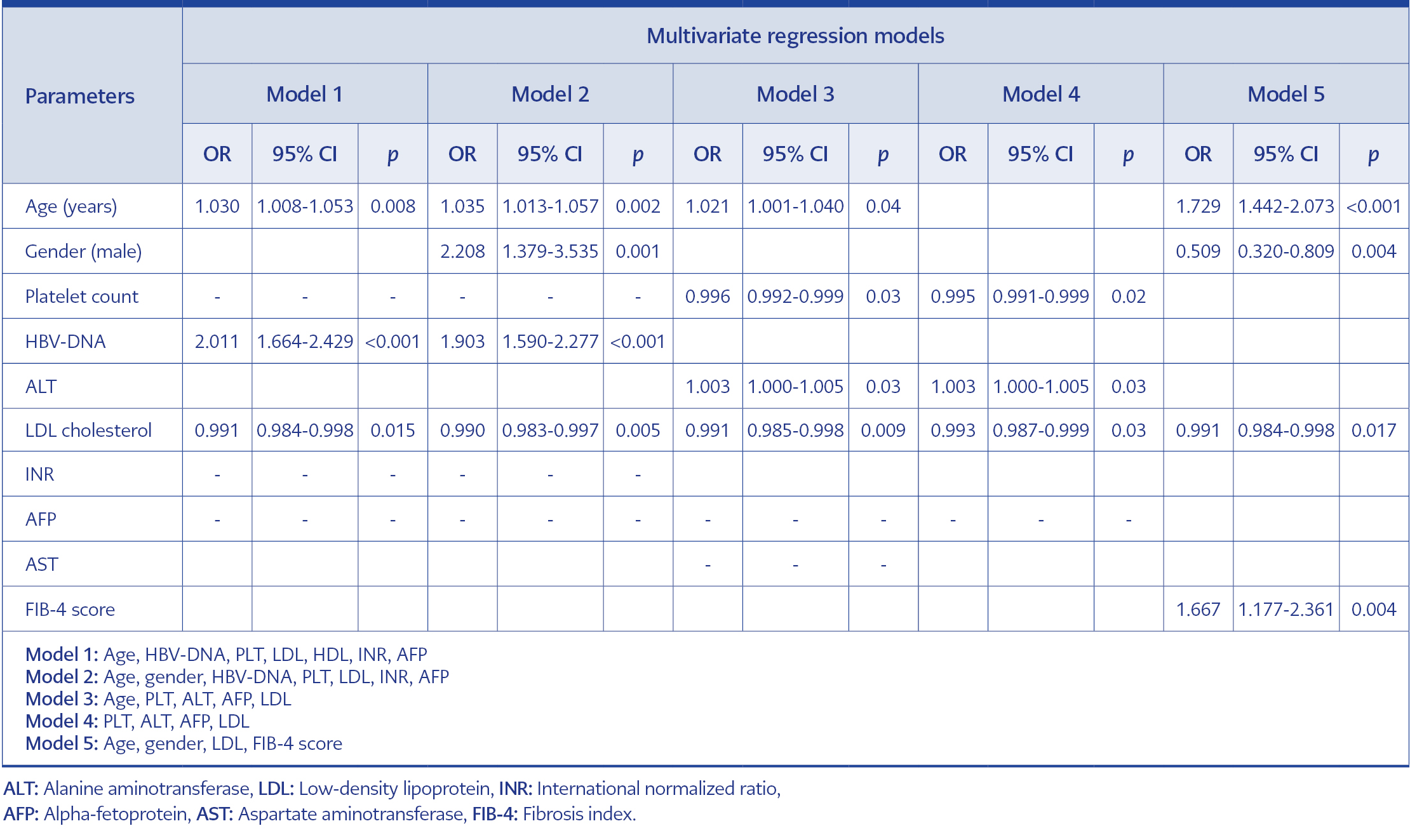
Table 4. Multivariate regression models for predicting significant histopathological abnormality in patients with HBeAg-negative chronic hepatitis B.
The research involved 566 patients diagnosed with untreated CHB. Within the cohort, 61% (345/566) were male, and the median age was 41 years, with an IQR of 34-50 years. The median HBV-DNA level was 23,724 IU/mL, ranging from 5495 to 402,762.5 IU/mL. Notably, 24.5% (138/566) of patients had a fibrosis score of ≥2,29.7% (167/566) had a HAI score of ≥6, and 36.9% (209/566) had SHA (Table 1). Patients with SHA were found to be older than those without SHA, with a median age of 42 years compared to 40 years (p=0.027). Patients with SHA also displayed lower median platelet count (p=0.001) and HDL levels (p=0.008) while having higher levels of HBV-DNA (p<0.001), ALT (p<0.001), AST (p<0.001), hemoglobin (p=0.014), LDL (p=0.022), total bilirubin (p=0.006), INR (p=0.004), alpha-fetoprotein (p<0.001), FIB-4 score (p<0.001), APRI score (p<0.001), and AST/ALT ratio (p<0.001) (Table 2).
In the univariate analysis, factors associated with SHA in CHB patients included age, gender, HBV-DNA, hemoglobin, platelet count, LDL, HDL, INR, alpha-fetoprotein, total bilirubin, and FIB-4 score (Table 3). Multivariate analysis, utilizing different models, identified age, gender, HBV-DNA, LDL, ALT, FIB-4 score, and platelet count as the most reliable predictors for SHA in CHB patients (Table 4).
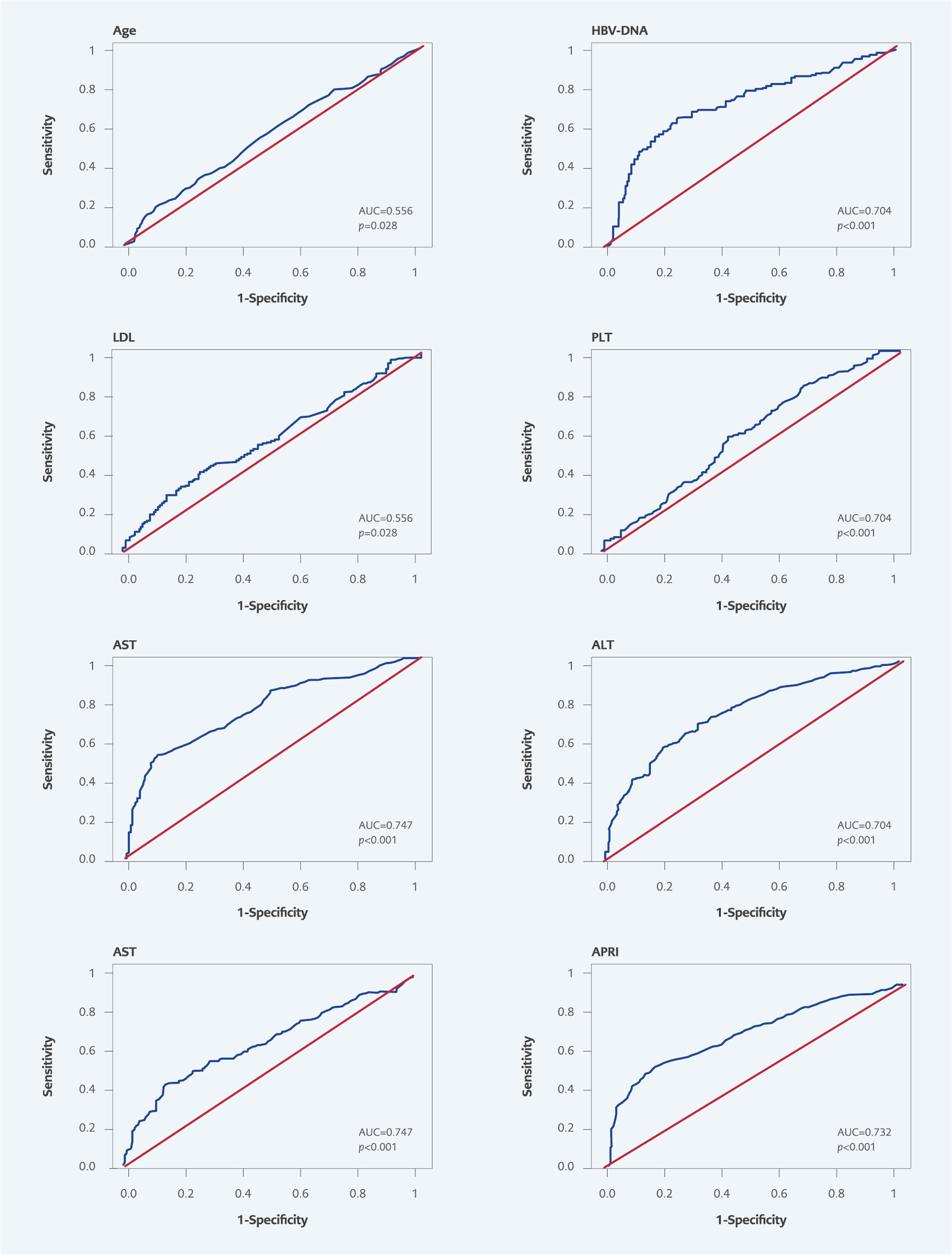
Figure 1. Receiver operating characteristics (ROC) analysis for predicting significant histopathological abnormality in patients with chronic hepatitis B.
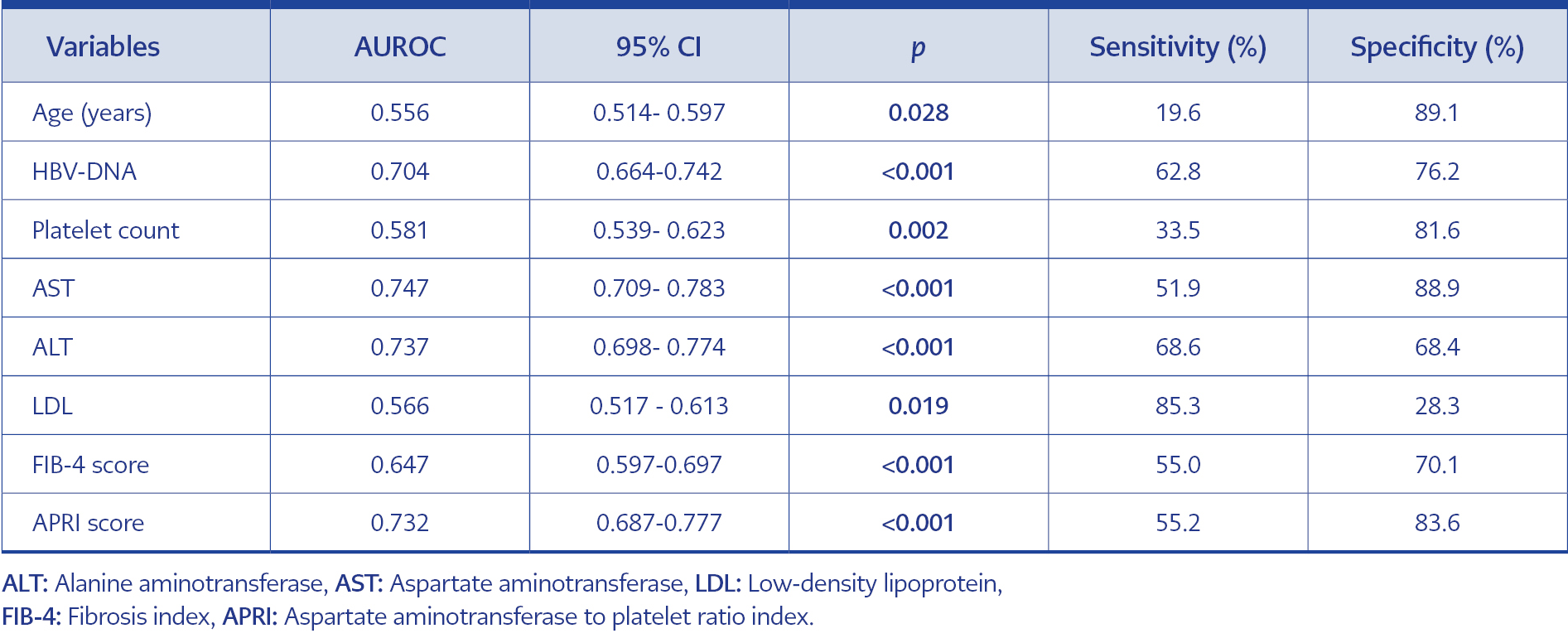
Table 5. Receiver operating characteristic (ROC) curves of laboratory parameters for significant histopathological abnormality in patients with HBeAg-negative chronic chronic hepatitis.
To predict SHA in CHB patients, the area under the ROC curves (AUROC) were generated for various factors, such as age, HBV-DNA, platelet count, AST, ALT, LDL, FIB-4 score, APRI score (Figure 1). The AUROC for all factors was statistically significant (p<0.05) (Table 5). Optimal threshold levels were determined for ALT (32 U/L), AST (37 U/L), and serum HBV-DNA (57,691 IU/mL). Sensitivities and specificities for these factors in predicting SHA were calculated accordingly. According to the ROC curve, for predicting SHA AUROC values of HBV-DNA, AST, ALT, FIB-4 score and APRI score were 0.704 (sensitivity=62.8%, specificity=76.2%; p<0.0001), 0.747 (sensitivity=51.9%, specificity=88.9%; p<0.0001), 0.737 (sensitivity=68.6%, specificity=68.4%; p<0.0001), 0.647 (sensitivity=55.0%, specificity=70.1%; p<0.001), and 0.732 (sensitivity=55.2%, specificity=83.6%; p<0.001), respectively (Figure 1).
Discussion
Our study assessed the demographic, laboratory, and radiological characteristics of 566 patients diagnosed with CHB who underwent liver biopsy. We aimed to retrospectively examine predictive factors for liver fibrosis to indicate the need for treatment. The multivariate analysis identified age, gender, ALT, HBV-DNA, LDL, and platelet counts as significant predictors for detecting SHA in CHB infection. Additionally, ROC analysis revealed that LDL had effects on detecting SHA, and age and AST exhibited the most specific effects.
Comparing our findings with the study conducted by Abdo et al., which explored predictors of significant fibrosis (≥F2 fibrosis), we observed similarities (4). Both studies identified advanced age, increased AST levels, and decreased albumin and platelet count as independent predictors for significant fibrosis. Özdemir et al. also established correlations between HAI score and AST, ALT, and HBV-DNA levels (11). Diktas et al. similarly found correlations between HAI score and AST, ALT, and HBV-DNA in HBeAg-negative CHB patients (12). Our study corroborated some of these associations, with age, HBV-DNA, LDL, and FIB-4 score identified as predictors for SHA in multivariate analysis modeling.
In our study, we determined optimal thresholds for predicting SHA for ALT, AST, and serum HBV-DNA. However, we identified HBV-DNA as a predictor for SHA in multivariate analysis modeling for HBeAg-negative CHB patients. FIB-4 score, a non-invasive method, varied as a predictor of SHA. In different studies in the literature, the FIB-4 score has been determined to be a predictor of SHA (13, 14).
Comparing our findings with Ramírez Mena et al., we determined that an HBV-DNA level above 2000 IU/mL was associated with a roughly 2-fold increased risk for significant liver fibrosis, consistent with their results. Additionally, male gender and increased ALT were independent predictors for SHA in our study, compatible with Ramírez Mena et al.’s findings (15). Similarities were also observed in the study of Wang et al., where male gender and elevated ALT and viral load were independent predictors for liver fibrosis (16). Our study confirmed ALT and HBV-DNA levels as predictors for SHA, and the optimum predictive limits aligned with sensitivity and specificity values.
Seto et al. reported that viral load and platelets, but not ALT, were predictors of significant fibrosis (17). While sharing similarities, our findings indicated that ALT levels remained significant in our study. In Yenilmez et al.’s study, ALT and HBV-DNA levels predicted SHA, similar to our results. However, the HBV-DNA threshold in our study, which includes only HBeAg-negative individuals, was notably lower compared to studies that include HBeAg-positive individuals (18).
Our study determined optimal threshold levels for ALT (32 U/L). In the study of Kang et al., which included 1101 CHB patients, 79.3% of patients with normal ALT (≤40 U/L) levels had significant histological changes in the liver (19). Determining new optimal ALT levels in CHB patients may be considered to detect SHA.The study by Esmaeelzadeh et al. identified AST, ALT, and HBV-DNA as independent indicators of histological grade, with age as the sole predictor for liver fibrosis (20). Our study, evaluating histological grading and fibrosis together, identified age, AST, ALT, and HBV-DNA as predictors for SHA, aligning with similar findings in the literature.
Our study has some limitations. Firstly, it was conducted retrospectively in a single center, so it is not generalizable. Secondly, only one measure of each laboratory test was evaluated. Thus, the fluctuations in laboratory parameters by longitudinal monitoring were not analyzed. Lastly, the biopsy specimens were evaluated by different pathology specialists.
On the other hand, it has some strengths. Firstly, since our center was a tertiary-care research hospital, our sample size was relatively high. Secondly, we included a homogenous study group by excluding HBeAg-positive patients. Thirdly, we included various candidate variables with different models in the multivariate regression analyses.
In conclusion, age, male gender, ALT, AST, HBV-DNA, LDL cholesterol, platelet count, and FIB-4 score were independent predictors of SHA in HBeAg-negative chronic hepatitis B in our study. In descending order, the most sensitive parameters for SHA were LDL and ALT, and the most specific parameters were age, AST, and APRI score. Optimal ALT cut-off values for SHA were determined very close to the upper limit of ALT. Even if ALT values are normal in HBeAg-negative patients, one should remember that SHA may occur in patients with high HBV-DNA levels and not delay antiviral treatment.